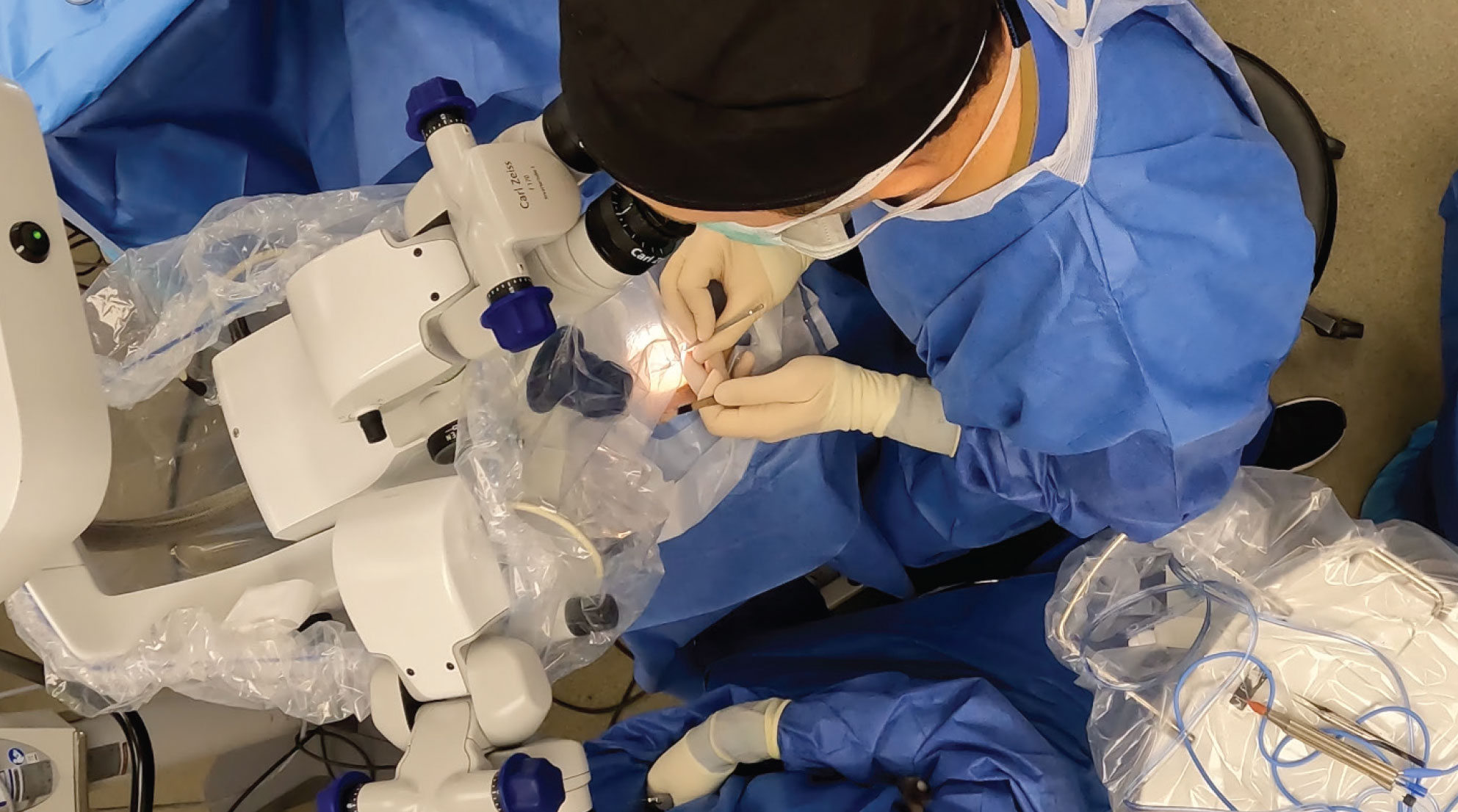
The advent of technology and video sharing platforms has provided immeasurable benefits to the training and education of surgeons worldwide. They can find almost any technique online with a closeup view of instruments entering the eye and how to maneuver them. And although this has become the standard way to demonstrate technique, there’s a new methodology emerging in the field that advocates for zooming out and showing more of the surgeon and their particular positions and movements to achieve any given technique.
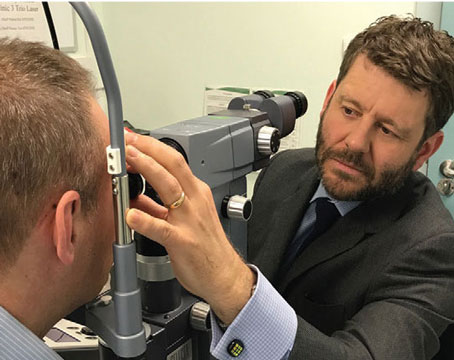
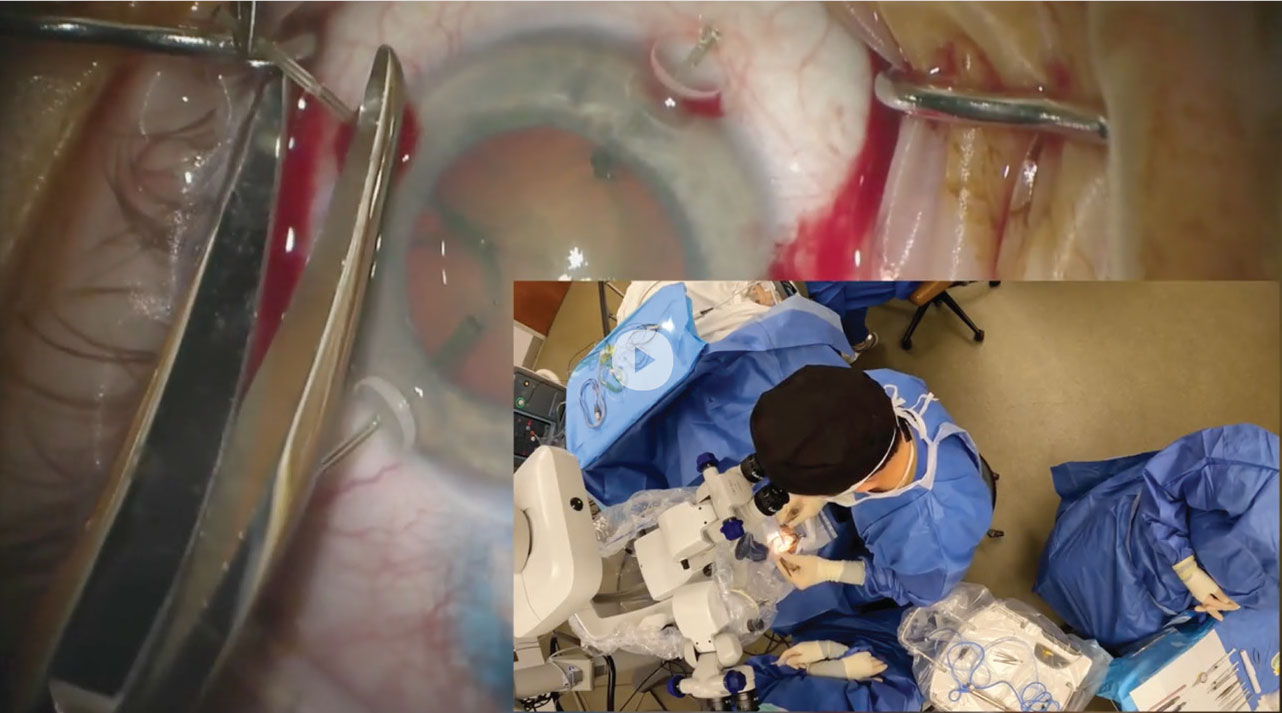
We spoke with Brandon Ayres, MD, co-director of the Cornea Fellowship Program at Wills Eye Hospital, and a proponent of this updated video style, who also plans to release a series of videos on YouTube in the coming months. Along with detailing the benefits of this style, he shared some photos of unique grips and hand positions as a preview of what to expect.
Why the Angle Matters
According to Dr. Ayres, watching surgeries solely from the surgeon’s point of view (looking through the microscope) can be misleading for those hoping to learn from it.
“Sometimes those videos can make something look easy, but the viewer has no idea what’s going on outside of the eye,” Dr. Ayres says. He has witnessed the fellows in his program step away from the scope for additional angles.
“I often find, as the year goes on, our fellows stop watching what’s going on at the scope to some degree and start watching for more of the finer points of the surgery. They’ll ask why a Yamane technique takes them an hour, yet takes me only five minutes, for example. And it’s because of the angles of the instruments and how I may be holding them differently,” he says.
It’s not uncommon for surgeons to switch instruments from one hand to another, Dr. Ayres continues. “There’s certain times when we’re doing iris repairs where I’m suturing with my left hand versus my right hand and back and forth, but that doesn’t transfer on the screen through the microscope. You can’t really tell which hand is holding an instrument unless you’re really looking closely,” he says.
Dr. Ayres believes that fellows and residents can gain a better understanding of the intricacies of cataract surgery when they see the economy of motion outside of the eye. “It’s about how you’re grabbing, how you’re moving your hands—that’s where the magic is. It’s not what’s going on inside the eye, it’s how you’re managing the instruments in the sutures outside the eye,” he says.
He was encouraged to continue pursuing this when Ike Ahmed, MD, who practices at the University of Utah’s Moran Eye Center, mentioned this topic during a session they paneled at the 2022 American Academy of Ophthalmology meeting. “We’re both on a similar mission to show surgery from different perspectives, not just hands but our feet as well,” Dr. Ayres says. “I think this is really how surgeons can learn these more advanced techniques because it’s more than just making a hole and putting an instrument through it.”
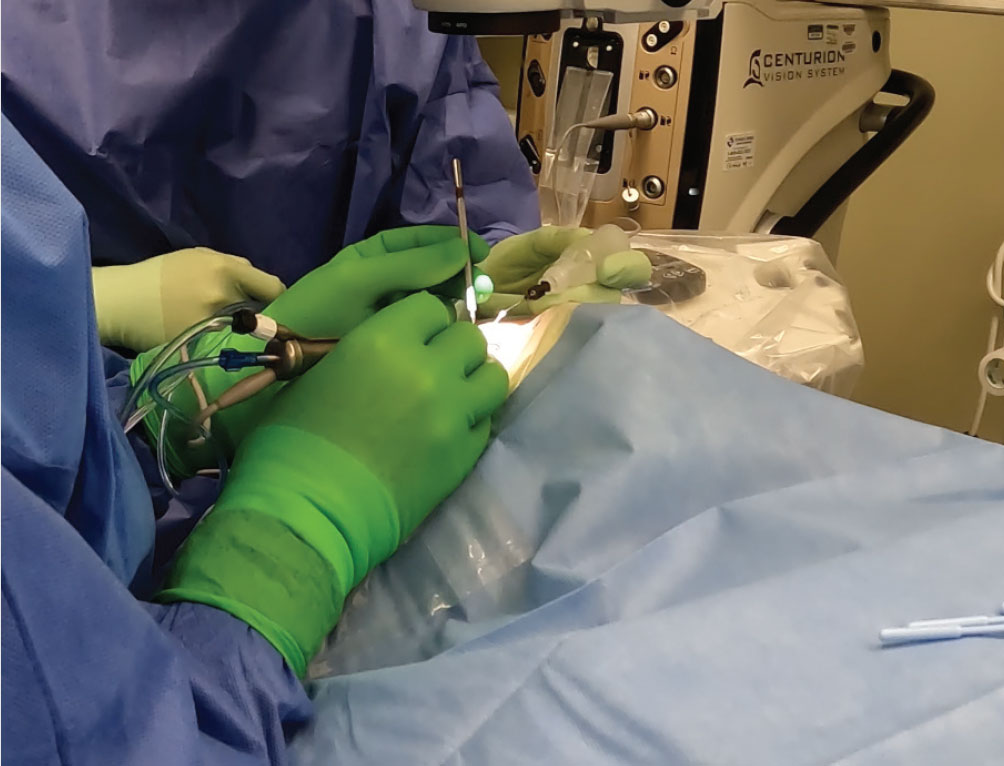
Typical Phaco Position | Phaco Position (another angle) |
 |  |
| |
The Importance of Being Flexible
Although there are “default” or “traditional” grips and positions that every surgeon learns, physicians make tweaks as their careers progress. Dr. Ayres advises that surgeons must be willing to be flexible.
“Very often when I’m operating with fellows or residents, they sort of get locked into the idea that you’ve got one main incision and one paracentesis and you have to do all of the surgery through that, so I think there’s adjustments to be made not just in holding instruments, but also the approach,” he says. “Maybe it’s okay to have two or three paracenteses, so you’re not locked into just a paracentesis and a main. And I hold my instruments all different ways, in unorthodox grips. There are times when I don’t know how I’m going to get an instrument where I need it, but then I change my grip or move my hand and suddenly it makes more sense. I do things completely differently than when I first started, and a lot of that is because surgery itself is progressing, so your technique is bound to change.”
Since making these videos, Dr. Ayres realizes how many unconscious tweaks and maneuvers he makes during surgery. “It’s been really interesting to see what happens during these complex cases. I realize how I place my pinkie finger on the patient’s forehead to support my hand to reduce tremor, and I don’t know that I ever noticed that in the moment,” he says.
| When things become more complicated, Dr. Ayres says he has to think outside the box: |
| Bracing One Hand with the Other |
 |
|
| Cerclage and Left Hand Suture Grip |
 |
|
Underhand MST Grip | |
 | |
Underhand Grip (another angle) | Vent Incision |
 |  |
|
|
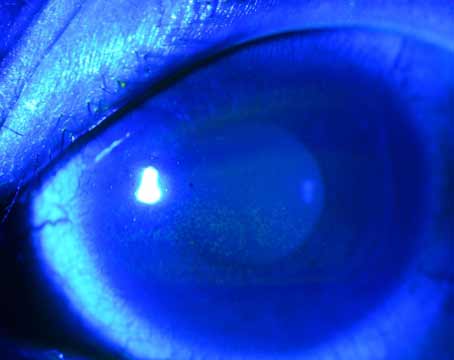
| Complex Cataract Extraction with Pars Plana Vitrectomy (Surgical Video Screen Shots) |
 |
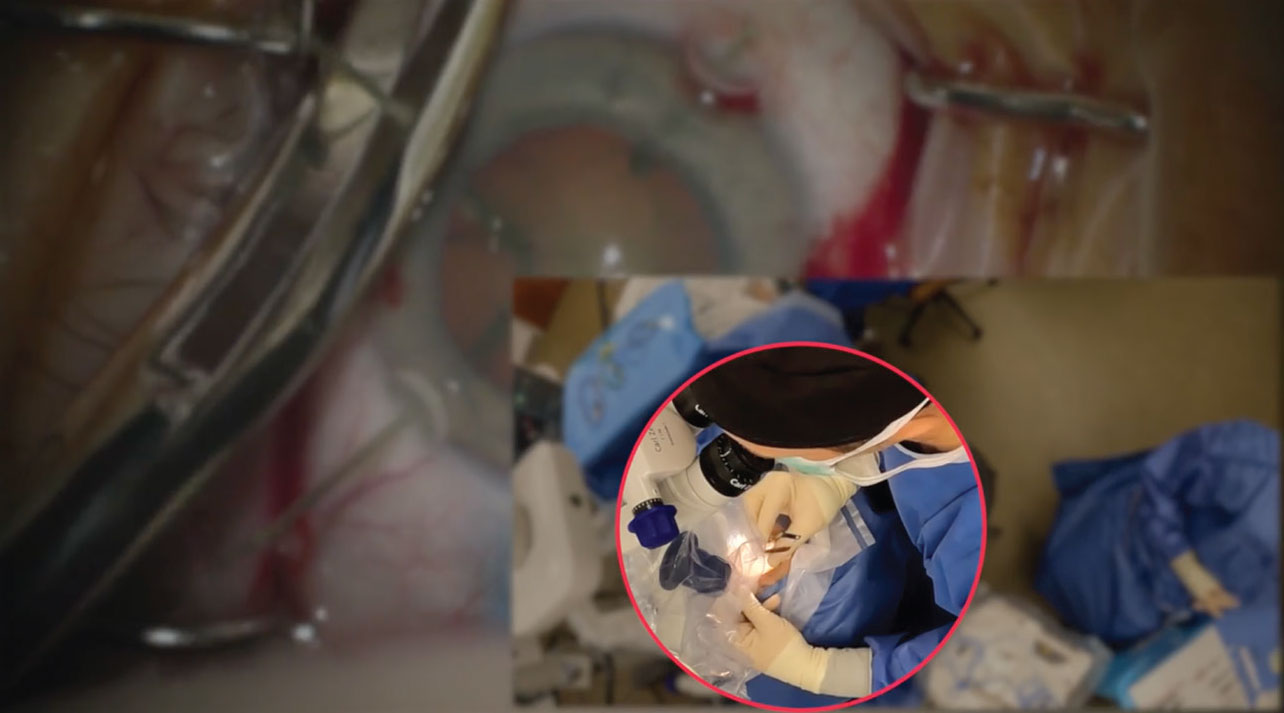 |
In a soon to be published video, Dr. Ayres highlights the “strange” way he holds instruments during this procedure. |
Dr. Ayres has no financial disclosures related to this topic.