 |
| Figure 2. UBM of the right eye showing a large anterior-posterior lens diameter and plateau iris configuration with a shallow anterior chamber. |
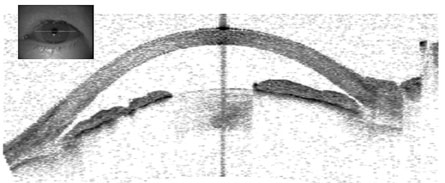 |
| Figure 3. Anterior segment OCT of the right eye illustrating a shallow anterior chamber, large lens and narrow angles. |
The patient was given IV mannitol, IV diamox, dorzolamide-timolol, brimonidine and prednisolone in the right eye. Two hours later her intraocular pressure was 40 mmHg. She was admitted to the hospital and given additional IV mannitol. Four hours later the intraocular pressure was 15 mmHg. After 24 hours, her pressure rose to 26 mmHg. After addition of pilocarpine, her pressure stabilized at 15 mmHg. She was subsequently discharged home on pilocarpine, dorzolamide-timolol and prednisolone in the right eye. Pilocarpine was also added to the left eye for prophylaxis.
The patient followed up in the Wills Eye Glaucoma Clinic two days later, at which time BCVA in the right eye was markedly improved to 20/60. Intraocular pressure in the right eye was 10 mmHg. Slit-lamp examination of the right eye revealed corneal edema, pigment on the inferior endothelium, and pigment and 1+ flare in the anterior chamber. Gonioscopy of the right eye showed an angle configuration of B20p. The left eye examination had not changed, except her angle had opened up to (B)C20p. The patient was observed and continued on topical pressure lowering medications.
The patient returned 13 days after initial presentation for follow-up. Intraocular pressure in the right eye was noted to be 15 mmHg. Slit lamp examination of the right eye was unchanged from the prior visit, except for mild improvement in corneal edema. The patient was comfortable and denied ocular pain. Ultrasound biomicroscopy (UBM) and anterior segment optical coherence tomography of both eyes was obtained at that visit (See Figures 2 and 3).
Right eye UBM revealed a plateau iris configuration. Anterior segment OCT illustrated narrow angles and a large lens displacing the iris forward. Therefore, the patient’s initial episode of angle closure glaucoma was the result of a combination of plateau iris syndrome and phacomorphic glaucoma.
Her intraocular pressure was observed closely until her eye was quiet enough for cataract surgery. She was also offered cataract extraction in the left eye in order to decrease her risk for acute angle closure.
| Gonioscopy shows the classic "double-hump" sign, with the peripheral hump created by the ciliary body pushing the iris root forward and the central hump created by the iris sitting on top of the anterior lens capsule. |
Plateau iris configuration is an anterior displacement of the ciliary body that mechanically pushes the iris root into close approximation to the trabecular meshwork. Plateau iris syndrome is persistent angle occludability despite a patent peripheral iridotomy. Plateau iris syndrome is a recognized cause of secondary angle closure glaucoma typically seen in younger female patients who are less hyperopic than most patients with narrow angles. Plateau iris configuration tends to run in families. Slit-lamp examination shows a deeper central anterior chamber with a shallow peripheral chamber. Gonioscopy shows the classic “double-hump” sign, with the peripheral hump created by the ciliary body pushing the iris root forward and the central hump created by the iris sitting on top of the anterior lens capsule.
Plateau iris syndrome can be managed in several ways. Conservative management includes use of topical pilocarpine to pull the iris away from the trabecular meshwork and increase meshwork outflow. Argon laser peripheral iridoplasty, on the other hand, uses laser burns to the iris periphery to cause iris scarring. Subsequent contraction then pulls the iris away from the trabecular meshwork. Phacoemulsification with intraocular lens implantation is also a viable primary treatment for chronic angle closure glaucoma caused by plateau iris or as treatment for persistent angle closure after peripheral laser iridotomy.
The author would like to thank George Spaeth, MD, of the Wills Eye Institute Department of Glaucoma, for his time and insight.
1. Etter JR, Affel EL, Rhee DJ. High prevalance of plateau iris configuration in family members of patients with plateau iris syndrome. J Glaucoma 2006;15:394-398.
2. McKibbin M, Gupta A, Atkins AD. Cataract extraction and intraocular lens implantation in eyes with phacomorphic or phacolytic glaucoma. J Cataract Refract Surg 1996;22:633-636.
3. Lam DS, Leung DY, et al. Randomized trial of early phacoemulsification versus peripheral iridotomy to prevent intraocular pressure rise after acute primary angle closure. Ophthalmology 2008;115:1134-1140.
4. Jacobi PC, Dietlein TS, et al. Primary phacoemulsification and intraocular lens implantation for acute angle-closure glaucoma. Ophthalmology 2002;109:1597-1603.
5. Nonaka A, Kondo T, et al. Cataract surgery for residual angle closure after peripheral laser iridotomy. Ophthalmology 2005;112:974-979.



