“Meibomian gland dysfunction is a major cause of dry eye,” notes Reiko Arita, MD, PhD, clinical researcher in the department of ophthalmology at the University of Tokyo School of Medicine, and an associate professor at Keio University. “However, conventional meibography is performed in a limited number of clinics, probably because of the necessity for examiner expertise, as well as patient discomfort induced by the direct application of a transilluminating light probe to the eyelid.”
To create a less-invasive option, Dr. Arita’s team has developed two noncontact meibography systems. The first, designed to attach to a slit lamp, includes an infrared filter and an infrared charge-coupled video camera. “In this system, a transilluminating probe is not necessary, making it more patient-friendly,” he explains. “The structure of the meibomian glands can easily be observed in both the upper and lower eyelids of patients without causing patient discomfort.
“Using this system we’ve reported some new findings,” he continues, “including the shortening of meibomian glands in contact lens wearers, meibomian gland duct distortion in patients with perennial allergic conjunctivitis, and the dropout of meibomian glands in patients with obstructive meibomian gland dysfunction. The system is also useful for differentiating aqueous-deficiency dry eye from lipid-layer-deficiency dry eye. Moreover, we found meibomian gland dropout in patients who have used anti-glaucoma eye drops for more than six months.”
Taking the Next Step
Despite its advantages, the slit-lamp system has some downsides. “Because there are many kinds of slit lamps all over the world, this system can’t be used in all facilities,” he notes. “Also, it can’t be used to examine the meibomian glands of patients who can’t use the chin rest, such as infants or inpatients with severe systemic diseases.”
Most of the limitations of the slit-lamp system have now been eliminated with their latest iteration: a portable, handheld, pen-shaped meibography device, manufactured by Topcon. “Our mobile, pen-shaped device comprises an infrared LED light source (wavelength 940 nm), a highly sensitive video camera for the acquisition of a clear image, and computer imaging software,” he says. “It’s connected to a monitor or a personal computer. It provides a panoramic view of all of the meibomian glands along the upper or lower eyelid. To avoid catoptric [reflected] light, the body of the pen-shaped device is held vertically toward the eyelid. None of the subjects have reported glare, discomfort or pain during the meibography procedure.
“Using this mobile pen-shaped meibography device, we can observe meibomian glands in patients who can’t sit up,” he continues. “We can visit a home for the aged and diagnose meibomian-related diseases. We can also monitor the changes in the meibomian glands of both healthy infants and those with congenital diseases such as congenital ectodermal dysplasia and congenital insensitivity to pain with anhidrosis.”
In a recent study, Dr. Arita’s group compared the new handheld device to the slit-lamp system they had previously developed.1 “We used both systems to visualize the upper and lower eyelids of healthy volunteers and patients with meibomian gland dysfunction, contact-lens wearers with dryness and patients with allergic conjunctivitis,” he says. “The quality of images using the mobile meibography device was similar to those captured using the slit-lamp meibography system.”
The handheld device currently costs about $3,000 and is available for import, but has not been approved by the Food and Drug Administration.
Other New Options
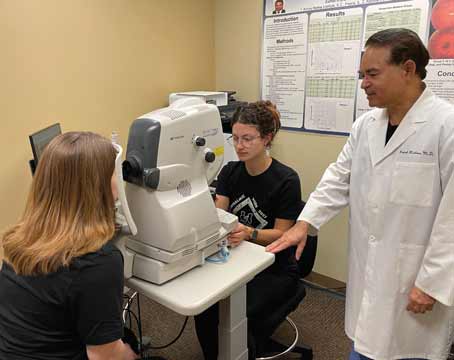
“We need to have new ways to perform meibography,” agrees Sruthi Srinivasan PhD, BS Optom, FAAO, research assistant professor at the Centre for Contact Lens Research at the University of Waterloo in Ontario. Her group has been conducting meibomian gland research, first using the Oculus Keratograph 4 and more recently the newer Oculus K5M. “Some of the older meibography methods were more research-oriented, and not clinician-friendly,” she notes. “They tended to involve bulky equipment and be time-consuming, and there was some discomfort for the patient. Video processing was difficult as well—we never got a full picture of the lid in one shot, so we had to stitch them together. The new devices take a full picture of the lid in one shot.”
|
“The new model [K5M] includes dedicated meibography software, allowing us to take meibography images more easily,” she says. “Also, the working distance has been increased to enlarge the field of view; the infrared diodes have been rearranged; and the images are optimized for clarity and much easier to obtain. In addition, this instrument gives you a variety of tools in a single platform. That’s why we find it more beneficial than other stand-alone meibography tools.”
Dr. Srinivasan notes that a clinician-friendly meibography device will help both patients and clinicians. “Clinicians can explain the condition more easily to patients if they have a picture,” she says. “They can correlate the signs and symptoms to the patient’s experience. It will also allow clinicians to take a series of pictures over time, to determine whether the glands are changing.
“Using the current Oculus keratograph is very simple,” she continues. “Patients rest their head on the chin rest, and you use a cotton tip applicator to gently evert the lower or upper lid. You click on the meibography option, and that opens up a window onscreen. Sometimes you may need an assistant to hold the lid in place, but if you’re an experienced user, you can probably do it yourself. Then it’s as simple as clicking a button to capture a photo or video.”
Dr. Srinivasan says the instrument isn’t currently able to perform digital analysis and quantification of images, but this can be done using other software. “There are numerous subjective grading scales for this purpose,” she explains. “But we can use a program like ImageJ to outline the areas
of gland loss and then calculate the gland loss as a percentage of the total area of the lid, which is more objective.” She admits that digital quantification is probably more than is needed for clinical use. “But if you want a precise quantification of percentage loss,” she says, “it is possible to achieve.” REVIEW
Dr. Arita is an advisor to Topcon. The Centre for Contact Lens Research has conducted funded research studies on behalf of Oculus during the past three years, but Dr. Srinivasan personally does not have a financial relationship to Oculus or the instruments described.
1. Arita R, Itoh K, Maeda S, et al. A Newly Developed Noninvasive and Mobile Pen-Shaped Meibography System. Cornea 2013;32:3:242-247.
2. Srinivasan S, Menzies K, Sorbara L, Jones L. Infrared imaging of meibomian gland structure using a novel keratograph. Optom Vis Sci 2012;89:5:788-94.