In May, Review interviewed doctors across the country about their states’ elective surgery reopening protocols. Most reported slow increases in patient volume and expressed hope for flattening the curve. Recently, we checked in again to see what new challenges are afoot.
“COVID-19 cases have gone up markedly in Utah since May,” says Nick Mamalis, MD, of the Moran Eye Center in Salt Lake City. “We had on the order of about 150 cases a day, and then in June and July cases increased rapidly and peaked at about 900 cases a day. Fortunately in the Salt Lake City area, we’ve peaked and are starting to come down again, thanks to the institution of masking and social distancing. We’re down to around 300 daily cases now.”
“In California, we benefited from the large-scale early shutdown, but as the state began reopening, we saw case numbers climbing,” adds
Michele C. Lim, MD, of the University of California, Davis in Sacramento. She points out, conversely, that “when the case load was low in the beginning, we were completely shut down, but now as time goes on and cases are surging, everything is going full steam ahead.”
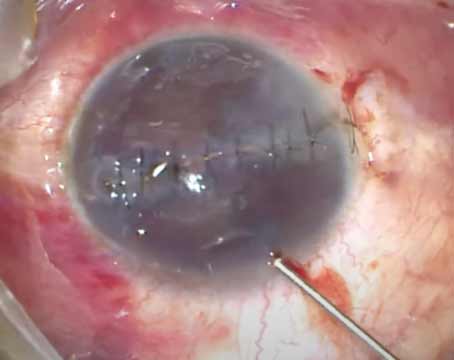
The Moran Eye Center requires pre-surgical COVID testing within 72 hours of cataract surgery. “We’ve blocked off part of our parking garage and set up a testing center, so we can do our own testing here,” says Dr. Mamalis. The patients are then instructed to stay home until their surgery.
In May, Vanderbilt Eye Institute’s Paul Sternberg Jr., MD, who’s also the physician lead for its COVID-19 Response Command Center, said Vanderbilt had set up its own PCR test and was running about 700 to 800 tests a day. Now he reports that tests have been as high as 1,200 a day. “We anticipate an uptick in patient requests for testing since school is about to start,” he says.
Rishi Singh, MD, in practice at the Cole Eye Institute in Cleveland, Ohio, says, “Our numbers for both eye-related and systemic issues like cancer and heart disease all went down over the past few months. I think people probably ignored many of their disease symptoms and waited to see if they’d resolve on their own, rather than risk coming into the clinic and being potentially exposed to COVID.”
Delays in seeking care have affected many during the pandemic. Dr. Lim reports that she recently had a few patients come in with very high pressures who’d been previously well-controlled, but hadn’t been seen in months. “These patients went to the OR urgently to get their pressures under control,” she says.
“The cases we’ve been seeing recently have been more significant in nature,” Dr. Singh agrees. “Those with diabetes whom we’re following for proliferative diabetic retinopathy have been coming back worse than before. Patients with AMD who hadn’t been seen for months have lost vision, some of which is almost irreparable at this point.”
Patients are returning to the clinic, though. Dr. Mamalis reports that his practice is back to about 90 percent of its pre-pandemic clinic volume. “The pandemic has really affected patient flow and how we see patients, and it’s put a burden on our technicians,” he says. “We no longer move patients from room to room. Now, they’re taken to one room for both the workup and for the doctor to see them. Afterwards, the entire room is cleaned, including the chair, slit lamp, door and counters. If the patients need to go somewhere else for a test, that room is closed afterwards.”
Maintaining adequate social distancing in the clinic is another challenge that comes with increasing patient volume. “We’re holding our clinic volume at 80 percent because we don’t have enough space to physically distance at our pre-pandemic volume,” says Dr. Lim. Her Saturday imaging clinics took the place of her drive-thru exams. “I have patients come in for visual fields, OCT imaging and pressure checks on Saturdays, and I follow up with a video visit,” she says. “It’s worked out well—the hospital is mostly empty on Saturdays and patients don’t need to take time off work.”
“The other big challenge we’re facing now is the fact that some of these returning patients are COVID-positive,” Dr. Singh says. “How do you see them? Do you see them alongside your other clinic patients? Do you distance them differently? The protocols are constantly evolving; it seems to change from week to week as far as recommendations go.”
Daniel Chang, MD, of Bakersfield, California, whose practice has ramped up to 75 to 80 percent of its pre-pandemic patient volume, adds that some of his staff members have come down with COVID. “With contact tracing, we found that no infections were transmitted at the office; they came from outside contacts, like at family events and parties. Fortunately, most of the affected staff are young and healthy, and bounced back quickly.” Per the CDC guidelines on aerosol transmission, many clinics have begun using eye protection in addition to N-95 masks.
But challenges also come from beyond the medical realm. “We initially thought staff infections would be the biggest challenge, but another thing we’re currently facing in California is the schools having only distance learning,” says Dr. Chang.
Dr. Sternberg echoes these concerns. “We’re working on creating more flexibility for our schedules so that parents can balance their child-care and professional responsibilities,” he says.
On the bright side, Dr. Chang points out that this pandemic has pushed doctors to work more efficiently. “We’ve also created a safer, cleaner environment for our patients, which will prove better in the long run,” Dr. Sternberg adds. “The safest place in your community is the doctor’s office—it’s the only place you’ll go where everyone has a mask on. Patients need to come back and feel comfortable; they need their preventive care.”
Face-Mask Difficulties
An article, published online ahead of print in the Journal of Glaucoma, reports that improperly fitted face masks can cause artifacts on standard automated perimetry.
In the case study, a 32-year-old female underwent SAP with the 24-2 SITA Fast test of the Humphrey Field Analyzer while wearing an ear-loop surgical mask. Post-testing, it was noted that the mask had ridden up on the woman’s face. Condensate was noted on the perimeter lens.
SAP demonstrated good reliability indices, but there was a marked reduction in sensitivity inferiorly in both eyes. In addition, the Glaucoma Hemifield Test was outside normal limits. As a result, the staff made sure that the upper border of the patient’s mask was well-sealed, with the loops secured around the ears and the nasal strip of the mask pinched down. Repeat visual fields were found to be normal.
The authors suggest that adjustments to the fit of face masks may help prevent fogging or mask slippage and increase test reliability. REVIEW
1. Young SL, Smith ML, Tatham AJ. Visual field artifacts from face mask use. J Glaucoma 2020; Jul 14. [Epub ahead of print].
 |