Global risk assessment that incorporates all available data should play an important role in making treatment decisions for patients with ocular hypertension. However, a global risk assessment tool is a goal rather than a reality today. Estimates used to assess patients will evolve and change as new population-based epidemiologic information becomes available and as available information is reassessed.
In a recent American Journal of Ophthalmology article, my coauthors and I described our initial efforts to develop a model to estimate the global risk of disease progression in ocular hypertensive patients and to calculate the "number needed to treat" to prevent progression to blindness.1
OHTS Results
The five-year results of the Ocular Hypertension Treatment Study were published in 2002.2 These results have caused some ophthalmologists to reassess the ways in which they evaluate and manage patients with ocular hypertension. The OHTS found that the cumulative probability of developing glaucoma after five years with untreated ocular hypertension was 9.5 percent.2,3 Not all patients who develop glaucoma, however, will lose functional vision during their lifetimes.
OHTS identified several risk factors that increased the chances of progression to glaucoma. While OHTS provided valuable information to glaucoma specialists, precise calculations of risk for disease progression to the loss of functional vision in individual patients are not yet possible.
Ophthalmologists clearly need a way to assess the risk data that predict the progression from ocular hypertension to loss of functional vision. To address this need, we looked at the cardiovascular disease risk model process and then surveyed the ophthalmic literature to find population-based studies of patients with ocular hypertension and glaucoma. This should allow us to begin to estimate the risk of progression from ocular hypertension to glaucoma and from glaucoma to unilateral blindness for both treated and untreated patients.
Figures recreated from Am J Ophthalmol 138;3:458-467with permission from Elsevier.
Cardiovascular Disease Model
A successful global risk assessment model has been used for many years to assess patients with cardiovascular disease.4 By knowing the status of a group of risk factors, it is possible to estimate the 10-year risk of having a cardiac event and to compare that risk to the general population. High-risk individuals are treated to reduce risk.
In comparison to cardiovascular disease assessment, glaucoma risk assessment is early in its development and is imprecise; only a limited number of factors have been identified. However, analyzing the available data should allow us to begin to prepare estimates of an individual's global risk of progressing from ocular hypertension to blindness. While these estimates are still a work in progress, they may help ophthalmologists manage patients with ocular hypertension.
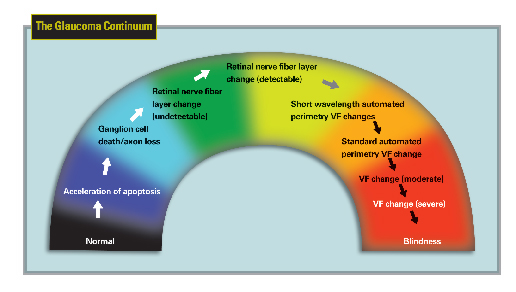
The Glaucoma Continuum
Glaucoma is a neurodegenerative disease of the optic nerve that can progress from undetectable disease to asymptomatic disease to functional impairment.5,6 Patients present to ophthalmologists at various stages of a continuum that is characterized by accelerated retinal ganglion cell death, subsequent axonal loss and optic nerve damage, and eventual visual field loss.1
At the beginning of the continuum, the initial changes in the retina and optic nerve are often asymptomatic and undetectable with currently available diagnostic tests. Additionally, physicians cannot agree on criteria for the diagnosis of the early damage that precedes standard achromatic visual field loss. Ophthalmologists therefore often wait for obvious signs of disease, which can result in a substantial amount of irreversible damage and progression.
Patients with ocular hypertension or glaucoma can progress to functional vision loss, and blindness may occur. Because many patients present in the early stages of the disease, the goal of treatment is to stop, delay, or limit progression to significant visual impairment. Identifying the individuals at greatest risk of developing functional vision loss may allow us to improve outcomes.
Related Clinical Studies
OHTS prospectively evaluated progression of patients with ocular hypertension through the development of earliest detectable glaucomatous change in the optic disk, visual field, or both.
Additionally, two observational studies of patients with established glaucoma have also provided data on disease progression to substantial visual field loss. First, researchers in Minnesota's Olmsted County retrospectively assessed patients and divided them into three groups: those with open-angle glaucoma, those with ocular hypertension, or those with unsupported glaucoma, which meant that patients were treated for glaucoma but lacked documentation of the diagnosis. The researchers determined each group's risk of developing either unilateral or bilateral blindness.7
In this study, residents of Olmsted Co. with diagnoses of ocular hypertension or glaucoma were followed for a mean of 15 ±8 years. The patients who were treated for ocular hypertension had a 4-percent 20-year cumulative probability of bilateral blindness and a 14-percent 20-year cumulative probability of unilateral blindness.
The second study was conducted in St. Lucia, West Indies.8 After an initial population survey, the investigators later returned and assessed the disease progression of untreated patients with diagnosed or "suspected" glaucoma to end-stage disease. Treatment had been recommended or initiated in these patients but was not maintained due to inadequacies in the infrastructure of subsidized glaucoma care.
Other studies, such as the Early Manifest Glaucoma Trial (EMGT),9 the Advanced Glaucoma Intervention Study (AGIS),10 and the Collaborative Initial Glaucoma Treatment Study (CIGTS),11 have evaluated the risk of glaucoma progression with or without medical intervention, but have not reported specific end points.
The Glaucoma Continuum
To estimate the risk of progression from ocular hypertension to blindness using the available study outcomes data, we made some assumptions:
• Unilateral vision loss is a relevant and conservative endpoint.
• Time progression periods can be added.
• Risk of progression to functional impairment is linear.
• A 15-year period is relevant for disease.
• OHTS results can be applied to the entire ocular hypertension population.
• Olmsted Co. results (treated patients) can conservatively be used to estimate progression in untreated patients.1
We recognize that these assumptions may or may not be proven as new evidence evolves.
Estimating Risk of Progression
Based upon these assumptions, it is possible to tentatively estimate the risk of progression to blindness for untreated and treated patients. To obtain an estimate of the risk of progression from glaucoma to unilateral blindness in untreated patients, we used data from the 10-year St. Lucia study. In this study, 16 percent of patients progressed to end-stage disease in at least one eye, based on an AGIS score of 18 or higher.
Therefore, if 9.5 percent of untreated patients will progress from ocular hypertension to glaucoma in five years as found in OHTS, and if 16 percent of those patients will develop unilateral blindness in five years as found in the St. Lucia study, then the risk of progression from ocular hypertension to functional impairment would be 1.5 percent over 15 years.
In comparison, when using OHTS data and the Olmsted data, we calculated the risk to be 2.6 percent over 15 years.
The risk of disease progression also was estimated in the St. Lucia study using CIGTS criteria for assessing visual field changes, which in general have lower levels of impairment for a given score than does the AGIS system. While CIGTS criteria do not define end-stage glaucoma, 35 percent of patients deteriorated to a CIGTS score of 18 or higher in at least one eye over a 10-year period. Using this value, the risk of progressing from ocular hypertension to a CIGTS score of 18 or more is 3.3 percent.
Unfortunately, no single study has assessed the impact of treatment on the risk of progressing from ocular hypertension to unilateral blindness. The only current way to estimate treatment impact is to combine the OHTS reduction in conversion rates from ocular hypertension to glaucoma with results from available glaucoma studies on reduction of risk of progression of glaucoma.
In the OHTS, the reduction in risk of converting from ocular hypertension to glaucoma with treatment was 54 percent over five years, while the EMGT found that treated patients' risk of progressing was 50 percent of that seen in untreated patients.
 |
Therefore, the risk of progressing from ocular hypertension to unilateral blindness in treated patients can be estimated at 23 percent of that for untreated patients. Data from the OHTS and the EMGT yield an estimated reduction of 77 percent in the risk of developing glaucoma and its progression with treatment. When applying this factor to our previously calculated risks of progression for untreated patients, we estimate that the risk of progression from ocular hypertension to blindness in treated patients over 15 years ranges from 0.3 to 0.6 percent, depending on the data set used.
When applied to the reported Olmsted data for progression from ocular hypertension to unilateral blindness, the estimated risk of progression for treated patients is 2.4 percent. Ophthalmologists should note, however, that this approach is conservative in that we may have overestimated the benefits of treatment by underestimating the number of patients converting from ocular hypertension during the 15-year period.
Overall, these calculations suggest that treatment may reduce the risk of progressing from untreated ocular hypertension to blindness between 1.2 percent and 8.1 percent over 15 years.
To determine how these calculations can affect our decision making in managing the ocular hypertension patient, we needed to determine the number of patients who need to be treated to prevent unilateral blindness in one patient. The number needed to treat is calculated using the following formula: 1/(difference in absolute risk between no treatment and treatment groups).1
Based upon our estimates, between 12 and 83 patients with ocular hypertension will require treatment to prevent one patient from progressing to unilateral blindness over a 15-year period.
Individual Risk
While this information can help us begin to make population predictions, it alone cannot determine whether or not to treat an individual patient. The number needed to treat approach is based on average risk of progression without consideration of individual risk. Assessing patients based on all of the major risk factors will allow for the identification of patients who are most likely to benefit from treatment and would quantify the combined effect of the risk factors that practitioners should consider in making treatment decisions. Additionally, ophthalmologists should consider the risks and benefits of various modalities when making such treatment decisions.
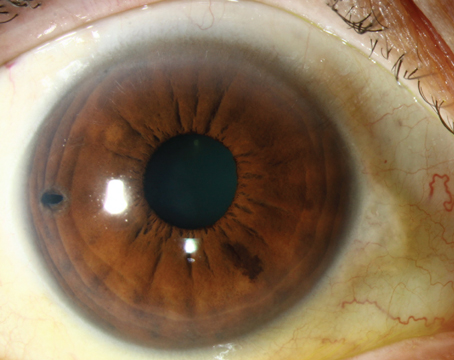
An individual patient's global risk of progression is affected by factors that have been found to be associated with higher risks of progression. For example, patients with higher mean intraocular pressure levels and increased cup-to-disk ratios are at highest risk of progression. In addition, small differences in pattern standard deviation at baseline, even among patients with normal and reliable results on Humphrey 30-2 Field Analyzer (Carl Zeiss Meditec, Inc, Dublin, Calif.) visual field tests, correlate with greater risk of disease progression in the OHTS.
Therefore, this might be an indicator of early glaucomatous damage. Assessing these differences in pattern standard deviation is not likely to be useful, however, because such small differences can be seen only by taking an average from multiple visual fields, so repeated testing is required. Thinner central corneal thickness measurement is also a risk factor for progression.
When deciding whom to treat, ophthalmologists should take patients' age into account. While age is positively correlated with greater risk of progression, if all other things are equal, older patients' shorter life expectancy may discourage aggressive treatment.
Consequently, a global assessment of risk should include age, IOP level, cup-to-disk ratio, and central corneal thickness. Combining all of these data can provide ophthalmologists with a useful indicator of individual risk.
For example, in the OHTS study, when the effect of central corneal thickness on the development of primary open-angle glaucoma was examined across the range of IOPs, 36 percent of patients with IOPs higher than 25.75 mmHg and corneas 555 µm or thinner were found to have developed glaucoma compared with only 2 percent of those patients with IOPs of 23.75 mmHg or less and corneas thicker than 588 µm.
Risk Assessment Calculator
In cardiology, the consolidation and analysis of cardiovascular risk factors from large patient data sets have led to the development of predictive algorithms that allow physicians to estimate an individual patient's risk of suffering an atherosclerotic cardiovascular event.
This may become possible for glaucoma. An algorithm that would allow ophthalmologists to use a patients' IOP and other risk factors (a so-called risk calculator) to estimate the risk of visual impairment from ocular hypertension and glaucoma would facilitate standardization of treatment for glaucoma and help in determining appropriate treatment for individual patients. Keep in mind, however that, as in the cardiovascular model, a calculator would be an adjunct to and not a substitute for the experience and judgment of a knowledgeable physician.
While we don't yet have all the answers, we are beginning to gather the pieces to the puzzle. This is an important first step. Using further data from the OHTS and other studies, it should be possible to create the first risk assessment calculator for glaucoma.
Dr. Fechtner is a professor at the Institute of Ophthalmology and Visual Science, UMDNJ-New Jersey Medical School, Newark. Contact him at (973) 972-2030 or fechtner@umdnj.edu.
1. Perspective: Risk assessment in the management of patients with ocular hypertension. Am J Ophthalmol 2004;138:458-467.
2. Kass MA, Heuer DK, Higginbotham EJ, et al, for the Ocular Hypertension Treatment Study Group. The Ocular Hypertension Treatment Study. A randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol 2002;120:701-713.
3. Gordon MO, Beiser JA, Brandt JD, et al, for the Ocular Hypertension Treatment Study Group. The Ocular Hypertension Treatment Study. Baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 2002;120:714-720.
4. Girkin CA, Kannel WB, et al. Glaucoma risk factor assessment and prevention: lessons from coronary heart disease. Am J Ophthalmol 2004;138(Suppl):S11-S18.
5. Weinreb RN, Khaw P. Primary open angle glaucoma. Lancet 2004;363:1711-1720.
6. Yucel YH, Zhang Q, et al. Effects of retinal ganglion cell loss on mango-, parvo-, konio-cellular pathways in the lateral geniculate nucleus and visual cortex in glaucoma. Prog Retin Eye Res 2003;22:465-481.
7. Hattenhauer MG, Johnson DH, Ing HH, et al. The probability of blindness from open-angle glaucoma. Ophthalmology 1998;105:2099-2104.
8. Wilson MR. Progression of visual field loss in untreated glaucoma patients and suspects in St. Lucia, West Indies. Trans Am Ophthalmol Soc 2002;100:365-410.
9. Heijl A, Leske MC, Bengtsson B, et al., for the Early Manifest Glaucoma Trial Group. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol 2002;120:1268-1279.
10. AGIS Investigators. The Advanced Glaucoma Intervention Study (AGIS): 12. Baseline risk factors for sustained loss of visual field and visual acuity in patients with advanced glaucoma. Am J Ophthalmol 2002;134:499-512.
11. Lichter PR, Musch DC, Gillespie BW, et al, and the CIGTS Study Group. Interim clinical outcomes in the Collaborative Initial Glaucoma Treatment Study comparing initial treatment randomized to medications or surgery. Ophthalmology 2001;108:1943-1953.