Upon presentation to the Wills ER, details of the patient’s recent admission were unavailable. Since she presented with
The patient was started on prednisolone acetate 1% every two hours while awake and cyclopentolate 1% twice daily in both eyes. At follow-up, renal biopsy records were obtained, and she was diagnosed with tubulointerstitial nephritis and uveitis (TINU) syndrome (Figure 1). Her anterior chamber reaction improved, and the topical steroids were tapered within two months. Several weeks after discontinuing her drops, the patient returned to the clinic and was found to have 3+ cell and flare in both eyes. Prednisolone drops were restarted four times daily. Three months later, both anterior chambers were quiet, and there were broken posterior synechiae from 6 to 7 o’clock in the left eye (Figure 2). The remainder of the exam was normal. She was started on a slow topical steroid taper, which she was on at her most recent appointment.
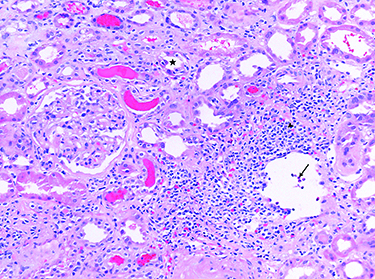 | 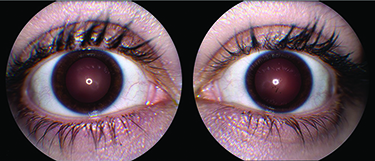 | |
| Figure 1. A representative photomicrograph of a renal biopsy (not from the patient in this report) demonstrating the features of interstitial nephritis. The inflammatory infiltrate is | Figure 2. Anterior segment photos of the right (A) and left (B) eyes. The left eye demonstrates broken posterior synechiae on the anterior lens capsule at 6 to 7 o’clock, but both eyes are white and quiet three months after restarting topical prednisolone acetate 1% to manage a relapse of anterior uveitis. |
During her treatment, the patient’s IOP increased to a maximum of 22 mmHg bilaterally from a baseline of 12 mmHg. She was started on brimonidine tartrate 0.2%/timolol maleate 0.5% drops b.i.d. in each eye, and her IOPs remained controlled over successive follow-up visits.
Discussion
Uveitis is a collection of approximately 30 distinct diseases, all characterized by intraocular inflammation.1 Disease course and management can vary widely by etiology, highlighting the need for an accurate diagnosis.
Uveitis is typically characterized by time course (acute or chronic), laterality, anatomic location (anterior, intermediate or posterior), morphology (e.g.,
Our patient presented with undifferentiated bilateral acute anterior uveitis. The differential diagnosis for anterior uveitis is broad, including, but not limited to, HLA-B27-associated inflammatory bowel disease, psoriatic arthritis, TINU, sarcoidosis, Behçet’s disease, viral etiologies (e.g., herpes simplex or herpes zoster), syphilis, tuberculosis
TINU, which usually occurs in adolescent females, is thought to be an autoimmune disorder, although its mechanism is unknown.3 This disease is rare, representing 0.1 to 2 percent of cases seen in specialty uveitis clinics, although it’s likely underdiagnosed.4
In addition to its low prevalence, making the diagnosis of TINU can be challenging because the signs and symptoms of acute interstitial nephritis are non-specific. In a review of 133 cases of TINU, researchers at Jules Stein Eye Institute at UCLA identified fever (53 percent), weight loss (47 percent), and fatigue/malaise (44 percent) as the three most common presenting symptoms.5 Only 32 percent of patients initially presented with eye pain or redness. Finally, episodes of nephritis don’t usually occur simultaneously with uveitis. In the same review from UCLA, researchers found that only 15 percent of patients presented with concurrent interstitial nephritis and uveitis.5 Twenty-one percent of patients had uveitis that preceded nephritis, and 65 percent had nephritis that preceded uveitis by at least one month, in some cases as much as eight months after the onset of renal disease.
The uveitis associated with TINU is limited to the anterior chamber in 80 percent of cases and is bilateral in 77 percent.6 Posterior involvement, if present, can include mild
TINU may have a genetic predisposition or be associated with certain HLA subtypes, but there’s no consensus to date.4 There is more evidence for an association with certain medications, in particular NSAIDs and antibiotics.5 Interestingly, medications associated with TINU, including cidofovir, rifabutin, sulfonamides
Treatment of the uveitis in TINU most often consists of topical steroids and cycloplegics. Periocular steroid injections have also been used. Systemic steroids have been reported for uveitis alone but are typically reserved for patients with progressive renal failure. In cases in which systemic corticosteroids failed or weren’t tolerated, disease control with immunomodulatory medications such as azathioprine, methotrexate, cyclosporine or mycophenolate mofetil have been reported.5 Our patient has required oral steroids multiple times for control of interstitial nephritis. She experienced a recurrence of uveitis after discontinuing topical steroids, but her ocular inflammation is currently well controlled on prednisolone acetate 1% drops alone.
In conclusion, TINU is an uncommon but likely underdiagnosed cause of bilateral anterior uveitis with systemic manifestations, especially in young females. It’s challenging to diagnose in part due to its rarity, but also because uveitis doesn’t often correlate temporally with nephritis. Thorough history taking is critical to establishing the correct diagnosis. REVIEW
At Wills, Dr. Uhr is in the Department of Medical Education and Dr. Dunn is in the Retina Service. Dr. Palmer is with the Department of Pathology and Laboratory Medicine, University of Pennsylvania Perelman School of Medicine.
1. Jabs DA, Busingye J. Approach to the diagnosis of the uveitides. Am J Ophthalmol 2013;156:2:228-236.
2. González-López JJ, García-Aparicio ÁM, Sánchez-Ponce D, et. al. Development and validation of a Bayesian network for the differential diagnosis of anterior uveitis. Eye 2016;30:6:865-872.
3. Kim JE, Park SJ, Oh JY, et. al. Successful treatment of tubulointerstitial nephritis and uveitis with steroid and azathioprine in a 12-year-old boy. Korean J Pediatr 2016;59
4. Okafor LO, Hewins P, Murray PI, et al. TINU syndrome: A systematic review of its epidemiology, demographics and risk factors. Orphanet J Rare Dis 2017;12:1:128.
5. Mandeville JT, Levinson RD, Holland GN. The tubulointerstitial nephritis and uveitis syndrome. Surv Ophthalmol 2001;46:3:195-208.
6. Aguilar MC,
7. Goda C, Kotake S, Ichiishi A, et. al. Clinical features in TINU syndrome. Am J Ophthalmol 2005;140:4:637-641.



