As myopia rates rise around the world, the condition has increasingly been referred to as an epidemic, a disease and a public health crisis in the making. Myopia can lead to pathology and vision loss when it’s severe, but the majority of cases don’t stray into pathologic levels and can safely be addressed with corrective lenses or refractive surgery. Some ophthalmologists feel that broadly applying the term “disease” to myopia may not always be appropriate for a condition whose affected majority isn’t at high risk.
On the other hand, the global prevalence of myopia is rising, and with it the proportion of individuals with high myopia who would be at risk for future retinal detachments or other conditions such as lattice degeneration and glaucoma. The COVID-19 pandemic lockdowns and stay-at-home orders have also exacerbated this rising trend,1 with an entire generation of young children seeing more screens than trees for the past few years. Myopia, whether severe or not, also entails a heavy economic burden. Eye care services around the world will be pressed to meet this growing need.
Should myopia be referred to as a disease though? The answer is nuanced, experts say. Bioethicist and pediatric ophthalmology subspecialist Alex V. Levin, MD, MHSc, FRCSC, and the Massachusetts Eye & Ear Infirmary’s Grayson W. Armstrong, MD, MPH, discuss myopia’s classification and how this may drive clinicians’ decisions regarding interventions.
 |
|
Studies show that sunlight exposure can help slow myopia progression.3-5 |
Classifying Myopia
“I’m a bit troubled when people refer to myopia as an ‘epidemic,’ because I’m not sure it’s always a disease,” says Dr. Levin, who also holds the Adeline Lutz – Steven S. T. Ching, MD, Distinguished Professorship in Ophthalmology and is chief of pediatric ophthalmology and ocular genetics at the Flaum Eye Institute and chief of clinical genetics at the Golisano Children’s Hospital at the University of Rochester Medical Center.
“Singapore’s Ministry of Health projects that 80 to 90 percent of all Singaporean adults will be myopic by the year 2050, with 15 to 25 percent of those individuals having high myopia. When almost everyone in a population has a condition, is it still a disease?” he asks. “If there’s no risk for a complication other than the fact an individual dislikes something about their uncorrected vision, can you call that a disease?
“Some people are dissatisfied by their inability to see the alarm clock in the morning. Other individuals are upset about the size of their nose,” he continues. “Both could choose to have a surgical procedure to relieve this ‘dis-ease.’ I don’t consider lower levels of myopia to be a disease category but rather a variation of normal. In medicine, we have to separate when we’re treating a medical problem that has clear, definable adverse outcomes from when we’re treating the preferences of a patient.”
When It’s Not Axial Lengthening “As we discuss disease and myopia classification, it's worth mentioning that some systemic medical conditions can lead to nearsightedness,” says Grayson W. Armstrong, MD, MPH, of the Massachusetts Eye & Ear Infirmary. “If an older patient who hasn’t had myopia previously presents with sudden onset of new myopia, that patient may be diabetic and their blood sugar may be high, causing the lens in their eye to swell, leading to a myopic shift. Those patients will come in with acute blurring and have a lot of trouble seeing far away, but if you just prescribe them glasses, they’re going to be walking around with diabetes that could be treated.” He notes that acute nearsightedness may also arise from other conditions including retinitis pigmentosa, Marfan syndrome, Stickler syndrome and Ehlers Danlos syndrome. |
“We know that there are genetic associations with myopia so it can be inherited like a disease, and we know that there are modifiable risk factors for it such as screen time, outdoor time and type of glasses or contacts,” says Dr. Armstrong, a Harvard Medical School instructor in ophthalmology, associate director of medical student education and director of the Massachusetts Eye & Ear ophthalmology emergency services. “But most myopia isn’t a disease,” he agrees. “Anything that causes pathology and leads to vision loss, blindness or surgical intervention is a disease, whereas if you’re correcting someone’s vision with glasses and that’s enough, and there are no risks of future sight-threatening complications, then that shouldn’t be classified as a disease.”
What To Do About Rising Rates?
Almost 30 percent of the global population is myopic with only about 4 percent highly myopic, but by 2050, these numbers are projected to increase to nearly 50 percent with 10 percent high myopes, according to the Brien Holden Vision Institute.2
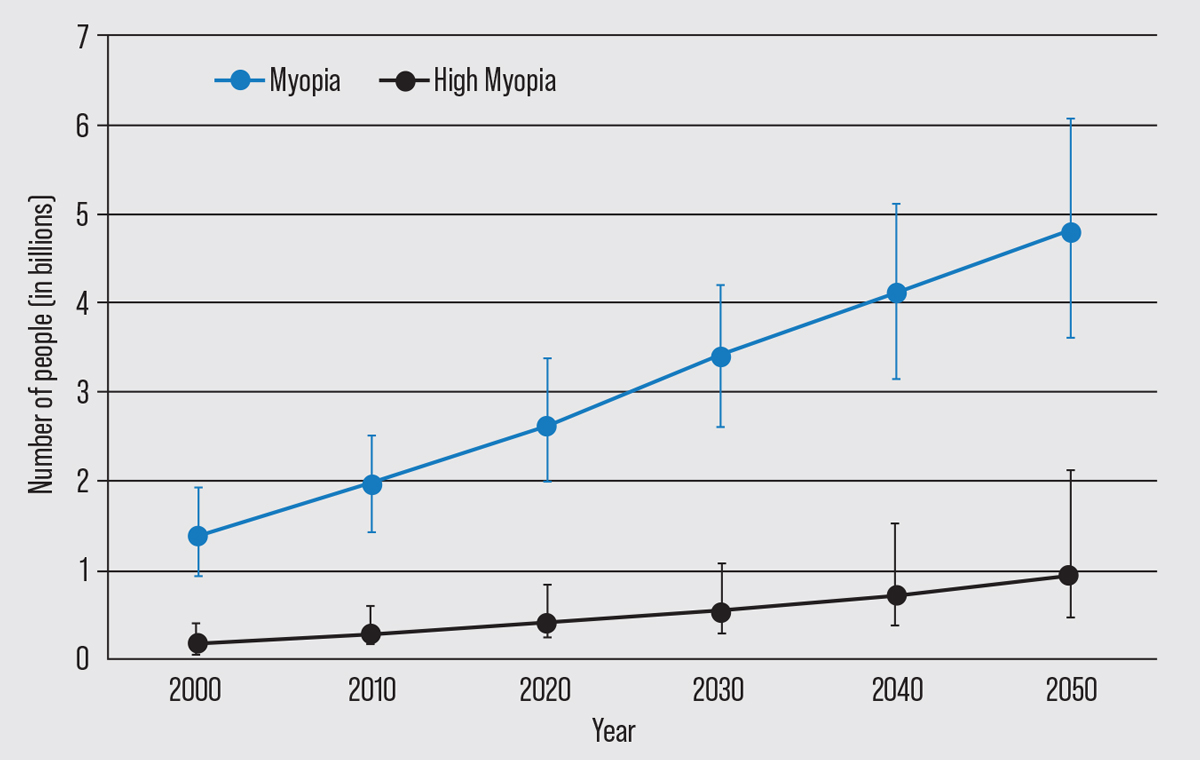 |
| In 2050, an estimated five billion people (50 percent of the global population) will have myopia and one billion will have high myopia (10 percent), according to the Brien Holden Vision Institute’s pre-pandemic 2016 estimate.2 (Adapted from Holden et al. 2016.) |
Uncorrected refractive error is a major and growing cause of vision impairment around the world. As myopia rates rise, there will be more individuals seeking refractive surgical correction. Certainly, interventions such as elective refractive surgeries like LASIK and clear lens exchange can address myopia, Dr. Levin points out. “These procedures don’t prevent medical problems, though,” he says. “With refractive surgery, the best-corrected 20/20 patient with a healthy eye that just happens to be longer than average, is submitting that eye to the risks of refractive surgery—which could include an increased risk of retinal detachment—for the convenience (or necessity in some cases) of not wearing glasses or contact lenses.
“If there were a way to prevent people from getting into the axial length categories that put them at high risk for retinal detachment and we had a treatment that was shown to effectively reduce the rate of retinal detachment from myopia, that would be fantastic,” Dr. Levin continues. “However, I’m not sure we can confidently prevent a -1 D myope from becoming a -8 D myope—yet. For pathologic myopia, which seems at least in part to be independent of axial length and likely a genetic disorder, our current therapies are likely even less effective.”
“I think one reason myopia is so often called an epidemic is because the number of myopes is rising,” says Dr. Armstrong. “In Taiwan, close to 80 percent of children are myopic now. A large portion of these children will hopefully go on to live normal lives without a risk of retinal detachment or tears. It’s perhaps worth monitoring myopia as a risk factor for disease but it’s not necessarily true that all 80 percent of those Taiwanese children has a disease from an early age.
“That said, we can’t always predict which of those children will go on to be highly myopic or which ones will need retinal detachment surgery or go blind from a choroidal neovascular membrane in the future, so we may want to monitor and/or treat them all as if they could be that patient,” he says. “We do know that the younger a child is when they become myopic, the greater the chance they have of becoming a high myope.”
This raises the question of potential intervention benefits and trade-offs. Dr. Armstrong notes that there’s some evidence for increasing outdoor time and limiting screen time as a management strategy. “Though children may still progress despite increased outdoor exposure, this intervention’s positive benefits extend beyond the eyes to the entire body,” he says.
Findings from the Sydney Myopia Study suggest that outdoor exposure alone is enough to have an effect on myopia progression. (Indoor sports weren’t associated with myopia reduction.)3 In the study, higher levels of outdoor activity were associated with more hyperopic refractions and lower myopia prevalence in 12-year-olds; no consistent associations were noted between refraction and activity in the 6-year-old group. Light intensity, increased depth of field and decreased image blur were suggested as contributing factors. The researchers also noted that light may affect retinal dopamine release, an eye growth inhibitor.
Similarly, a study in which children wore wrist light sensors reported that those who experienced low amounts of daily ambient light had significantly greater eye growth than children who experienced moderate or high levels of light exposure.4
A study in Taiwan reported that increasing outdoor activities and sunlight exposure in school was effective at slowing myopia progression. The researchers also reported that shorter outdoor time with high bright light exposure had an effect on myopia progression comparable to longer outdoor time with moderate light exposure.5
“While outdoor time isn’t as effective as low-dose atropine eyedrops, eyedrops also aren’t 100-percent effective in preventing high myopia in all children,” Dr. Armstrong notes. “There are certain risks associated with atropine eyedrops too, such as blurred vision and decrease in accommodative ability. If there’s an accidental overdose, there may be systemic issues such as flushing, fever and trouble urinating.”
Dr. Armstrong believes all children should be screened for glasses at a young age. “It’s very important for quality of life and school success,” he says. “If children can’t read the board, they won’t do as well in school. This is a small intervention with low risk. Defocus contact lenses and orthokeratology lenses may also potentially help with myopic progression, though these interventions aren’t risk-free. Contact lenses can lead to corneal ulcers if the lenses aren’t removed at night or aren’t cleaned regularly.”
While interventions have some associated risks and disadvantages, including cost, myopia intervention has been shown to significantly impact refraction and axial length.6 A review of randomized clinical trials reported that a range of interventions reduced myopia when compared with placebo. The paper reported that atropine, pirenzepine and progressive-addition spectacle lenses were effective in terms of refractive correction; and atropine, orthokeratology lenses, peripheral defocus-modifying contact lenses, pirenzepine and progressive-addition spectacle lenses were effective in terms of axial length.
Overall, they concluded that pharmacologic interventions (atropine and pirenzepine) were most effective; some specially designed contact lenses (ortho-K and peripheral defocus-modifying contact lenses) had moderate effects; and specially designed spectacle lenses had a minimal effect.
The ability to retard the progression of myopia may be crucial for avoiding more serious ocular problems down the road. One study reported that a 1-D increase in myopia was associated with a 67-percent increase in the prevalence of myopic maculopathy.7 The group reported that slowing myopia by 1 D should reduce the likelihood of developing myopic maculopathy by 40 percent, regardless of the level of myopia. Low and moderate levels of myopia, though less prone to complications than high myopia, still carry “considerable risks” for myopic macular detachment, retinal detachment, posterior subcapsular cataract, nuclear cataract and open-angle glaucoma, according to a 2020 review study.8
Effects of Labels
Dr. Armstrong notes that broadly classifying myopia as a disease may serve some public health aim. “Other public health experts may disagree, but it’s possible that if you categorize something as a disease it could be easier to track or find funding for research, though that’s a separate argument,” he says. “Calling it a disease also gets people’s attention, perhaps making them less likely to blow it off and assume their child only needs glasses.”
On the other hand, he says it could be stigmatizing to call every single person in the world who has some level of myopia a diseased patient. “We can try to control myopia as if it’s a preventable disease,” he says. “But once patients get out of that risk zone—when they reach a certain age and don’t have high myopia—I personally wouldn’t say that person is diseased. On the other hand, someone with high myopia should perhaps be monitored as if they have a disease.
“From a clinical standpoint, if I see a patient with one diopter of myopia, I don’t consider them as having a disease per se,” he continues. “If that child is six months old and they’re already two or three diopters myopic and I see them again and they’re a four-diopter myope, then to me that rate of decline at that early age at onset is a very bad prognostic indicator that that young child is probably going to have worse outcomes and a risk of high myopia. It has to be put into context.”
Looking to the Future
“We as a medical community are still learning why myopia occurs and what the best treatments are,” Dr. Armstrong says. “While studies have shown that we’re beginning to figure out the genetic causes, and we have found ways to start treating it, nothing’s perfect and we can’t always predict who will have high myopia or worse outcomes. We’re not going to be able to treat everyone and prevent high myopia with the tools we have today.
“Researchers in the myopia space will need to focus on myopia as if all of it were a disease and treat the patients at the highest risk of developing high myopia and related complications, as well as find ways to treat it before it reaches that point,” he continues. “These future treatments won’t apply to a patient who’s, say, a half-diopter myope at age 12 but they may be appropriate for children with four or five diopters of myopia who are really at risk of developing complications later in life.
“Ultimately, we have to take each case very seriously and focus on the disease aspects of myopia,” he says. “If we can pinpoint ways to curb the rates of myopia in those countries, then hopefully we can lower the rates of high myopia and associated vision-threatening conditions that come down the road. Myopia can have incredibly devastating consequences for people’s vision, quality of life, economic productivity and family. There are serious potential outcomes, so we should take the condition seriously and treat it with what we can.”
Dr. Armstrong and Dr. Levin report no related financial disclosures.
1. Kurupp ARC, Raju A, Luthra G, et al. The impact of the COVID-19 pandemic on myopia progression in children: A systematic review. Cureus 2022:14:8:e28444. [Epub August 26, 2022].
2. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology 2016;123:5:1036-42.
3. Rose KR, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 2008;115:8:1279-1285.
4. Read S, Collins M, Vincent S. Light exposure and eye growth in childhood. Invest Ophthalmol Vis Sci 2015;56:6779-87.
5. Morgan IG. Myopia prevention and outdoor light intensity in a school-based cluster randomized trial. Ophthalmology 2018;125:8:1251-2.
6. Huang J, Wen D, Wang Q, et al. Efficacy comparison of 16 interventions for myopia control in children: A network meta-analysis. Ophthalmology 2016;123:4:697-708.
7. Bullimore MA and Brennan NA. Myopia control: Why each diopter matters. Optom Vis Sci 2019;96:6:463-465.
8. Haarman AEG, Enthoven CA, Tideman JWL, Tedja MS, Verhoeven VJM, Klaver CCW. The complications of myopia: A review and meta-analysis. Invest Ophthalmol Vis Sci 2020;61:4:49.



