Standard automated perimetry has been the gold standard for evaluating a patient’s visual field for many years. The information it provides is crucial to monitoring the status of our glaucoma patients, and it often allows us to detect functional deficits before an individual notices any loss. Without this data, the disease may progress to a point at which it’s difficult to help the patient maintain the good vision that’s left, before the patient even realizes that a serious problem exists.
Every ophthalmologist understands that standard automated perimetry, such as a Humphrey visual field test, isn’t an easy test to take—or to give. It requires the patient to remain fixated on a visual target for several minutes at a time, suppressing the foveation reflex that makes us want to look directly at a new visual stimulus. And it’s not entertaining in any way that might offset the discomfort and mild stress associated with taking the test. That’s undoubtedly why we’ve all listened to patient complaints about having to take the test. Furthermore, from the practice’s perspective, it requires a fair amount of a technician’s time to ensure that the patient understands how to take the test and does so in a reliable way that produces meaningful data.
 |
| Standard visual field testing requires patients to suppress the foveation reflex—the desire to look directly at a new visual stimulus. In contrast, in this oculokinetic virtual reality test patients look directly at any new visual stimulus they’re able to see. When the system detects that the patient is looking at it, it becomes the new fixation point. The software uses the data to map out the patient’s visual field. Click image to enlarge. |
Given these realities, it should be no surprise that many researchers and companies are trying to develop an alternative way to test the visual field. During the past year, at the University of California San Francisco School of Medicine we’ve been developing a visual field test using virtual reality goggles in an unfunded collaboration with the company Vivid Vision. (I’m not a consultant and have no financial involvement in any product that may result; and I’m aware that several other VR visual fields are currently available.)
This project, seen as a way to allow patients to perform home testing, was in the works prior to the pandemic, but COVID has definitely shed light on the importance of being able to care for your patients remotely. Because of the pandemic, I haven’t seen some of my patients for more than a year, and some are still nervous about coming in. Clearly, an affordable and effective way to test the visual field at home would offer significant benefits for glaucoma management, and not just during a pandemic. Such an option would help doctors monitor their patients in very rural areas in America and around the world, as well as in resource-poor areas, where glaucoma has an inequitable distribution, even when times are relatively good.
Incorporating the Foveal Reflex
As I mentioned earlier, one of the challenges when taking a standard visual field test is the need for fixation—remaining visually focused on one point and suppressing the foveation reflex. Eliminating the need to do that has been a key goal of the test we’re developing.
To that end, our test uses oculokinetic perimetry, which was developed many years ago by Bertil Damato, MD, PhD, an ocular oncologist. It’s called oculokinetic because the eye moves, following each new visual stimulus, instead of remaining fixated on one point. Virtual reality is ideally suited for this approach because there’s no restriction on the visual locations perceived by the patient. The virtual space literally surrounds the patient.
Other Virtual Reality Perimeters VisuALL S System perimeter (Keeler/Olleyes) olleyes.com or VirtualEye Perimeter (BioFormatix) bioformatix.com/perimetry.html PalmScan VF2000 Visual Field Analyzer (Micro Medical Devices) micromedinc.com/our-devices/palmscan-vf2000-visual-field-perimeter/ Advanced Vision Analyzer (Elisar) elisar.com. Virtual Field (Virtual Field) home.virtualfield.io |
During our test, when a stimulus is flashed, you allow your foveation reflex free rein, turning your head to look at each new stimulus point. A center circular light spot marks your focal point, so the game becomes moving your head so the dot in front of you overlaps with the target stimulus. The device can tell where you’re looking, so once it perceives that you’re looking directly at the latest stimulus, that becomes the fixation point for the next stimulus. If the next stimulus falls in a “blind” area, the patient doesn’t turn to look at it. If the patient does see it, he or she turns to look at it. Meanwhile, the device is using this data to map out the patient’s visual field. The fact that the patient gets to move freely makes this test much easier and more intuitive than the gold-standard Humphrey visual field test.
If the patient is using this device at home and has Wi-Fi, the device will try to connect to the internet before conducting the test. If it’s able to connect, it will check in the company’s database to see if the doctor has made any changes to the testing plan, such as changing from a 24-2 algorithm to a 10-2 test pattern. Then, whether or not the device is able to connect to the internet, it runs the test using the most recent instructions. All of the data from each test is saved locally on the device, and is then synced with the cloud. If the patient has Wi-Fi at home, this happens immediately; if not, the patient has to bring the goggles back to the doctor’s office, where the device connects to the clinic’s Wi-Fi network and immediately uploads the data to the cloud.
One question that remains unanswered is whether the software will end up incorporated into a specific pair of virtual reality goggles, or be made available as software only, able to work with any VR goggles. The potential to run on multiple systems certainly exists, but having the software associated with a single piece of hardware also offers the advantages of consistency, as well as putting less of a burden on the patient to locate the software online and load it into a device.
It’s worth noting that there are a number of non-VR visual field tests being developed that allow the patient to take the test on a flat computer screen or using something like an iPad. At least one of these also uses an oculokinetic perimetry test. However, these tests have a number of inherent potential problems. For example:
- It’s impossible to know for sure that the screen is at the right distance from the patient’s eyes for the stimuli to appear in the patient’s visual field at the location you think you’re testing.
- The ambient lighting conditions during the test can’t be controlled.
- You can’t be sure about the screen resolution, or the background luminance during the test. (These can be significantly different from device to device.)
Obviously, these factors are under control when a patient takes the Humphrey visual field test. They can also be controlled when the test is given using virtual reality goggles.
The Power of Frequent Testing
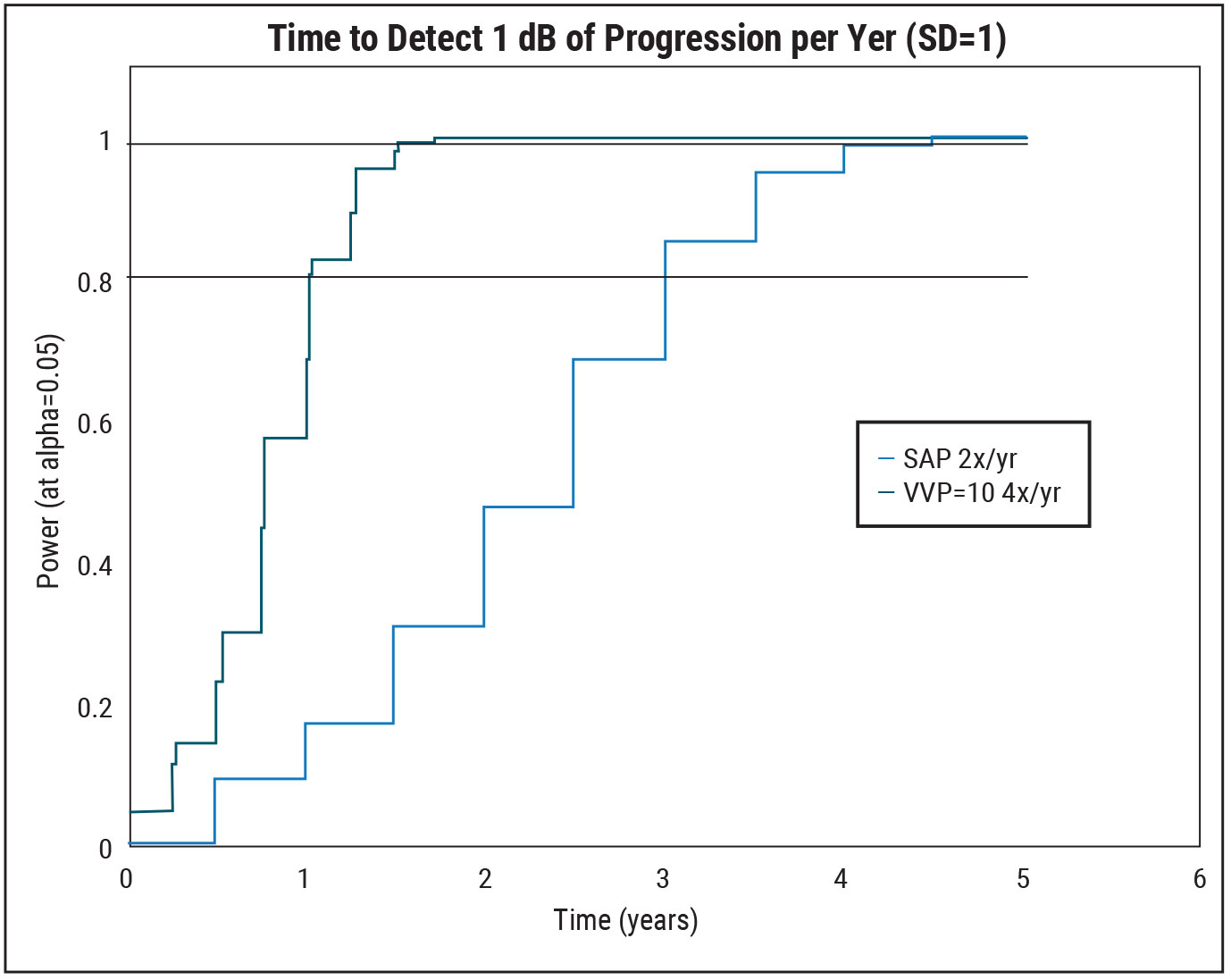 |
| Standard visual field testing is uncomfortable for the patient and has to be done in the office, making it difficult to do more than two tests per year. Patients don’t mind doing the virtual test at a rate of 40 times per year, and it can be done at home. This increased frequency of testing can detect rapid disease progression much more quickly. Click image to enlarge. |
Making visual field testing more pleasant and convenient for the patient is especially important for one reason in particular. As work done by Felipe Medeiros, MD, PhD, has demonstrated, the more often you’re able to test a glaucoma patient, the sooner you’re able to identify a fast progressor and increase your efforts to try to prevent further vision loss.
For example, suppose a patient is losing 1 dB of vision each year—a significant amount of loss. If you only do one visual field test per year, it will take you four years, on average, to realize that the patient is progressing at that rate. If you do two tests per year, you can detect that rate of loss within three years. If you do three tests per year—which is hard to do in a clinic population—you only decrease the time to detection to 2.6 years (on average). Dr. Medeiros’s suggestion for dealing with these practical constraints is to do several visual field tests when first working with the patient to establish a baseline, and then do two tests per year. Clearly, this is not ideal, but practically speaking, it’s the best we can do for most patients.
This is a key reason having a reliable visual field test that can be done outside the office—one that the patient won’t hate to take—could be a boon for patient care. Our work so far has shown that this test is easy for patients to take, even multiple times in a row. Right now we’re doing a longitudinal study where patients are taking the test 10 times per quarter, a schedule we call VVP-10. These glaucoma patients, all with existing visual field defects, were either given the device to take home or were mailed the device. They were trained to use it virtually. The test uses the same pattern of stimulus points as the Humphrey 24-2, allowing us to compare the data more easily. We test each location in the visual field four times.
This test-taking schedule gives us the data from 40 tests per year, which cuts the time required to detect a fast progressor by as much as 66 percent, compared to doing two Humphrey tests every year. For example, a fast progressor, losing 1 dB per year, would be detected in three years using two Humphrey tests per year. Using our VVP-10 test and schedule, you’d detect that rate of loss in one year. (See graph, above.) The fact that patients don’t find the test unpleasant or challenging—and they can do it at home—is crucial. (I can’t imagine asking a patient to do the Humphrey test 40 times a year.)
Our data so far indicate several specific things:
- Test-retest variability is very good.
- Pointwise correlation between VVP-10 and Humphrey was quite strong. (We’ve submitted an abstract to ARVO discussing this data.)
- Global mean sensitivity on the Humphrey test correlated well with the fraction correct seen using VVP-10. Of course, we’re not comparing the exact same thing, because the current version of VVP doesn’t include a threshold test like the one included in the Humphrey test.
Regarding that last point, the Humphrey test uses a white background and a white stimulus. During the test, the stimulus is dimmed until the patient doesn’t respond to it half the time. That’s the patient’s threshold sensitivity. Our current test uses a black stimulus on a white background and doesn’t change the intensity of the stimulus, i.e., the contrast. (We’re looking at incorporating a threshold test into upcoming versions of the VVP.)
VR for Other Visual Tests?
There’s no question it would be convenient to have other visual tests that could also be taken using the virtual reality goggles, and I’m sure this will happen in the future as technology advances. For now, though, measuring factors such as visual acuity is problematic, in part because the screen resolution doesn’t currently match the eye’s foveal resolution. The current off-the-shelf virtual reality technology can be used to measure visual acuity in eyes with poor vision—e.g., 20/70 or worse—but they can’t do much better than that. Certain patients, such as those with amblyopia, can be measured to look for improvement.
Of course, current virtual reality goggles can be used for specific types of tests such as driving simulation tests. I can imagine a virtual reality test that simulates a child chasing a ball into the street in front of the car, or a pedestrian crossing a crosswalk against the light. They goggles might also be useable for binocular tests of peripheral vision such as the Esterman test.
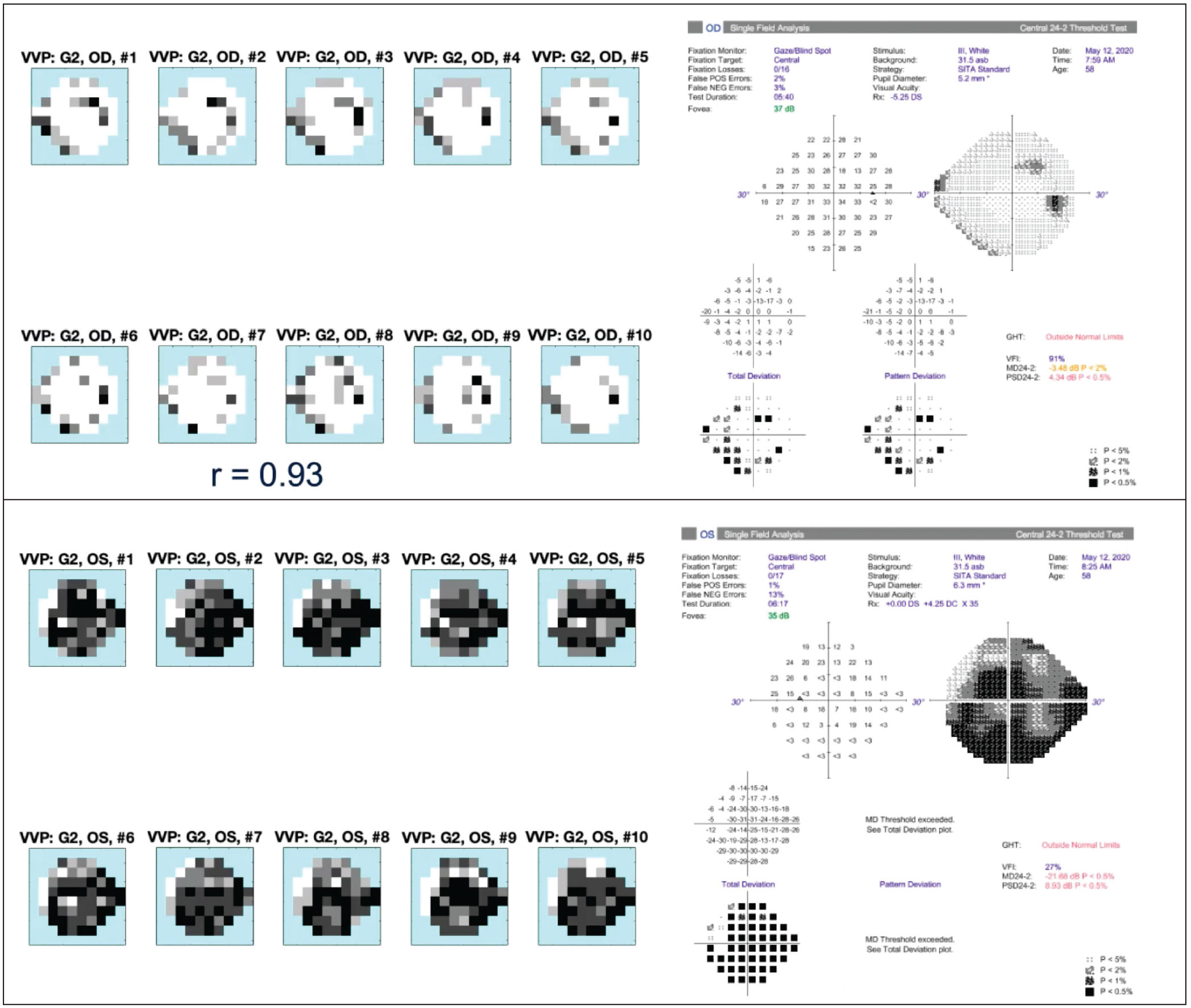 |
| Two examples of VVP-10 fields compared to Humphrey 24-2 fields for the same eyes. The point-by-point matches are close and the VVP-10 results are highly repeatable. Click image to enlarge. |
In the meantime, other information crucial to monitoring glaucoma, such as optical coherence tomography data, could be obtainable at home soon, thanks to portable OCTs that are in development. Having OCT and visual field data without the patient having to come to the office could be a game-changer in our ability to save our patients’ vision.
Stepping into the Future
The VVP system isn’t commercially available, although the team is preparing a research version that will be available for preorder soon. They expect to start delivering it on a first-come, first-served basis before summer. They’re hoping to enlist early adopters who are interested in contributing to the research effort.
What may lie ahead for this technology? The potential benefits of patients being able to conduct visual field tests at home are clear, but I can also see the benefit of using this in offices, where patients could take the test while waiting to see the ophthalmologist. The training module tutorial would be part of the testing experience; it could also serve to identify patients who are unable to follow the basic instructions.
One benefit of this possibility would be that a technician could administer many more tests than what’s currently feasible. I’ve seen some clinics run two to three visual field tests concurrently, but even doing this is challenging; here at UCSF, one technician can help two patients at most take the test at the same time. With VVP, I can imagine one technician administering 10 tests at the same time. Everyone in the waiting room could have virtual reality visual field goggles on, getting their visual field testing done.
This technology could also be used for real-world screening. The Humphrey test would be challenging to use for this purpose, but a simpler, more portable test like this could work. Of course, there are some visual field tests currently available that are lighter and more mobile than the Humphrey test, and those are sometimes used at eye-screening clinics. But you can’t get much smaller or more convenient than a pair of virtual-reality goggles.
We’re eager to have more doctors involved in collecting data, to help move the development of this technology forward. If you’re interested in participating, you can sign up for a research kit at https://seevividly.com/vvp. Needless to say, I’m excited about the possibilities opened up by a new option like this. It’s a promising new step into a future in which we can do an even better job of preserving our patients’ vision.
Dr. Ou is an associate professor of ophthalmology, academic director of the glaucoma division and vice chair for postgraduate education in the Department of Ophthalmology at the UCSF School of Medicine in San Francisco. She reports no financial ties to any product discussed.



