Although cataract surgery almost always goes smoothly, the fact that it’s performed on millions of individuals every year guarantees that any cataract surgeon will encounter plenty of challenging cases over time. Here, cataract surgeons share their advice for dealing with challenging cases that they’ve encountered.
Patients with Corneal Pathology
 |
|
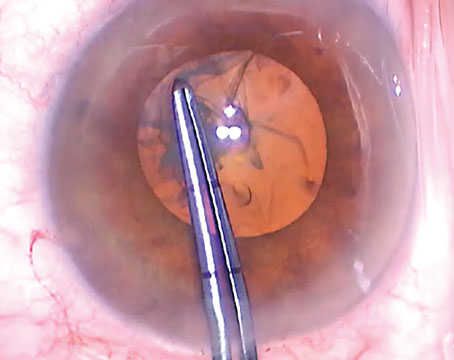
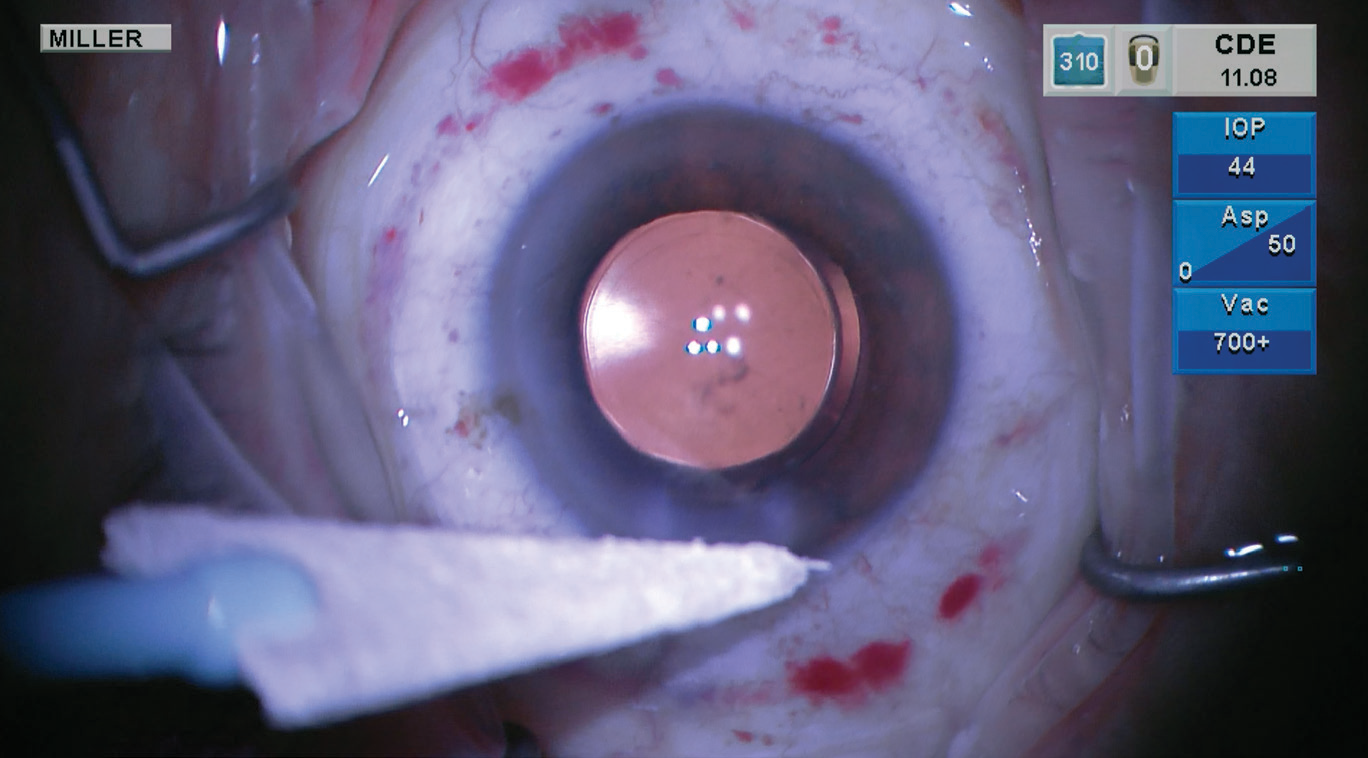
Cataract surgery in a young man with previously uncontrolled uveitis, resulting in dense cataract, posterior synechiae and iris-cornea touch. A combination of employing iris hooks, creating space with viscoelastic between the iris and cornea, releasing synechiae and staining the anterior capsule with trypan blue allowed for careful capsulorhexis and in-the-bag placement of the lens. (Image courtesy of Sruthi Arepalli, MD) |
Zaina Al-Mohtaseb, MD, an associate professor of ophthalmology and associate residency program director at Baylor College of Medicine, offers these pearls:
• Always look for corneal pathology preoperatively. “It’s important to diagnose co-existing corneal pathology in cataract patients because corneal diseases can affect IOL selection,” she notes. “In addition, cataract surgery can contribute to the progression of co-existing corneal disease, limiting visual outcomes postoperatively. Diagnosing epithelial basement membrane disease in particular is vital, as it can lead to decreased vision, irregular astigmatism and inaccurate IOL power calculations. If your patient has this problem, perform superficial keratectomy and then await stabilization of the topography. That stabilization takes an average of at least three months after the keratectomy procedure.”
• If the view through the cornea isn’t ideal …. For cataracts with a difficult view through the cornea (secondary to scarring or neovascularization, for example), Dr. Al-Mohtaseb offers these tips to help ensure a safe cataract extraction:
— Optimize the ocular surface prior to the cataract surgery.
— Use the topography and IOL power calculations or the average K from the other eye.
— Be sure to achieve good pupil dilation.
— Use trypan blue to enhance visualization.
— Adjust the illumination to low or medium lighting, because too much co-axial lighting can cause backscatter.
— Consider using a light pipe (from a vitrectomy machine or photon laser light) to aid visualization during the case.
— If the cornea is scarred, start the capsulorhexis in a transparent area.
• Be cautious if the patient has Fuchs endothelial dystrophy. Sumit (Sam) Garg MD, vice chair of clinical ophthalmology, medical director and professor of cataract, corneal & refractive surgery at the Gavin Herbert Eye Institute at the University of California, Irvine, offers three pearls for managing these patients:
— Consider using a femtosecond laser to assist in removing the cataract. “The laser allows me to pre-soften the nucleus, which then allows for the use of less phacoemulsification energy,” he explains.
— Use ample dispersive OVD in these cases. “This will protect the fragile endothelium,” he says.
— Consider implanting a three-piece IOL. “I generally favor three-piece IOLs in these patients if I feel that a DMEK may be necessary in the not-too-distant future,” Dr. Garg explains.
 |
|
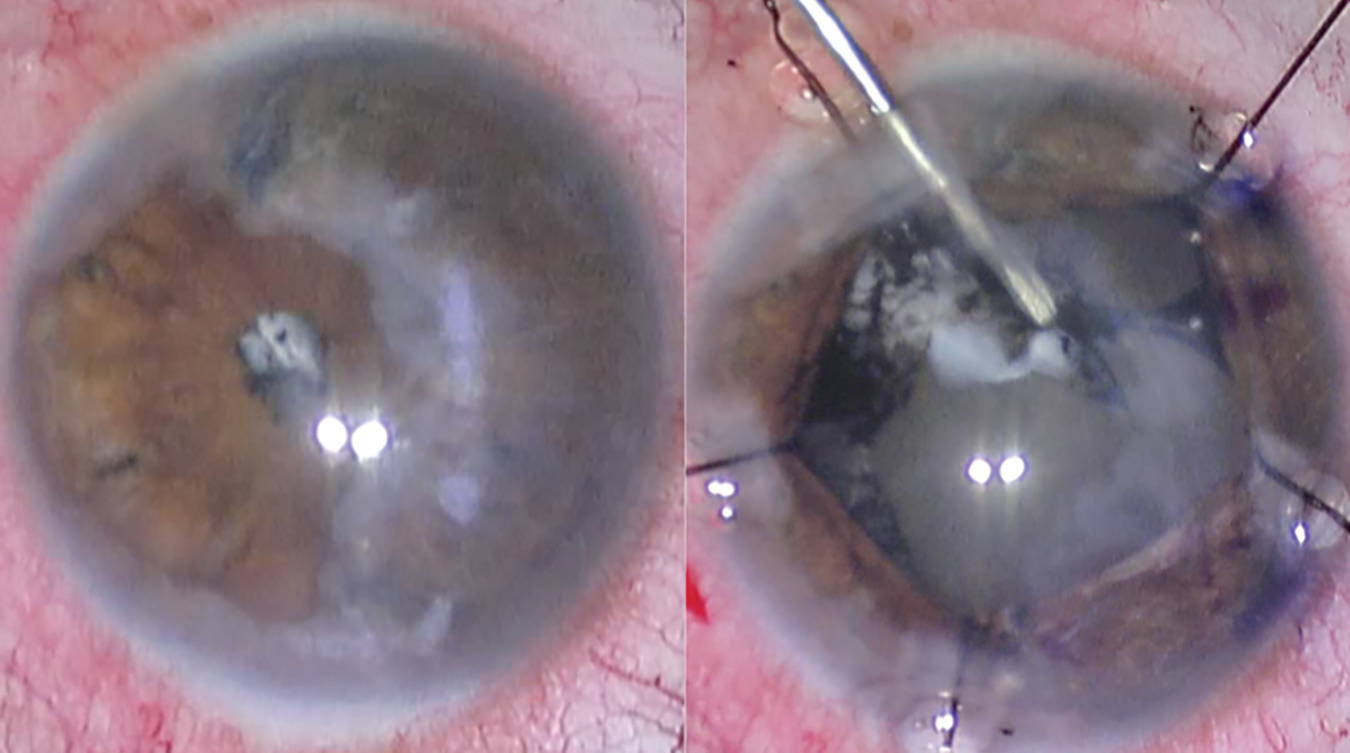
It’s always important to manipulate an IOL by grabbing it at the edge or at the optic-haptic junction, surgeons say. Above: A surgeon rotates an extended-depth-of-focus, single-piece acrylic posterior chamber IOL within the capsular bag using a Kuglen hook, engaging the lens at the optic-haptic junction. (Image courtesy of Kevin Miller, MD) |
• Don’t place your wound too far posteriorly. “Some corneal peripheral abnormalities such as arcus and pannus can make it challenging to know where to make the corneal wound,” notes Robert Weinstock, MD, director of cataract and refractive surgery at the Eye Institute of West Florida in Largo, Florida, and an assistant clinical professor in the Department of Ophthalmology at the University of South Florida.
“The best way to avoid placing the wounds too posteriorly is to be very conscientious in wound creation,” he says. “Err on the side of caution and place the wound slightly anterior to the limbus. A good rule of thumb is to place the corneal wound just at the beginning of clear corneal tissue.”
Dr. Weinstock adds that surgeons in training often make their wounds too posteriorly, causing subconjunctival chemosis. “In these cases the conjunctiva is cut at the posterior edge of the wound,” he explains. “During cataract surgery, fluid finds its way under the conjunctiva and balloons it up, 360 degrees. This can make for a very challenging view of the eye. It also makes it difficult to close the eye postoperatively.”
If the Patient has a Cough ...
Tape the patient’s head to the gurney. “I actually do this for every case,” says Kevin M. Miller, MD, chief of the Cataract and Refractive Surgery Division and a professor of clinical ophthalmology at the David Geffen School of Medicine at UCLA. “You never know when someone will cough, sneeze, begin snoring, or suddenly awake from sleep and shake their head.”
With Highly Myopic Eyes
Pressurize the eye slowly when turning irrigation flow on. “Although this is good advice for any cataract surgery, it’s especially important for large, myopic eyes,” says Dr. Miller. “Slow pressurization can be achieved using the machine settings for ‘IOP Ramp’ if you’re using the Centurion phaco unit, or by slowly raising the bottle on gravity-fed phaco machines.”
If the Patient has Uveitis
“Uveitis-related cataracts are typically not straightforward, so expect surprises,” says Sruthi R. Arepalli, MD, a uveitis and vitreoretinal surgeon at Tennessee Retina in Nashville. She offers these suggestions:
• Get inflammation under control before the surgery. “Peri-operative control of inflammation is necessary for better outcomes,” she notes. “Generally, this means keeping the eye quiet with the help of uveitis colleagues and rheumatologists for at least three months prior to surgery.
“Of course, there are rare exceptions to this,” she continues. “While I prefer to wait three months with the disease quiescent before doing cataract surgery, there are some situations in which waiting that long isn’t possible. Sometimes, the patient depends on this eye for functional vision. Sometimes the patient is young and at risk of developing amblyopia in that eye if we wait three months for surgery. In those cases, I’ll add additional oral or peri-ocular steroids to quiet the eye if I plan on entering the eye before the three-month period is up.”
• Avoid topical anesthesia in these patients. “In order to limit unnecessary variables, I stay away from topical anesthesia in cataract patients with uveitis,” Dr. Arepalli says. “I often have patients receive either a retrobulbar or peribulbar block. In certain cases, such as pediatric patients or cases that may be more complicated where I anticipate a longer surgical time, I’ll plan for general anesthesia.”
• Have extra surgical tools at the ready. “In addition to the typical surgical set up for a phacoemulsification, I request trypan blue and iris hooks, at a minimum,” notes Dr. Arepalli. “It’s always good to have capsular tension rings as well, and an anterior vitrectomy set up if necessary.”
• Placing a three-piece lens is preferable. “Placing a three-piece lens in a uveitic patient gives me more flexibility down the road if I need to place it in the sulcus during a later surgery, or need to rescue the lens if it falls,” Dr. Arepalli explains.
• You may need to leave some young uveitic patients aphakic. “I’ll leave a young patient aphakic if I anticipate that their postoperative period will have a lot of inflammation, or if I don’t think I can safely place a lens during the initial surgery,” Dr. Arepalli says. “I can always come back and place a lens after the eye settles down and I see how they’re healing.”
• If the uveitis is severe, increase the steroids. “If the disease is severe I’ll give additional topical or oral steroids before and after the cataract surgery,” says Dr. Arepalli. “I also taper topical steroids very slowly after the surgery and monitor the patient more frequently than other patients, in case they need further modifications to their immunosuppression.”
Iris Instability
 |
|
Experts say that performing bimanual surgery can be a big help when dealing with a floppy iris, and can also allow very gentle insertion of a capsular tension ring if that’s necessary. Above: Robert Weinstock, MD, observes fellow Kirk Castellano, MD, doing bimanual surgery using the Beyeonics One virtual reality headset. (Image courtesy of Robert Weinstock, MD) |
Dr. Weinstock offers these tips for managing an eye with an unstable iris:
• Use bimanual technique. “Floppy iris syndrome and iris prolapse are among the most challenging things to deal with during cataract surgery,” Dr. Weinstock notes. “Using bimanual phaco and bimanual irrigation and aspiration is a great way to deal with this situation. With these techniques, the wounds are smaller and the irrigation can be kept anteriorly, pushing the iris down and away from the wounds, while the cataract is removed deeper in the eye.”
• Avoid iris prolapse by decompressing the eye, sealing the wounds and then gently reinflating. “Often, at the end of the case when the eye is inflated and pressurized, an unstable iris will prolapse out of the wound,” Dr. Weinstock explains. “In these situations, it’s best to decompress the eye; completely soften it and then seal the wounds with stromal hydration. Then, gently reinflate the eye by injecting BSS into the anterior chamber, pushing the iris back.
“If this doesn’t work,” he adds, “put sutures across the wounds while the eye is soft and then gently inflate, pushing the iris down and back. Gentle fluid dynamics work in the surgeon’s favor, helping to complete these cases successfully and avoid complications.”
Sticky Cortex
• When necessary, viscodissect the cortex off the posterior capsule. “I often see surgeons struggle with cortical cleanup, especially in the sub-incisional area,” says Dr. Weinstock. “Many times this leads to inadvertent tears of the capsule or zonular dehiscence because of pressure put on the posterior capsule.
“A simple way of dealing with the situation is to come out of the eye and use a viscoelastic such as Amvisc or another cohesive type to gently viscodissect the cortex off the posterior capsule and push it anteriorly up into the sulcus. Then an artificial lens can be inserted, stabilizing the capsule. The residual cortex can be removed with bimanual irrigation and aspiration once the IOL is in place.”
Pseudoexfoliation/Zonular Laxity
Francis Mah, MD, who specializes in cornea, external disease and refractive surgery at Scripps Clinic in La Jolla, California, offers pearls for operating on patients with pseudoexfoliation, or in whom you have any suspicion that zonular laxity may be present:
• Don’t overfill the anterior chamber with viscoelastic. “Doing so could risk causing more zonular damage,” Dr. Mah points out.
• Create the largest capsulorhexis you can comfortably create, despite what might be a smaller pupil. “This will make it easier to get the cataract out, with less chance for anterior capsular phimosis and a dislocated posterior chamber IOL days, weeks or years later,” Dr. Mah explains.
 |
|
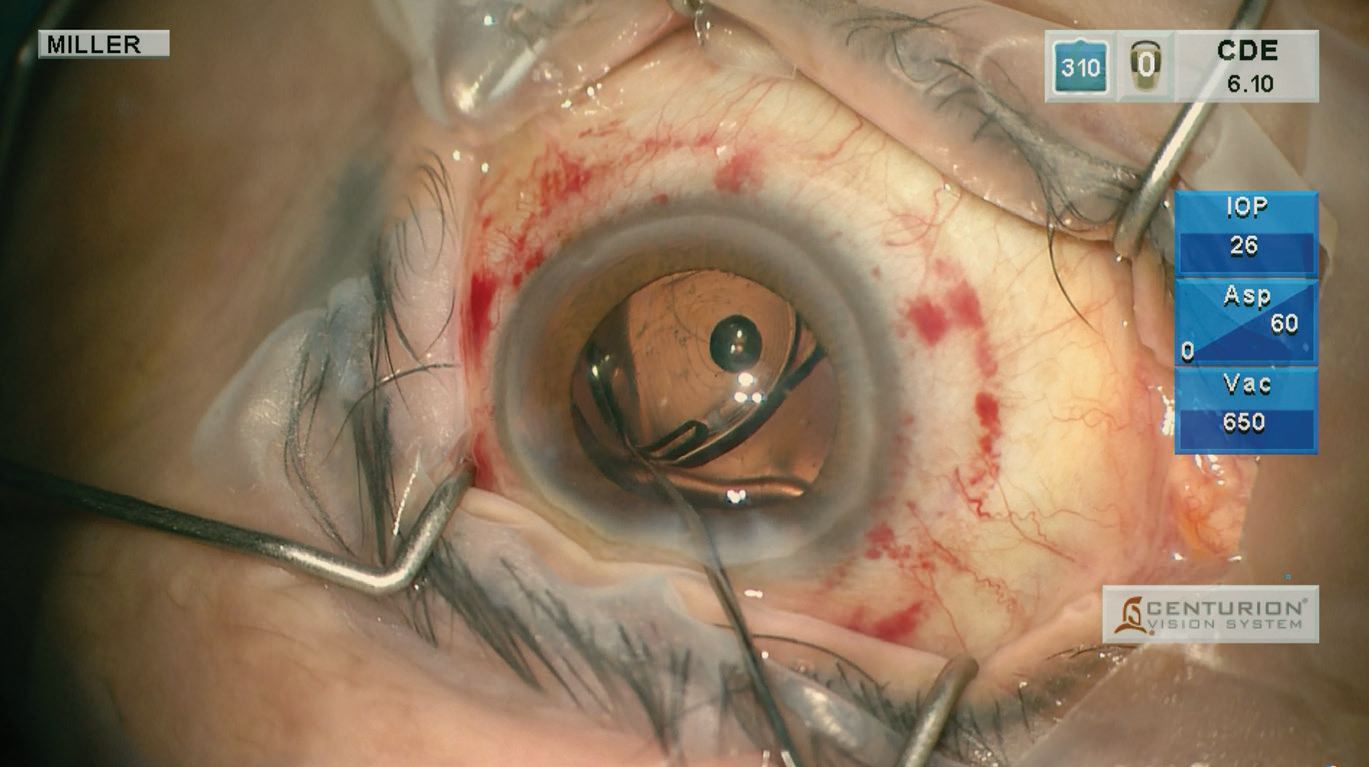
When using a cystotome to create your capsulorhexis, don’t start with a deep puncture; a deep puncture may dig up cortex that will later obscure your view. Above: An anterior capsule puncture is performed using a 30-gauge needle in an anterior capsule stained with trypan blue. (Image courtesy of Kevin Miller, MD) |
Should the surgeon try to enlarge the pupil in this situation?
“My general mantra in the OR is ‘less is more,’ so if a pupil is 5 mm or larger, I just go with it, especially in cases of pseudoexfoliation and zonular laxity,” says Dr. Mah. “This is a little different than intraoperative floppy iris syndrome or Flomax cases; in those cases the pupil will most likely come down during the surgery, so use of a ring or hooks to enlarge and/or maintain pupil size is critical. In 5- or 6-mm pupils, I go right up to the pupil margin when creating the capsulorhexis. You’ll find the pupil will actually be a tiny bit more dilated during the surgery and at the conclusion of the case, because removing the cataract allows more space for the pupil.
“If the pupil is between 3 and 5 mm,” he continues, “I usually just stretch it with Kuglen-style hooks placed 180 degrees apart to create microtears along the pupil sphincter. Usually, you’ll gain 1 to 2 mm with this maneuver. If the pupil is smaller than 3 mm, I like Greishaber-style pupil hooks. If you think you need the hooks, I’d advise making all the corneal paracentesis incisions before making the main incision, because it’s easiest to make these incisions before you’ve done any other manipulations to the eye.
“There are various rings for enlarging the pupil, such as the Malyugin and iRing,” he adds. “You might consider using a 6.25-mm Malyugin ring around a 4-mm pupil. I personally don’t use these in pseudoexfoliation cases, since the pupil will stay dilated during these cases; I reserve them for IFIS cases. However, you should use whatever technology you need to feel comfortable and safely remove the cataract.”
• Be sure to do an excellent hydrodissection. “You may want to devote more time to this than usual, to ensure that the cataract moves easily, so undue stress or tension on the zonules doesn’t occur,” Dr. Mah explains.
• Don’t wiggle the hydrodissection cannula when you advance it out under the capsulorhexis. “The fluid you inject into the eye will follow the path of least resistance when it leaves the tip of the cannula,” explains Dr. Miller. “If you push the cortex aside while advancing the cannula, the fluid will make a 180-degree turn when it exits the tip and come right back along the side of the cannula.”
• Use whatever lens disassembly technique you’re most comfortable with. “Use the technique you typically use,” Dr. Mah advises. “Don’t use something less familiar just because you’re dealing with zonular weakness. It’s good to use a technique that will allow you to avoid rotating the lens too much or pressing on it. Stop-and-chop, vertical chop, and ‘V’ techniques are nice if they’re in your armamentarium, because they require less rotation of the lens. However, this isn’t the time to try a new technique.”
• Don’t use the phaco needle to rotate a lens. “To avoid stressing the zonules any more than necessary, you want to maximize torque and minimize push when rotating a nucleus,” notes Dr. Miller. “In other words, use a second instrument, perhaps a cyclodialysis spatula, lens manipulator or chopper, instead of the phaco needle, to engage the peripheral lens and rotate it.”
• If implanting a CTR, considering using a bimanual approach. Dr. Garg says that in recent years he’s changed the way that he implants a capsular tension ring when the patient has weak zonules. “I used to just inject the CTR into the capsular bag as gently as possible,” he notes. “Now, I’ve transitioned to a bimanual technique in which I use a Sinskey hook to stabilize the leading eyelet of the CTR. This allows me to place the CTR into the capsular bag even more gently.”
• During cortical cleanup be careful to not accidentally grab the capsule. “If you grab the capsule,” Dr. Mah explains, “zonules will easily break. The capsule might become looser and the capsule will become floppier.”
 |
|
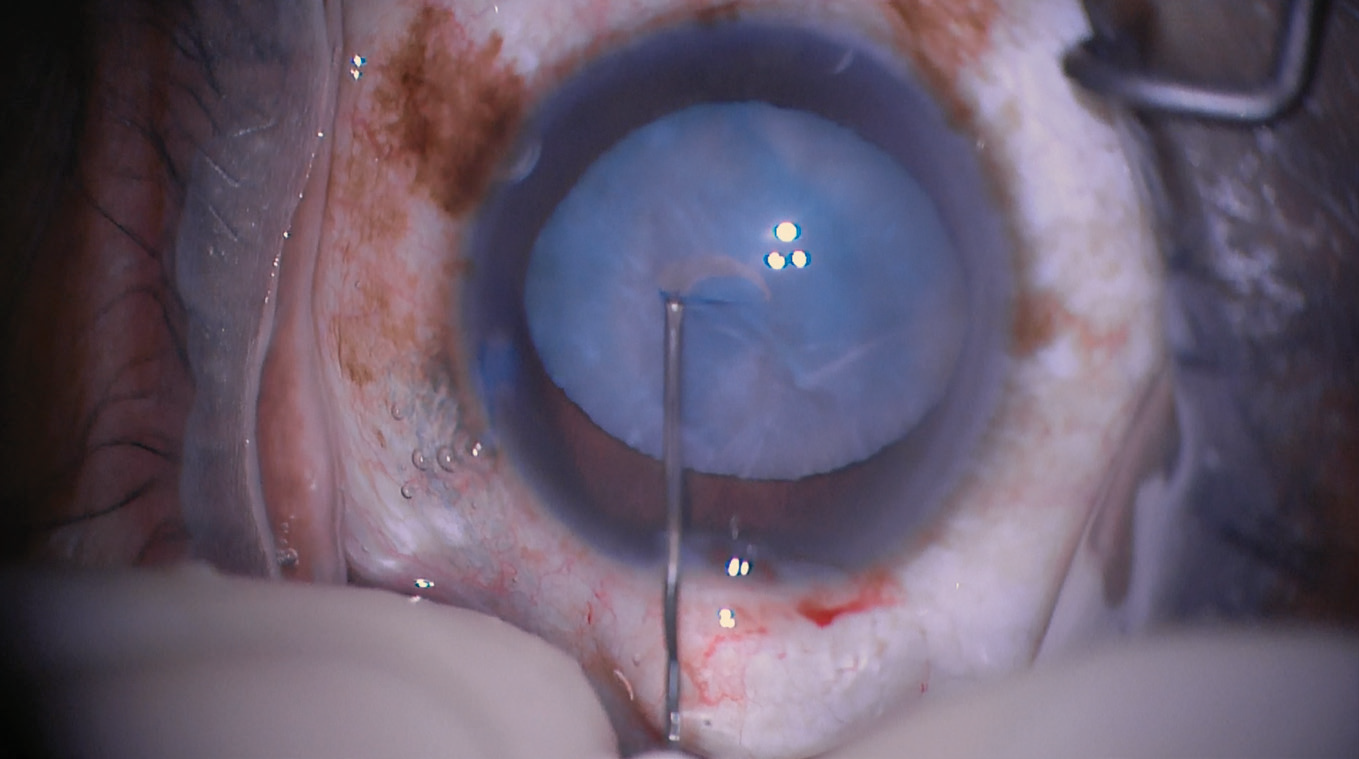
To reduce the risk of endophthalmitis following cataract surgery, dry the the exterior ocular surface to reduce the load of bacteria on the eye before hydrating the incisions. (Image courtesy of Kevin Miller, MD) |
• Orient the lens haptic based on the location of zonular laxity. “If there’s an area of specific zonular laxity, as opposed to general zonular laxity, try to put the haptic of the IOL in that area,” Dr. Mah says. “This will ensure that the bag is fully expanded in that area.”
• Use specifically designed anterior capsule polishers to thoroughly remove the lens epithelial cells from the entire anterior capsule. “The anterior capsule will be much cleaner years later, and you’ll never have a lens decenter on you,” adds Dr. Miller. “This will establish your reputation as a Picasso instead of a house painter! It’s particularly important to polish the anterior capsule in eyes with weak zonules because aggressive contraction of the capsulorhexis postoperatively could further stress the zonules. It’s also a good strategy when operating on very young eyes, because lens epithelial cells in young eyes proliferate more aggressively.”
Pearls for All Occasions
Surgeons offer these tips for any cataract surgery case:
• Learn how to control eye position by using the corneal incisions as pivot points. “The experienced cataract surgeon is able to keep an eye perfectly centered under the microscope while performing complex manipulations at the tips of the instruments,” says Dr. Miller. “Each instrument passes through a corneal incision, and each corneal incision can be manipulated in the axis of the incision by the instrument that passes through it. So, if the corneal incisions are 90 degrees apart, a surgeon can completely control the rotational position of the eye in three axes—back and forth, up and down, and rotationally.”
• If employing a cystotome to create a capsulorhexis, use an appropriate technique. “If you’re using a cystotome to create your capsulorhexis, don’t start with a deep puncture,” says Dr. Miller. “Instead, use the tool to barely puncture the anterior capsule. That way you won’t dig up a lot of cortex that will subsequently obscure your view. Also, once the initial capsule puncture and cut are made, pull the cystitome toward you to begin the circular part of the tear. A bent needle works much better as a pulling instrument than it does as a pushing instrument.”
• To reduce the risk of “punching through” the epinucleus and cortex at the end of a trough when sculpting, set the “Vacuum Rise” setting on an Alcon Centurion or the “Dynamic Rise” setting on an Alcon Infiniti to -2. “When the machine senses it’s nearing vacuum limit, it will quickly dial the AFR back 50 percent to release the ‘grab,’ ” Dr. Miller explains.
• Use a “last fragment setting” when removing the final piece of nucleus. “What that means is, dial the vacuum limit down when you’re removing the last fragment,” says Dr. Miller. “That way you won’t get an occlusion break surge and pop a hole on the posterior capsule.”
• Manipulate the IOL by grabbing it at the edge or at the optic-haptic junction. “Don’t touch the surface of an optic with the I/A probe or other metallic instrument,” advises Dr. Miller. “Those instruments will scratch the lens.”
• Be sure to remove the viscoelastic behind the optic. “A lot of OVD can get trapped back there,” Dr. Miller points out. “The best way to do this is to go behind the lens with an irrigation-aspiration probe.”
• Always flush out the angle recesses with BSS. “Do this even after removing your viscoelastic,” Dr. Garg advises, “especially when performing femtosecond-laser-assisted cataract surgery. You’ll be surprised how much residual OVD and/or fine nuclear chips can be hiding in the angle. Flushing out the angle with BSS can help prevent retained lens fragments and postop IOP spikes.”
• Dry the corneal incisions with a sponge before you hydrate. “Despite your use of povidone iodine, the fluid on the ocular surface at the end of surgery is a cesspool of bacteria and other microbes,” Dr. Miller explains. “Any microbes that enter the eye during surgery will be irrigated out, but whatever gets pushed into the eye at the end of surgery when you hydrate the incision will stay in. So, be sure to soak up the contaminated fluid from the surface of the eye before you hydrate the incisions.” τ
Dr. Garg is a consultant to Johnson and Johnson Vision. Dr. Miller is a consultant to Johnson and Johnson Surgical Vision, Long Bridge Medical and Oculus USA. Dr. Weinstock is a consultant to Alcon, Johnson and Johnson Vision, Bausch + Lomb and Zeiss. Dr. Mah is a consultant to Alcon, Johnson and Johnson Vision and Bausch + Lomb. Dr. Arepalli and Dr. Al-Mohtaseb have no relevant financial ties to report.