Preoperative Concerns
In the screening process, I try to set patients straight immediately, disabusing them of the notion that a refractive procedure will free them from their glasses. I also make them well aware of the risks involved, which will depend on how good a candidate they are.
Along the lines of informed consent, I will reel off the usual list of risks and complications, especially tailored to the particular patient's profile. After a discussion of any additional risks they may have, I have them write the specific risks they have in their own handwriting at the end of the consent form when the time comes to complete the document.
 |
| For bad cases of epithelial ingrowth, suturing can help stop the cells. |
If someone has dry eye when not wearing contacts that's bad enough to need treatment ahead of time, I usually won't perform laser vision correction on him or her. I'm also very conservative when it comes to inferior steepening on topography. I don't try to figure out if it's warpage from contact lenses or not. Instead, I will automatically choose LASEK in these patients if it is appropriate for them.
The risk factors I personally look for when assessing the risk of postop halos are large pupils, high prescriptions (above -6 D) and astigmatism above 2 D. If they have any of these risk factors or a combination of them, I will spend more time discussing halos with them.
I highly recommend custom ablations on patients with large pupils or with astigmatism greater than 2 D, because, with the Visx laser I use, the astigmatic optical zone is somewhat smaller with the conventional treatment than with the CustomVue treatment. I believe this larger optical zone decreases their risk for halos.
The Procedure
To prepare the patient for LASIK, we avoid instilling any tetracaine until right before the procedure to decrease the risk of epithelial defects, but for LASEK instilling it beforehand is probably recommended, because it loosens the epithelium a bit. We also give antibiotic drops to the patients when they come in.
For LASIK, I always measure the intraocular pressure intraoperatively with a pneumotonometer. I don't rely on finger palpation or whether the patient has lost vision. I also don't like to use the Barraquer tonometer, because it only gives you an indication of a pressure of
60 mmHg, while the pneumotonometer will give you an indication of 80 mmHg and above. When I put the suction ring on, if it's a superior hinge, I'll decenter the ring a little superiorly; I'll decenter it nasally for a nasal-hinged flap. Decentering the ring gives a little more room for the ablation. I always mark the cornea to ensure proper apposition and orientation of the flap and avoid any folds.
I prefer to make large, 9-mm, flaps. You'll find that a large flap is useful for several reasons: If a patient has an overcorrection postop, he already has a large flap to accommodate a hyperopic treatment. The edge of the flap is also farther away from the visual axis, so when it comes to epithelial ingrowth or diffuse lamellar keratitis that creeps in from the periphery, I will have more time to intervene. Also, if I have to place sutures at the flap edge, they will be farther from the axis. Furthermore, since the flap is closer to the limbus, it adheres better and is less prone to traumatic dislocation than a smaller one, and it's also much more forgiving to a decentered cut, since the bed is larger.
After cutting the flap, I dry the bed and do the procedure. Then I irrigate the bed completely with BSS and put the flap back down. After this, I squirt a small amount of BSS beneath the flap, then pass the cannula over the flap to squeeze out the fluid. I then dry the gutter with a methylcellulose sponge. Some surgeons don't like to wet the stromal bed with BSS, thinking that it swells the flap and gives them a bigger gutter. I found that isn't the case, because I use the same technique for enhancements but then there is no gutter. The flap swells because of the keratome pass, not because you've irrigated the bed.
I'll then place a contact lens if it's an enhancement, otherwise I won't place one. Also, with enhancements, if there are any epithelial tags, it helps to make sure they're draped over the flap rather than under it, to avoid epithelial ingrowth.
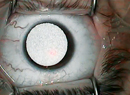
 |
| If diffuse lamellar keratitis gets beyond stage 2 (shown here), Dr. Melki will lift and irrigate the flap. |
For LASEK, which I use for about 35 to 40 percent of refractive surgery candidates, I use a particular method for epithelial debridement that's different from what most surgeons use. We delaminate the epithelium mechanically after applying the alcohol, using a LASIK flap lifter that's nudged under the epithelium, separating it from the underlying Bowman's layer in a manner similar to lamellar dissection. This gives a very nice flap that's similar to those made with epi-LASIK without having to use the epi-LASIK separator. It gives intact epithelial flaps about 90 percent of the time.
Postop Topics
I have LASIK patients wait about 20 minutes, then examine them again to make sure the flap is sitting well. They start their drops about four hours later (prednisone q.1.h. for two days, then q.i.d. for two days; antibiotic drops q.i.d. for four days). With LASEK patients, we place the contact lens and have them go home without the 20-minute check.
Here is how I approach some common postop LASIK issues:
• Striae. If I see these on postop day one, I'll refloat the flap, wait an hour and re-check. If there's an improvement I'll also check the patient the next day.
If folds persist, I classify folds into two groups: visually significant and non-visually significant. For the former, in the first week postop, I'll try to refloat the flap and iron it out. If that doesn't work, I'll perform some epithelial debridement in the area of the fold. The debridement is necessary because there will be crevasses that have become filled with epithelium. If you try to stretch the flap, it won't work, because the epithelium is acting like a glue. When you debride the epithelium though, you'll find the flap easier to stretch.
If debridement and stretching don't work, I'll place sutures to smooth out the flap.
• Diffuse lamellar keratitis. I don't see this as often now, presumably because of my postop steroid regimen. If I do see a case, I have a low tolerance for it. If it gets beyond stage 2, I'll lift and irrigate the flap. Fortunately, if DLK doesn't worsen in the first three or four days, it will most likely amount to nothing.
• Epithelial ingrowth. I observe this closely to make sure it's not progressing. I'll stain the eye with fluorescein, with any pinpoint staining at the edge of the flap indicating an area of cell infiltration. I try to avoid lifting the flap as much as possible, because that can lead to a vicious cycle: You lift the flap and scrape the cells and then the flap gets a little edematous. The flap swelling raises the edges a little and more cells infiltrate, etc. However, if I have to, I will lift and scrape. I also won't hesitate to place sutures to stop the infiltration, making sure to put sutures around the edges, with a couple extra in the area of the ingrowth. Usually, these methods can quell the cells.
Dr. Melki is an associate surgeon at the Massachusetts Eye and Ear Infirmary and is founder of the Boston Eye Group, his private practice.