A 63-year-old Caucasian female without past ocular history presented with two to three weeks of black floaters
 |
Medical History
Past medical history was significant for depression, hypothyroidism, chronic left lower quadrant abdominal pain of unclear etiology, and diverticulosis. Of note, no inflammatory bowel disease, cancer or infection was found on her colonoscopy. She had an allergy to sulfa. She never smoked, used illicit drugs or drank alcohol.
Her medication list included levothyroxine 75 mcg daily and multiple antidepressants and anxiolytics, including bupropion 100 mg, risperidone 2 mg, duloxetine 30 mg, armodafinil 150 mg and trazodone 50 mg, all dosed daily or nightly, and clonazepam 0.5 mg as needed.
Examination
The patient’s vital signs were stable and within normal limits. Ocular examination demonstrated a best corrected visual acuity of 20/40 OD and CF at 1 foot OS. She had full extraocular movements. There was no relative afferent pupillary defect. Her visual fields were full OD but globally diminished OS. The periorbita and adnexae were normal.
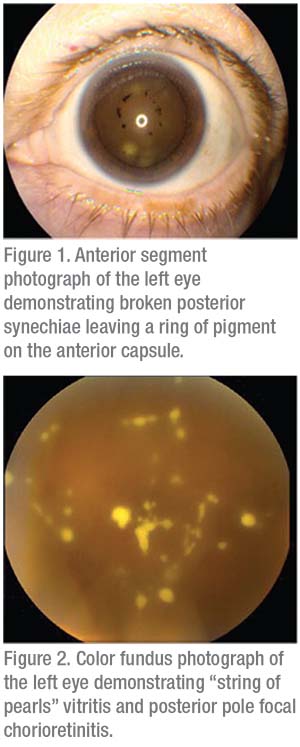
Anterior slit lamp examination of the right eye was normal. The left eye had corneal haze with 1 to 2+ Descemet’s membrane folds and diffuse inferior non-granulomatous keratic precipitates. The anterior chamber had 2+ cell without hypopyon. The iris revealed broken posterior synechiae with a ring of pigment on the anterior capsule of the lens (Figure 1). Intraocular pressure was 14 mmHg OD and 7 mmHg OS.
Fundoscopic examination was normal in the right eye. There was a hazy view to the back of the left eye with 1+ vitreous cells, and fluffy white-yellow lesions with a “string of pearls” appearance (Figure 2). The optic disc was normal. The vessels were without sheathing or vasculitis. The macular exam showed no edema, thickening or hemorrhage. However, there was focal chorioretinitis in the posterior pole.
What is your diagnosis? What further workup would you pursue? Click here for diagnosis and discussion.



