|
| When dry-eye symptoms include photophobia, it’s likely there’s an underlying neuropathic etiology. |
Dry Eye-Like Symptoms
Dry eye-like symptoms are triggered by specialized corneal nerve receptors4 designed to protect the integrity of the mirror-smooth corneal tear film necessary for enhancing the optical quality of the external corneal surface. This collection of nociceptors—mechanoreceptors, chemoreceptors and thermoreceptors—detects the subtlest changes in the ocular surface environment and functions as our cornea’s alarm system to warn us of potentially harmful disruption of the status quo. In particular, specialized thermal sensors provide an indirect measure of the thickness of the tear film. By sensing slight changes in ocular surface temperature, they monitor the rate of tear-film evaporation to provide a measure of both tear-film thickness and osmolarity in real time.5 The sensors’ responses to environmental conditions are a modulation of their excitability and an alteration of neuronal action potential firing rates. Like any such alarm system, modulation can be either positive or negative. As an example, on a windy day evaporation at the ocular surface is increased, and the activation of thermoceptors will increase the firing rate of the corneal sensory nerves, triggering an increase in lacrimal gland secretion to compensate for the accelerated tear-film thinning. Like all sensory nerves, continuous input modulates the set point, or activation threshold. All is well as long as this set point is in synchrony with other parts of the sensory feedback loop.
What happens when there is dysregulation of the sensory nerve circuit? If the triggering threshold is too high, the system will be relatively insensitive to the external environment, and the tear film will thin and break up, causing a loss of clarity, unstable vision and an exposed ocular surface. If the sensor threshold is set too low, the biological alarm will be triggered prematurely, generating dry eye-like symptoms in the presence of a normal tear film: a false alarm. These sensory circuits are described as being sensitized, and would be expected to require thicker-than-normal tear films to keep the dry-eye alarm in a silent mode. Under these conditions, sensory neurons respond to the ocular surface environment with symptoms of dryness, even though there is little or no stimulus generating that perception. Like all sensitive, powerful and complex systems, corneal innervation is vulnerable to component breakdown, with the result being neuropathic pain, a disease in its own right.
Dry Eye-Like Pain
Activation thresholds of tear film corneal sensors are lowered in the presence of inflammatory products such as pro-inflammatory cytokines.6 Increased activity of sensory nerves can also cause inflammation in the form of neuro-inflammation, which in turn ramps up the activity of pain-carrying nerves, leading to a self-perpetuating phenomenon known as peripheral sensitization.7 For many patients this can be reversed after resolution of the inciting stress and ocular surface inflammation.8 Some dry-eye patients experience only transient episodes of pain, whereas others have persistent symptoms of chronic disease. Neuropathic pain is by definition “pain arising as direct consequence of a lesion or disease affecting the somatosensory system,” and is often chronic.9
The transmission of dry-eye pain signals to the somatosensory cortex is not a passive process. Along the way, these electrical signals are modified by feed-forward and feedback systems that typically intensify the signals. This explains the unique property of pain to become amplified during a constant noxious stimulus, in contrast to most other types of sensory responses that adapt during persistent stimulation and thereby attenuate the responses. This physiological phenomenon, known as central sensitization, occurs with dry eye-like pain as well.8 Since the trigeminal brainstem was shown in animal models to be the location of central control of homeostatic corneal wetness,10 corneal algesia11 and aversive responses to light,12 the brainstem may also be the origin of the clinical expression of dry-eye-related pain. The possibility that disorders of the dry-eye alarm system itself can explain the variety of clinical patterns associated with dry eye-like pain offers a strikingly different perspective. Moreover, the location and persistence of this dysfunctional alarm system can alter the functional anatomy through the well-known, innately powerful neuroplasticity of the central nervous system. These maladaptive changes in the CNS result in neuropathic pain.
Possible Origins of the Pain
For us to be able to manage these cases effectively, it’s important to recognize the factors influencing neuropathic pain. Age-related dry-eye disease is characterized by the attrition of corneal nerve fibers. Its consequences are associated with an increased sensitivity to tear evaporation, or corneal evaporative hyperalgesia. Pain fiber attrition also occurs in de-afferentation hypersensitivity, a phenomenon found in the skin of healthy elderly subjects. The loss of nerve fibers in these conditions is associated with increased activity of the surviving nerves.13 The parallels between this condition and age-related dry eye are striking.
In mice, it has been demonstrated that sensory nerve injuries, such as those caused by LASIK axotomies, trigger a phenotypic change in the somata of the surviving nerves from conduction to regeneration, promoting the expression of atopic pain generators that are hypersensitive and hyper-responsive14 and that are transported to the regenerating nerve sprouts and the central terminals of severed axons from the nerve somata in the trigeminal ganglion where they’re expressed. This likely is responsible for the complaints of dry-eye symptoms following refractive procedures. Persistence of the regenerating phenotype long after healing has occurred, sometimes years after LASIK, as suggested by the characteristic morphology of regenerating nerves and increased numbers of mature dendritic cells in the sub-basal plexus, may explain the chronicity of dry-eye pain even in the absence of external signs of inflammation.
| In Memoriam: Henry F. Edelhauser, PhD |
| It is with great sadness that I relate the recent death of my colleague and friend Henry F. Edelhauser, PhD. Hank spent his career, first at the Medical College of Wisconsin and, since 1989, at the Emory Eye Center in Atlanta working in translational ophthalmic research, something near and dear to my own heart. Hank’s intuitive understanding of ocular physiology and his gift for insightful clinical research led to his seminal work on the corneal endothelium and to the development of irrigating solutions for ophthalmic surgery. He was a pioneer in the development of methods for ocular drug delivery, and it’s fair to say that his work improved the vision and visual health of many thousands of patients over the course of his life. As just one example, the scales that Hank developed to help us quantify the health of the corneal epithelium are used routinely here at our research firm Ora, and in specular microscopy exams in clinics all over the world every day. I was fortunate enough to have shared a podium or two with Hank over the years, and I was always impressed by his ability to succinctly and eloquently describe the most complex of physiological concepts. The author of more than 250 publications, a past president of the Association for Research in Vision and Ophthalmology, and the recipient of numerous awards including the Proctor medal, Hank was one of the great ophthalmic researchers of our time. His passion for science was palpable and was transmitted over his long, successful career to colleagues and students alike. He will be missed. —MBA |
It has been well known for years that our psychological well-being profoundly influences our immunological status. Pain thresholds are also known to be increased by meditation.16 The flip side of this should not be a surprise. In the present context, patients with depression or post-traumatic stress disorder have a twofold increased risk of a dry-eye diagnosis compared to those without these diagnoses. Studies with Asian populations have shown similar relationships between depression and dry eye. Data from the national Veterans Administration database demonstrated that patients with chronic pain diagnoses are more likely to also have a dry-eye diagnosis. Patients with dry eye were also found to have higher pain sensitivity at a remote site (forearm) than those without the disease.8
We see that neuropathic pain accompanying dry eye might also be born from central sensitization in the central nervous system, and this possibility should be considered when weighing the contribution of signs versus symptoms presented by our patients diagnosed with dry-eye disease.
Diagnosis and Treatment
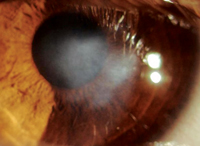
Identifying patients with a neuropathic component in their dry eye may influence treatment. Neuropathic pain is typically chronic and difficult to treat. It often includes burning, sharp, needle- or foreign body-like symptoms, and neuropathy should be considered when hearing these descriptors. It can also be expressed as spontaneous, and as a response to normally non-noxious stimuli, such as photo-allodynia. Esthesiometry has demonstrated lower sensitivity to mechanical stimuli, and some dry-eye patients report hypersensitivity to chemical fumes and cold. Confocal microscopy has identified neuronal morphological alterations in the corneal sub-basal plexus in patients with chronic dry-eye symptoms,8 even in the absence of external signs of inflammation (one author’s observations—PR). A history of abnormally heightened sensitivity to noxious stimuli and confocal morphological changes in patients with chronic dry-eye symptoms suggests a neuropathic component.
Such patients would benefit from an approach that includes treating the ocular surface with protective and anti-inflammatory agents, and treating central ocular sensory dysfunction with anti-neuropathic pain drugs. Research is needed to understand the role of the many available neuropathic pain treatments in treating dysfunctions of the ocular sensory apparatus associated with dry eye. Therapies are in development, some of which arise from studies of the pain genetics.17 We need effective regimens for neuropathic pain, and an important goal would be a diagnostic algorithm for neuropathic pain associated with dry-eye disease.8
We know that dry eye is not just a simple disease of tear deficiency and/or hyper-evaporation, but rather a heterogeneous group of disease subtypes with varying pathologies of the lacrimal gland unit and ocular sensory apparatus. It’s likely that a subgroup of dry-eye patients has neuropathic pain and central sensitization, making their condition more resistant to topical therapy designed to optimize the ocular surface. Identifying these conditions is paramount to solving the mystery behind this pain, and personalizing the treatment of dry eye. REVIEW
Dr. Abelson is a clinical professor of ophthalmology at Harvard Medical School, and emeritus surgeon at the Massachusetts Eye and Ear Infirmary. Dr. Rosenthal is emeritus surgeon at the Massachusetts Eye and Ear Infirmary, part-time assistant professor of ophthalmology at Harvard Medical School, founder and president of the Boston Eye Pain Foundation and founder of the Boston Foundation for Sight. Dr. McLaughlin is a medical writer at Ora Inc.
1. Mathers WD, Lane JA, Zimmerman MB. Tear film changes associated with normal aging. Cornea 1996;15:3:229-34.
2. Lane SS. A new system, the LipiFlow, for the treatment of meibomian gland dysfunction. Cornea 2012;31:4:396-404.
3. Galor A. Ocular surface parameters in older male veterans. Invest Ophthalmol Vis Sci 2013;54:2:1426-33.
4. Hirata H, Meng ID. Cold-sensitive corneal afferents respond to a variety of ocular stimuli central to tear production: Implications for dry eye disease. Invest Ophthalmol Vis Sci 2010;51:8:3969.
5. Belmonte C, Gallar J. Cold thermoreceptors, unexpected players in tear production and ocular dryness sensations. Invest Ophthalmol Vis Sci 2011;52:6:3888-92.
6. Watkins LR. Characterization of cytokine-induced hyperalgesia. Brain Res 1994;654:1:15-26.
7. Bhave G, Gereau RWT. Posttranslational mechanisms of peripheral sensitization. J Neurobiol 2004;61:1:88-106.
8. Galor A. Neuropathic ocular pain: An important yet underevaluated feature of dry eye. Eye (Lond) 2015;29:3:301.
9. Geber C. Revised definition of neuropathic pain and its grading system: An open case series illustrating its use in clinical practice. Am J Med 2009;122:10:S3-12.
10. Hirata H. A novel class of neurons at the trigeminal subnucleus interpolaris/caudalis transition region monitors ocular surface fluid status and modulates tear production. J Neurosci. 2004;24:17:4224-32.
11.Tashiro A. Behavioral and neurophysiological correlates of nociception in an animal model of photokeratitis. Neuroscience 2010;169:1:455-62
12. Rahman M. Trigeminal pathways for hypertonic saline- and light-evoked corneal reflexes. Neuroscience 2014;277:716-23.
13. Namer B. Microneurographic assessment of C-fibre function in aged healthy subjects. J Physiol 2009;587(Pt 2):419-28.
14. Wolf G. Genetic impairment of interleukin-1 signaling attenuates neuropathic pain, autotomy, and spontaneous ectopic neuronal activity, following nerve injury in mice. Pain 2006;120:3:315-24.
15. Rosenthal P, Borsook D. Ocular neuropathic pain. Br J Ophthalmol. 5 May 2015. doi:10.1136/ bjophthalmol-2014-306280. [Epub ahead of print]
16. Reiner K, Granot M, Soffer E. A brief mindfulness meditation training increases pain threshold and accelerates modulation of response to tonic pain in an experimental study. Pain Med. 8 Aug 2015. doi: 10.1111/pme.12883. [Epub ahead of print]
17. Nahorski MS, Chen YC, Woods CG. New Mendelian Disorders of Painlessness. Trends Neurosci 2015;38:11:712-24.