Presentation
A 5-year-old female presented to her pediatrician with a “pink” left eye, which progressed to a painful eye with a dilated pupil over the next two weeks. The patient was evaluated by an optometrist who found 2+ anterior chamber cells in the left eye and initiated treatment with prednisolone acetate. Examination of the asymptomatic right eye was within normal limits.
Several days later another optometrist found that the visual acuity in the left eye was 20/25 and the intraocular pressure 40 mmHg. There was 2+ anterior chamber cells and a spiderweb-like plaque with a scalloped border on the posterior lens capsule. There were 1+ cells in the anterior vitreous and a white vitreous strand extended from the inferotemporal ora serrata to the mid-peripheral retina. The right eye remained normal.
The patient underwent an extensive work-up at an outside facility, including magnetic resonance imaging of the brain, which was read as normal, and an extensive serologic work up including CBC, BMP, ESR, ANA, tick-borne diseases panel (including Lyme), treponemal antibodies, toxoplasma, QuantiFERON gold, ACE, lysozyme, bartonella and HLA-B27, all of which were normal.
During the subsequent months, the patient had persistent inflammation and elevated intraocular pressure in the left eye, necessitating corticosteroid injections, goniosynechiolysis, and ultimately an Ahmed valve tube shunt. She was managed by ophthalmology in consultation with rheumatology and treated with methotrexate and adalimumab for recurrent episodes of inflammation. Finally, 11 months after initial presentation, the patient was referred for an additional opinion by our team.
Examination
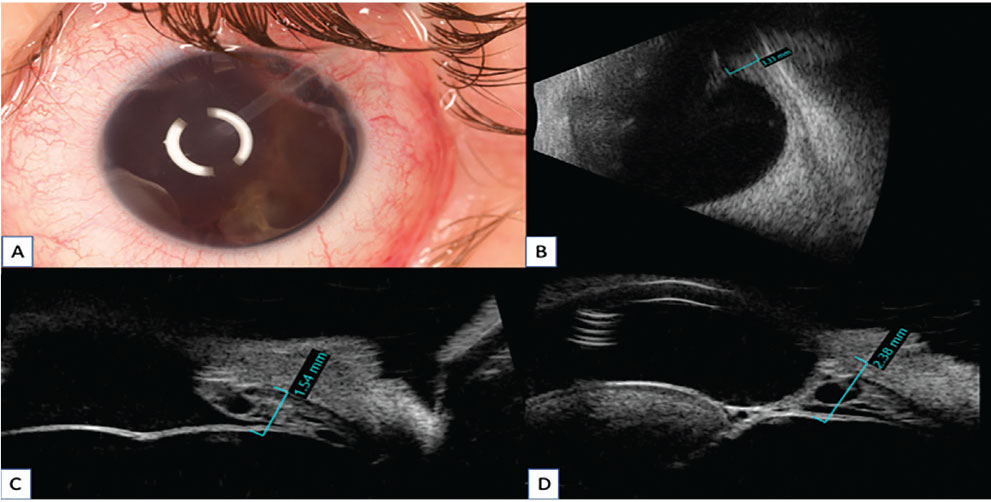 |
| Figure 1. A) Clinical features on an external photograph. B) B-scan ultrasonography of mass with a depth of 3.33 mm. C,D) Ultrasound biomicroscopy of ciliary body mass demonstrating intratumoral cysts. Click image to enlarge. |
On examination, the right eye was normal, with 20/20 acuity and 15 mmHg IOP. Acuity in the left eye was 20/200 and the IOP was 20 mmHg, despite the patient being on several glaucoma medications. The anterior segment exam revealed a white and quiet conjunctiva, clear cornea and a long tube shunt in the anterior chamber. There was complete retraction of the iris into the anterior chamber angle and the anterior and posterior surfaces of the inferonasally subluxed lens were enveloped by a translucent membrane (Figure 1A). The view of the posterior segment was hazy, and showed a fluffy, white membrane with occasional cysts lining the pars plana, and an optic nerve with a cup-to-disc ratio of 0.3. B-scan of the posterior segment in the left eye revealed a peripheral, solid mass (Figure 1B). The retina was flat.
What is your diagnosis? What further workup would you pursue? The diagnosis appears below.
Diagnosis and Management
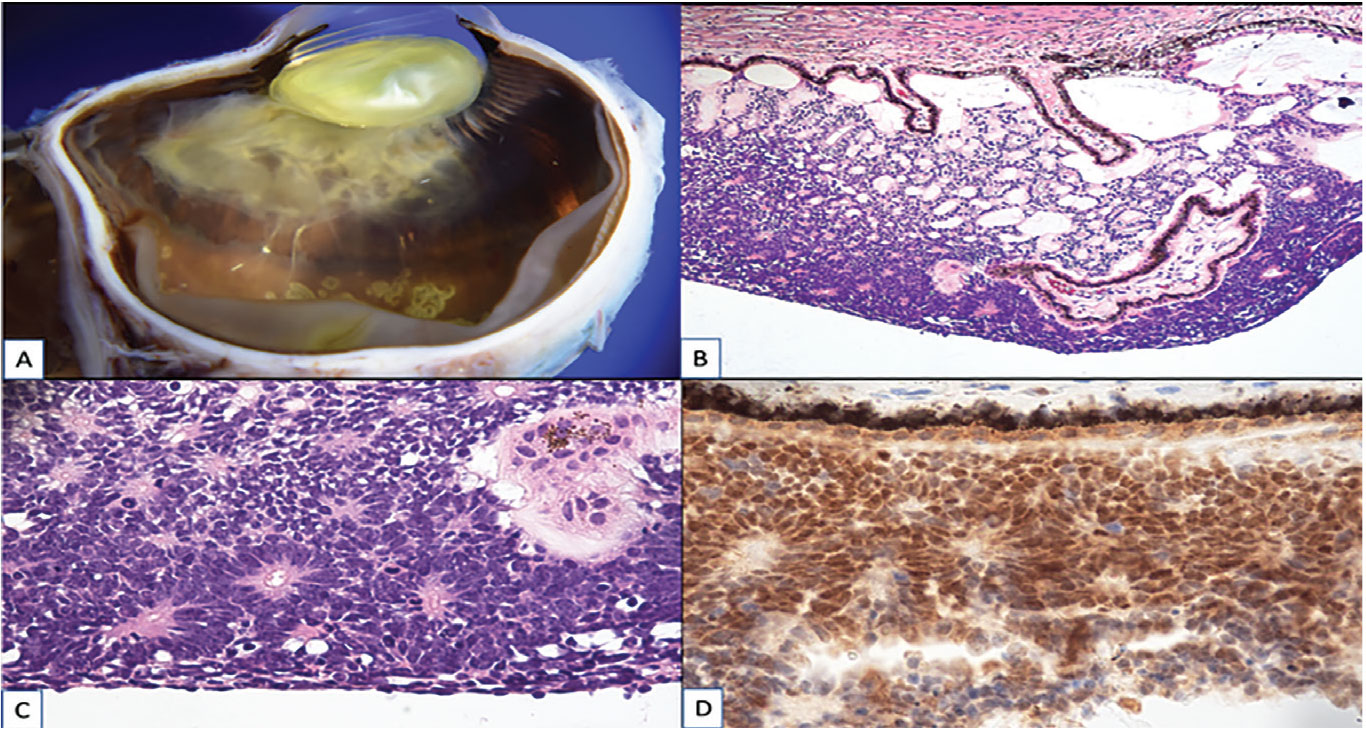 |
| Figure 2. Pathology features: A) Gross dissection photograph showing a poorly circumscribed white to tan tumor covering the pars plicata and the anterior half of the pars plana of the ciliary body. B) Photomicrograph showing a basaloid tumor on the inner surface of the ciliary body. C) Photomicrograph showing mitotic figures and Flexner-Wintersteiner rosettes. D) Photomicrograph showing positive immunoreactivity for RB1 protein. Click image to enlarge. |
The patient was examined under anesthesia. Anterior segment fluorescein angiography showed 360-degree neovascularization of the iris retracted into the anterior chamber angle and neovascularization within the enwrapping lenticular membrane. Anterior segment OCT demonstrated flattening of the iris surface from iris neovascularization. Ultrasound biomicroscopy was most informative, demonstrating a multicystic, wispy ciliary body mass that involved nine clock-hours and extended into the anterior chamber, enwrapping the tube shunt (Figure 1C). All imaging of the right eye was normal.
Based on the results of the exam and imaging, the patient was suspected to harbor a non-pigmented ciliary epithelial medulloepithelioma. MRI of the brain and orbits revealed no evidence of extraocular extension of the tumor. Because the tumor involved at least 75 percent of the pars plana and a tube shunt was present, minimal-manipulation enucleation was performed to minimize the risk of extrascleral extension and metastasis. The globe and tube shunt were removed completely as a unit and orbital biopsies were taken. The patient tolerated the procedure well without complication.
Gross dissection of the enucleated eye was notable for a poorly circumscribed white-to-tan tumor with a fluffy translucent appearance and cystoid spaces that filled part of the posterior chamber and covered the pars plicata and the anterior half of the pars plana of the ciliary body. Several delicate strands extended from the tumor onto the peripheral retina (Figure 2A). Histopathology disclosed a basophilic, mitotically-active cellular tumor on the inner surface of the ciliary body that contained multiple Flexner-Wintersteiner rosettes with small central lumina (Figure 2C). The tumor contained pools of mucopolysaccharide and had areas with a diktyomatous appearance (Figure 2B). The nuclei of the tumor cells showed convincingly positive immunoreactivity for RB1 protein (Figure 2D), excluding retinoblastoma as a diagnosis. There was no sign of optic nerve invasion, nor evidence of extraocular tumor in the Ahmed tube shunt capsule or orbital biopsies. No heteroplastic elements were present. The final diagnosis was non-teratoid malignant ciliary body medulloepithelioma without extrascleral extension. The patient didn’t require additional radiotherapy or chemotherapy.
Discussion
Medulloepithelioma is a rare tumor of the nonpigmented ciliary epithelium that occurs most frequently in children at a mean age of onset of 5 years.1-3 The classic tetrad for medulloepithelioma is leukocoria, lens notch, neovascular glaucoma and a cystic ciliary body mass.4,5 Common findings include glaucoma in 44 percent, cataract in 46 percent, iris neovascularization in 51 percent, neoplastic cyclitic membrane in 51 percent and intratumoral cysts in 61 percent. By histopathology, 80 percent of tumors are malignant.3 When present, a neoplastic cyclitic membrane serves to distinguish medulloepithelioma from retinoblastoma and Coats disease.3 Diagnosis of this tumor is often challenging; one study demonstrated that 88 percent are misdiagnosed initially and 39 percent have undergone prior treatment for secondary effects of the tumor prior to diagnosis.3
The patient with medulloepithelioma reported here was thought to have uveitic glaucoma and was treated with systemic immunosuppressive therapy and an Ahmed tube shunt. Although medulloepithelioma typically masquerades as neovascular glaucoma,1,3,6,7 it also can masquerade as uveitic glaucoma.8,9 Medulloepithelioma has been misdiagnosed as persistent fetal vasculature (PFV) (also known as persistent hyperplastic primary vitreous [PHPV])9 and, in fact, 20 percent of patients diagnosed with medulloepithelioma have been found to have some degree of PFV/PHPV.2 The unusual pseudo-uveitic nature of this patient’s presentation may be one reason the diagnosis was delayed.
Tube shunt implantation in patients with unsuspected intraocular tumors, including medulloepithelioma, has been reported and, in some instances, the tube shunt has served as an avenue for extrascleral extension of tumor.6 In cases of medulloepithelioma in which a tube shunt has been implanted, the mass was difficult to visualize as it was hidden behind the iris,6 as was the case for the patient in this report. Anterior segment OCT and ultrasound biomicroscopy have been recommended as effective imaging modalities to identify ciliary body tumors that are hidden by the iris and not evident on clinical examination.1 Plaque radiotherapy has been used to effectively treat localized small- to medium-sized cases of medulloepithelioma, with tumor control in 83 percent of patients and globe salvage in 67 percent of patients.10
In conclusion, ciliary body medulloepithelioma is a rare tumor of the nonpigmented ciliary epithelium that’s frequently misdiagnosed on initial presentation. The classic tetrad of leukocoria, lens notch, neovascular glaucoma, and a cystic ciliary body mass may not always be present, and a high degree of suspicion is necessary in order to make the diagnosis. In cases of pediatric neovascular glaucoma with a normal fundoscopic examination, consider medulloepithelioma in the differential diagnosis, and be sure to perform either anterior segment optical coherence tomography or ultrasound biomicroscopy to look for an occult ciliary body mass.1
1. Tadepalli SH, Shields CL, Shields JA, Honavar SG. Intraocular medulloepithelioma–A review of clinical features, DICER 1 mutation, and management. Indian Journal of Ophthalmology 2019;67:6:755-762.
2. Broughton WL, Zimmerman LE. A clinicopathologic study of 56 cases of intraocular medulloepitheliomas. American Journal of Ophthalmology 1978;85:3:407-418.
3. Kaliki S, Shields CL, Eagle RC, et al. Ciliary body medulloepithelioma. Ophthalmology 2013;120:12:2552-2559.
4. Peshtani A, Kaliki S, Eagle RC, Shields CL. Medulloepithelioma: A triad of clinical features. Oman Journal of Ophthalmology 2014;7:2:93.
5. Shields JA, Eagle RC, Shields CL, De Potter P. Congenital neoplasms of the nonpigmented ciliary epithelium (medulloepithelioma). Ophthalmology 1996;103:12:1998-2006.
6. Kaliki S, Eagle RC, Grossniklaus HE, Campbell RJ, Shields CL, Shields JA. Inadvertent implantation of aqueous tube shunts in glaucomatous eyes with unrecognized intraocular neoplasms: Report of 5 cases. JAMA Ophthalmology 2013;131:7:925-928.
7. Vempuluru VS, Jakati S, Krishnamurthy R, Senthil S, Kaliki S. Glaucoma as the presenting sign of intraocular tumors: Beware of the masquerading sign. International Ophthalmology 2020;40:7:1789-1795.
8. Chua J, Muen WJ, Reddy A, Brookes J. The masquerades of a childhood ciliary body medulloepithelioma: A case of chronic uveitis, cataract, and secondary glaucoma. Case Reports in Ophthalmological Medicine 2012;2012:493493-3.
9. Pushker N, Bajaj MS, Singh AK, Lokdarshi G, Bakhshi S, Kashyap S. Intra-ocular medulloepithelioma as a masquerade for PHPV and panophthalmitis: A diagnostic dilemma. Saudi journal of Ophthalmology 2017;31:2:109-111.
10. Ang SM, Dalvin LA, Emrich J, Komarnicky L, Shields JA, Shields CL. Plaque radiotherapy for medulloepithelioma in 6 cases from a single center. Asia-Pacific Journal of Ophthalmology 2019;8:1:30-35.



