Brain plasticity—the ability of the brain to structurally alter itself and create new axonal connections in response to changing internal and external conditions—has become a hot topic during the past decade. The implications for healing and regaining lost function following brain damage are profound, and programs designed to take advantage of this have begun to proliferate.
One player in the area of vision rehabilitation following brain damage is NovaVision, a small company in
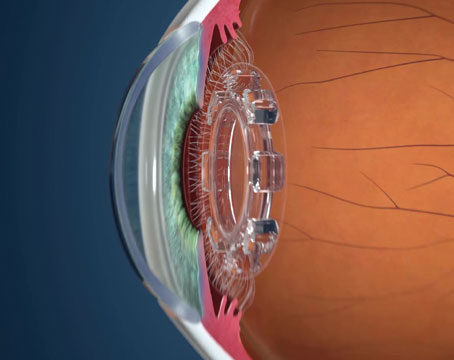
"The ability of the brain to create new neuronal pathways has now been well-documented through clinical trials and functional MRI studies," says Rudy Mazzocchi, president and CEO of NovaVision. [For summaries of key publications and data relating to this process and stroke, visit novavision.com/Research.html.] "The VRT system takes advantage of this ability, using the healthy, intact retina as a conduit to the damaged visual cortex of the brain. It forces the brain to detect photic stimuli on the border of the functional area where there is some residual vision. As a result, new neural connections form and the visual field gradually expands."
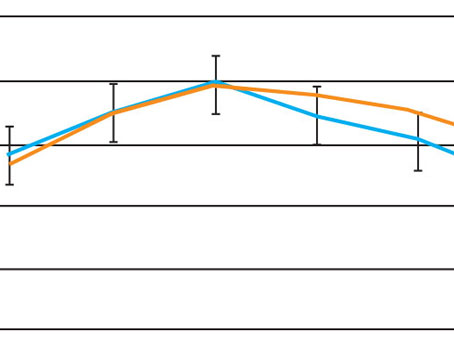
Does it really work? "The VRT system was cleared by the FDA back in 2003, and we've now treated close to 3,000 patients worldwide," notes Mr. Mazzocchi. "Today we're primarily treating patients with stroke or traumatic brain injury, brain tumors and, to some degree, optic nerve damage. A lot of these patients are hemianopic; half of their visual field is gone." The company claims that treatment can open up 80 to 90 percent of the central, high-acuity area of the visual field. (See sample cases) "In terms of subjective improvement, 88 percent of our patients have indicated at least one major quality of life improvement after their therapy, such as improved reading, driving or movie and television viewing," he says. (See chart)
How It Works
The VRT program is completed in the patient's home once a physician has prescribed the therapy. The therapy device, consisting of a mini-processor, a CRT display that presents the fixation point and photic stimuli, a foldable chin-rest that positions the patient's eyes at a predetermined distance from the screen, and a mouse for responding, is leased by the patient and shipped to the patient's home. It arrives preloaded with the first set of software programs customized for that individual, based on eye exam information and a visual field map provided by the ophthalmologist. (The practice doesn't have to invest in any equipment to offer VRT.)
The fixation target in the center of the screen periodically changes shape and color; the patient responds by clicking a mouse every time it changes, as well as whenever he sees another light stimuli appear elsewhere on the screen. The computer walks the patient through the process. "At the outset of the therapy, many stimuli appear within the functional visual field," explains Mr. Mazzocchi. "Then the stimuli slowly move into the blind area. It's like gradually sliding a curtain open."
Patients are required to undergo therapy 20 to 30 minutes a day. The company urges them to do it twice a day, six days a week. NovaVision monitors the patient's progress via the Internet, downloading the patient's results every evening. If a patient doesn't use the program for three or four days, someone at NovaVision contacts the patient to find out what's wrong.
Each month the company sends the patient revised software, adjusted based on the patient's progress. (The company hopes to switch to a self-revising software program this year.) The company also sends the prescribing physician a monthly report on the patient's progress.
How long does it take to achieve results? "The threshold of therapy usually occurs around month three, so we encourage physicians to give the patient a prescription for a minimum of three months," says Mr. Mazzocchi. "NovaVision can provide follow-up modules of the software for three additional months. Some patients undergo the therapy for nine to 12 months because they like the progress they're experiencing."
Apparently, there are plenty of eligible patients. "There are about 700,000 new acute stroke patients every year in the
Mr. Mazzocchi points out that practices also benefit from directing appropriate patients to this therapy. "In addition to actually having a treatment option to offer these patients, the follow-up visits help to generate revenue," he says. "Also, we reimburse the physician approximately $250 for analyzing the patient's progress reports and making a recommendation on the algorithm for the therapy. That money comes out of the fees that we capture from the patient, who's billed for the first three months of therapy when we ship the equipment." (Mr. Mazzocchi says NovaVision currently charges $1,950 for the first three months of therapy and $650 per month if the patient elects to continue.)
What the Doctors Say
Andrew Berman, MD, a general ophthalmologist and neuroophthalmologist who has practiced in
"Most of my patients haven't realized a significant enlargement of their visual fields," he continues. "I think the largest field expansion I've seen was 4 to 6 degrees. However, they respond to their visual environment more quickly, accurately and comfortably after therapy, and this can be enormously helpful in performing activities of daily living. These positive changes can usually be appreciated between the third and sixth modules, with each module taking about 32 days to complete. Some of my patients are two years out now, and they feel that what they gained from the training is permanent."
Mohammad Fouladvand, MD, associate professor of ophthalmology and neurology, and neuroophthalmologist at
"We've had a fair amount of good experience, and some of my patients do very well, beyond any placebo effect," he notes. "But I think patients who have a partial field defect have a better chance of improvement than those with a total loss of visual field on one side. And younger patients are more computer-oriented, which may work in their favor."
What's Next?
Mr. Mazzocchi notes that in addition to upgrading the software, NovaVision is involved in a clinical trial to evaluate using this therapy to treat dry macular degeneration. "Our aim is to improve the functional acuity of the peripheral retina these patients are now using to see," he notes.
1. Jung CS, Bruce B,
2. Romano JG, et all. Visual field changes after a rehabilitation intervention: Vision restoration therapy. J Neural Sci 2008;15:273:1-2:70-74.
3. Meuller I, et al. Visual Impairment Research 2003;5:157-178.