The differential diagnosis for bilateral serous retinal detachment is broad. It includes neoplastic, inflammatory, vascular, congenital and idiopathic disorders such as central serous chorioretinopathy. Given the patient’s post-partum status, the most likely etiologies were those associated with pregnancy, including pre-eclampsia, eclampsia, HELLP syndrome, disseminated intravascular coagulation (DIC), and thrombotic thrombocytopenic purpura (TTP).
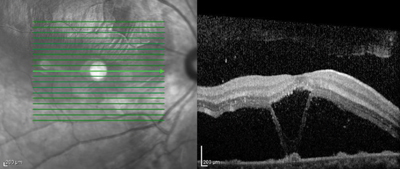
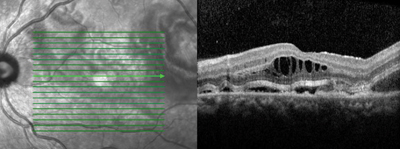
Her blood pressure was checked immediately and was normal. Optical coherence tomography demonstrated outer retinal edema and subretinal fluid in both eyes (See Figure 2). A systemic workup including a CBC, CMP and coagulation studies was also obtained. It was remarkable for renal failure (creatinine 1.5), anemia (hemoglobin 8.1), and thrombocytopenia (platelets 8,000).
The patient was admitted to the medical service at Thomas Jefferson University Hospital for further management. Additional bloodwork demonstrated an elevated LDH (883), low haptoglobin (<10), and an elevated total bilirubin (1.6). All of these results indicated an ongoing hemolytic process, which was confirmed by the presence of schistocytes on the peripheral blood smear. Coagulation studies were normal, making a consumptive coagulopathy such as DIC less likely, and the presumptive diagnosis of TTP was made. Treatment with plasmapheresis and steroids was initiated and the diagnosis of TTP was later confirmed with an ADAMTS13 activity level, which was less than 1 percent.
|
Discussion
TTP is an acute syndrome that manifests as microangiopathic hemolytic anemia, thrombocytopenia, acute renal insufficiency, neurologic abnormalities and fever. With advancements in medical treatment, the above pentad is rarely seen in a single patient. It is caused by low levels of ADAMTS13, a metalloprotease involved in hemostasis. With decreased ADAMTS13 activity, platelets aggregate and form complexes that lead to microthrombosis and hemolysis.1 Before the 1970s, TTP was almost universally fatal. Since that time, improvements in diagnosis and management have reduced the mortality rate to 40 percent.2 First-line treatments include steroid therapy and plasmapheresis. IVIG and other immunomodulatory therapies are second-line options.
The incidence of TTP in pregnancy is only one in 25,000, but 10 to 25 percent of all patients diagnosed with TTP are pregnant or recently post-partum.3,4 As a result, these patients may be initially misdiagnosed with an obstetric complication, such as pre-eclampsia or HELLP syndrome.5 Pregnancy has been shown to decrease the levels of ADAMTS13, precipitating TTP in patients who have below-normal levels of this enzyme.1,6
Ocular involvement is seen in 14 to 20 percent of all patients with TTP.7,8 Although our patient presented with visual complaints, they usually develop in the later stages of the disease.6 These complications may vary widely. Serous retinal detachments are the most common manifestation of TTP, but choroidal bleeding, macular infarction, occlusions of the central retinal artery and vein, Purtscher-like retinopathy, and cortical infarcts resulting in visual field defects, diplopia and cortical blindness have also been reported.9 Although the exact pathophysiology is unknown, serous retinal detachments are thought to be related to the formation of microthrombi in the choroidal vasculature. Ischemic injury to the retinal pigment epithelium leads to a breakdown of the blood-retinal barrier, reduced resorption of subretinal fluid and subsequent serous retinal detachments.9 Hypertension, if present, may also contribute to choroidal vascular damage and retinal pigment epithelial tears.7 Most case reports have shown that plasmapheresis will result in complete resolution of the retinal detachment and any visual deficits, usually in days, demonstrating excellent prognosis with prompt treatment.8,10,11 REVIEW
The authors would like to thank Bill Benson, MD, of the Wills Eye Hospital Retina Service, for his time and assistance in preparing this case report.
1. Tsai HM. Pathophysiology of thrombotic thrombocytopenic purpura. Int J Hematol 2010;91(1):1-19.
2. Kremer Hovinga JA, Meyer SC. Current management of thrombotic thrombocytopenic purpura. Curr Opin Hematol. 2008;15:445-450.
3. Ezra Y, Rose M, Eldor A. Therapy and prevention of thrombotic thrombocytopenic purpura during pregnancy: A clinical study of 16 pregnancies. Am J Hematol 1996;51(1):1-6.
4. George JN. The association of pregnancy with thrombotic thrombocytopenic purpura-hemolytic uremic syndrome. Curr Opin Hematol 2003;10(5):339-44.
5. Lucania G, Camiolo E, Carmina MG, et al. Multidisciplinary approach in pregnancy-associated thrombotic thrombocytopenic purpura: A case report. Blood Transfus 2014;12 (Suppl 1):s137-40.
6. Lambert SR, High KA, Cotlier E, et al. Serous retinal detachments in thrombotic thrombocytopenic purpura. Arch Ophthalmol 1985;103:1172-4.
7. Harris JA, Friedman MT, Varma M. Unilateral serous retinal detachment in a patient with thrombotic thrombocytopenic purpura. J Clin Apher 2008;23(3):116-7.
8. Bobbio-Pallavicini E, Porta C, Brocchieri A, et al. Ocular involvement in acute thrombotic thrombocytopenic purpura. Haematologica 1995;80(2):194-5.
9. Kovács EM, Molvarec A, Rigó J Jr, et al. Bilateral serous retinal detachment as a complication of acquired peripartum thrombotic thrombocytopenic purpura bout. J Obstet Gynaecol Res 2011;37(10):1506-9.
10. Slusher MM, Pugh HP, Hackel RP. Bilateral serous retinal detachment in thrombotic thrombocytopenic purpura. Arch Ophthalmol 1990;108:744-5.
11. Zhao C, Qu Y, Sui R, et al. Delayed visual recovery in pregnancy-associated thrombotic thrombocytopenic purpura with bilateral serous retinal detachment. Doc Ophthalmol 2013;126(2):163-9.