Cataract surgeons are often faced with some unwanted yet unavoidable issues in their patients outside of cataract removal, and thus must be ready for the unexpected. One such scenario relates to cataract patients who underwent a previous glaucoma surgery and have an overfiltering trabeculectomy. Patients may present asymptomatic or with complaints of blurred vision, and it’s imperative for cataract surgeons to accurately address the overfiltration and IOP with the best course of action. Failure to do so could affect IOL calculations.
We spoke with glaucoma specialists to hear how they approach these patients and their recommendations for successful visual outcomes.
Recognizing the Signs and Symptoms
The goal of any trabeculectomy is to lower the eye pressure in glaucoma patients, but sometimes, a trabeculectomy can work too well and the pressure can get too low and the patient can become hypotonous.
Overfiltration typically develops early on following the glaucoma surgery, either immediately after or after releasing the scleral flap sutures, says Jody Piltz-Seymour, MD, who is an adjunct professor at UPenn’s Perelman School of Medicine and an attending at Wills Eye Hospital. However, she’s also seen patients present with late overfiltration.
“One was a young man who started heavy weight lifting about three years after his trabeculectomy and he became hypotonous with the development of macula striae in his only eye,” Dr. Piltz-Seymour says. “And we’ve seen overfiltration and hypotony develop late in some patients treated with anti-VEGF agents, but most of the time, it usually presents early in the postop period.”
Patients can present in three different ways. “One is that they don’t notice anything. Many eyes can tolerate a low eye pressure and the patient remains asymptomatic,” Dr. Piltz-Seymour says. “But some patients with overfiltering blebs can develop bleb dysesthesia or blurred vision. Bleb dysesthesia develops when the elevated contour of the bleb interferes with how the lid interacts with the surface of the eye. Normally as we blink, the eyelids spread the tears smoothly over the corneal surface. But if you have a large, bullous bleb, as the lid passes over that bleb, it may not come in contact with the superior cornea and you get dry spots and irritation. Dellen may also develop.”
 |
Bleb dysesthesia presents with pain, irritation or foreign body sensation, continues Dr. Piltz-Seymour. “It can be a mild annoyance or severely debilitating for some people. Others can develop bubble dysesthesia, where each time they blink a little bubble forms between their lid and the limbal edge of the bleb and makes these little pops every time they blink. If overfiltration causes hypotony issues, patients may have blurred vision and this needs to be addressed to restore the patient’s optimal vision,” she says.
According to Erin A. Boese, MD, a clinical assistant professor of ophthalmology and visual sciences at the University of Iowa, not all hypotony is created equal. “The hard part about hypotony and overfiltering trabeculectomy is that it’s not the same in everybody,” she says. “There are some people out there who might do great with a pressure of 3 or 4 mmHg and not have any problems with hypotony, then there are some people who might have pressures even higher than that and still have issues. So it’s really from the symptoms and exam where we differentiate the people whose pressure is too low vs. doing well.”
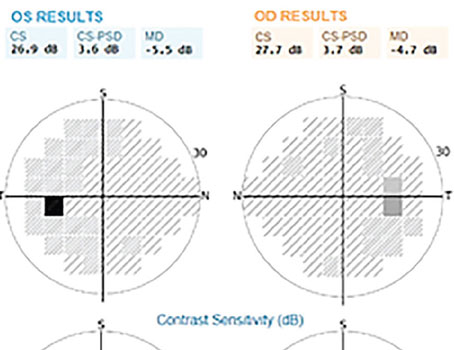
Dr. Boese says complaints of shadows in the periphery could be caused by choroidal effusions, and blurred/distorted vision could be hypotony maculopathy, which would appear as wrinkling on the macula during an exam or by using OCT.
Bleb overfiltration that causes hypotony can lead to blurred vision from multiple mechanisms. “Blurred vision from overfiltration has numerous etiologies. You can sometimes see subtle vertical pooling of fluorescein on the corneal surface that I refer to as tear striae that can be associated with mild blurred vision,” says Dr. Piltz-Seymour. “Hypotony can also lead to serous choroidal detachments, which usually, but not always, resolve. Patients may develop shallow anterior chambers, which can usually be treated conservatively if not severe, and there’s an increased risk of cataract development with low IOPs. But the thing that’s really the most detrimental to vision is hypotony maculopathy. Fine macular striae can cause marked visual compromise and if not treated in a timely fashion, can lead to permanent deficits, even if the pressure is raised. Tear striae and shallow chambers resolve if the pressure goes up, choroidals usually resolve spontaneously or can be drained, but hypotony maculopathy, if not fixed, can really cause long-term problems. You don’t want to sit on hypotony maculopathy for too long.”
Treatment in the Presence of a Cataract
Dr. Boese says removing a cataract with a bleb present causes a surgeon to think differently, and those considerations compound when the bleb is overfiltering. “In some people you just want to nudge their pressure up by a couple of points and in others where the pressure is way too low, you really need to just completely start new to bring it up a lot. Depending on the situation, your approach might differ,” she says.
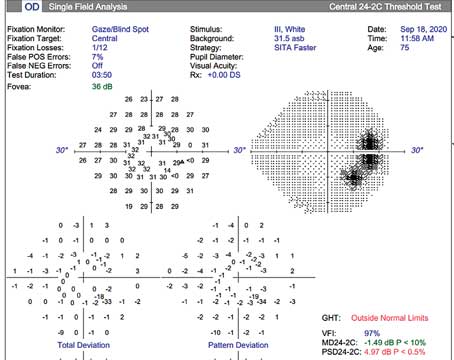
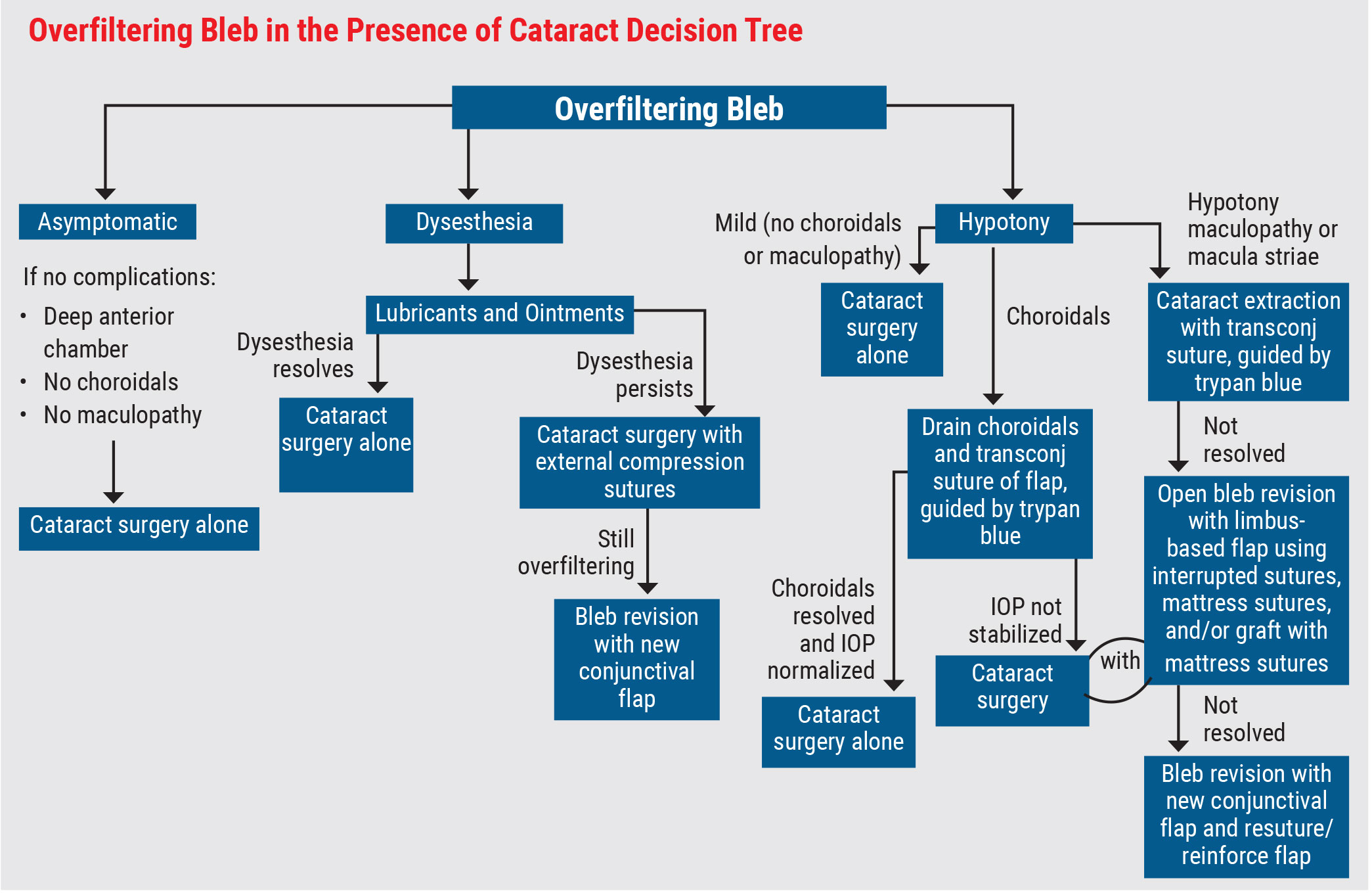
Dr. Piltz-Seymour agrees, adding that there are multiple paths the procedure could take depending on what issues the patient is experiencing due to the overfiltering bleb. (See Decision Tree, above)
Here are their recommendations for the possible scenarios:
• Treatment in asymptomatic patients. If the patient has no other complications and their IOP only needs to come up a slight amount, cataract surgery itself might do the trick.
“If you’re just slightly low and you’d like to see that pressure come up a little bit, one of the things that you can do is take advantage of a little bit of the inflammation that comes with doing the cataract surgery,” says Dr. Boese. “It’s not much but you don’t need a lot either. Normally if I have a well-filtering bleb—it’s not overfiltering—and I do cataract surgery, afterwards I’m using lots of topical steroids, way more than I would normally to help keep that trabeculectomy functioning as well as it did beforehand. But if I’m hoping to elevate the pressure a little bit, I don’t want that trabeculectomy to work as well. In that scenario, I might use considerably fewer postop topical steroids, or in some cases, maybe no steroids at all, because I’m just hoping to harness some of that intraocular inflammation to promote that subconjunctival fibrosis scarring. I think that’d be the easiest thing when you’re just looking for a little bit of an increase in IOP.”
Although not a new technique, Dr. Boese suggests an autologous blood patch as an option. “I think it’s something that deserves a little bit more credit because it’s not very invasive and it’s a technique that can help in some patients,” she says. “The blood patch can be a good tool when you have reasonable expectations and only when you’re trying to move the pressure up by just a couple points. It’s not going to be your tool if you’re looking to get that pressure up significantly. One of the nice things is it can be done safely in the clinic. You don’t have to take the patient to the OR.”
However, cataract surgeons may not be as familiar with the technique as glaucoma surgeons. Dr. Boese says it helps to have a second person there who draws up a little of the patient’s blood from the antecubital vein and gives that syringe to the surgeon.
“You quickly put in a small needle, usually a 30-gauge is just fine, and then you go into the bleb itself,” she says. “You want to start peripherally where the conjunctiva is more healthy. Go into the bleb itself, unlike needling where you’re actually sweeping and breaking up some of those loculations, you actually would just want to gently pierce into these loculations and inject a small amount of blood. You end up seeing these patchy pockets of blood overlying the flap as well as in that overfiltering subconjunctival space. The idea is that blood itself is inflammatory, so by putting blood in this space, you’re trying to promote subconjunctival fibrosis. It doesn’t work for everybody, but it only takes a few minutes and in some cases, it’s all they need.
“Of course afterwards, you’re not going to be putting them on steroids because the whole idea is letting that inflammation help you out,” continues Dr. Boese. “I think it’s an underutilized tool and a nice thing to pull out when you’re trying to see if something in clinic might be enough.”
• Treatment in patients with bleb dysesthesia. Dr. Piltz-Seymour says the first step for bleb dysesthesia is conservative, with lubricants and ointments to help smooth the ocular surface. If the issue resolves itself after that treatment, she would proceed with cataract surgery. “However, if dysesthesia persists, anything you can do to flatten out the contour of the bleb is beneficial,” she says. “I typically place external compression sutures, that’s usually our best bet. Others also recommend using techniques like using trichloroacetic acid or painting the bleb with Rose Bengal and using laser or using cautery. I’ve tried these techniques, but haven’t found them as helpful as external compression sutures. If the compression sutures don’t do the trick, I do a bleb revision, excising the bulk of the old bleb and pulling down fresh conjunctiva.”
• Treatment with hypotony. If the patient requires a significant boost in IOP, Dr. Boese recommends a surgical revision. “This is the most effective way to increase the IOP, even though it means an extra trip to the OR,” she says. “A surgical revision involves replacing the nylon sutures in the scleral flap as a way to decrease the flow through the trabeculectomy flap.”
Dr. Boese cautions that this addresses the root cause of the problem, but could unintentionally spike the patient’s pressure too high. “Surgeons have to be prepared and think multiple steps ahead,” she says.
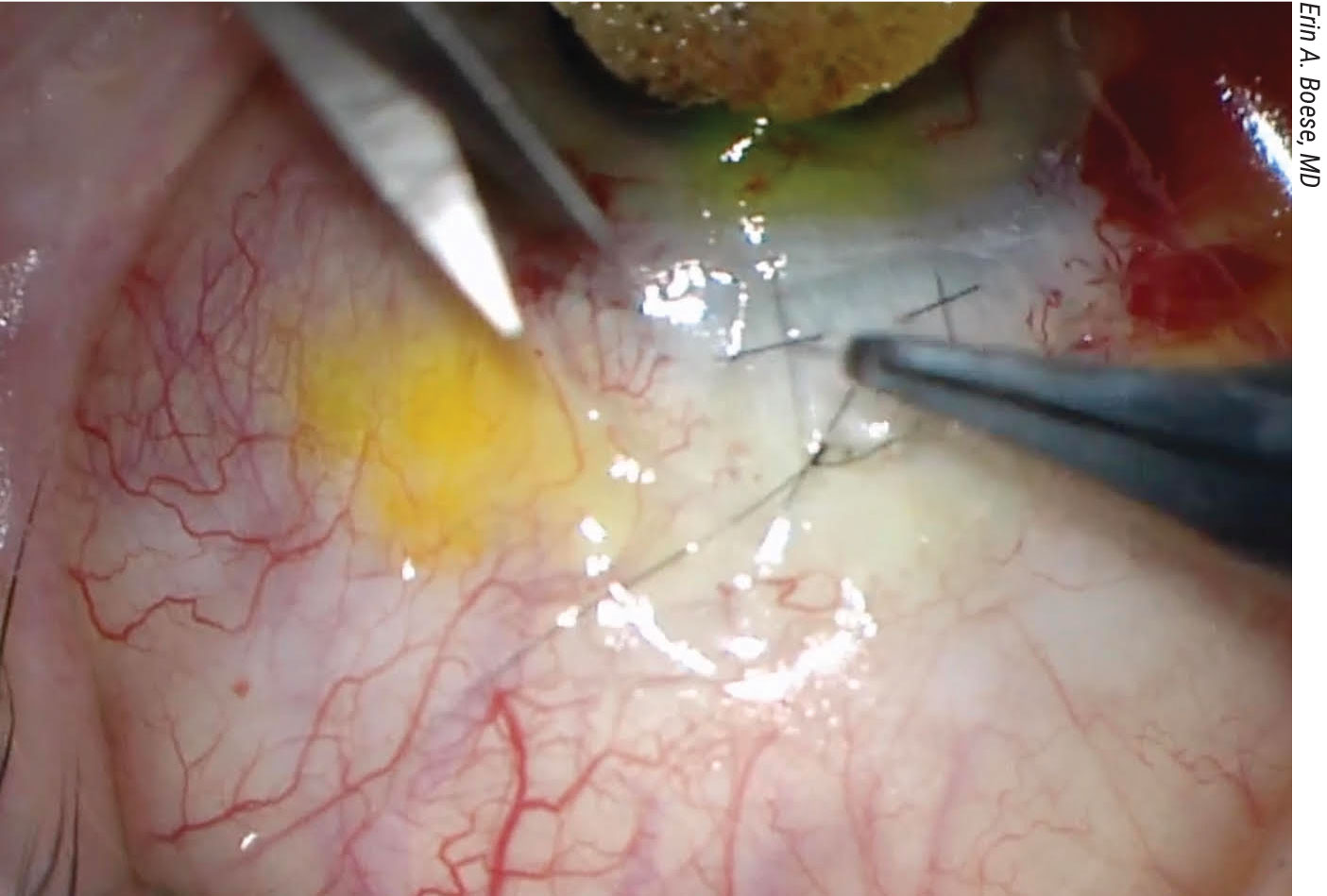
For the severe cases involving hypotony maculopathy or macular striae, Dr. Piltz-Seymour has several considerations. “During cataract surgery, my first recommendation is to place transconjunctival sutures through the scleral flap to try to close down some of the flow through the trabeculectomy flap,” she says. “Many people think the bleb filters in all areas along the scleral flap, but when a trabeculectomy develops, there’s typically only a very localized place on the scleral flap that drains—a small localized fistula—so you need to find out where that spot is in order to put your sutures. I recommend injecting trypan blue into the anterior chamber and then, as the stained aqueous drains from the flap, it will mark the location of the localized fistula. You only need to place transconjunctival sutures in this location. You can place a couple of sutures and that’ll usually help to raise the pressure.”
If that doesn’t work, she creates a limbus-based conjunctival flap by incising the conjunctiva posterior to the bleb in the fornix. “Reflect the bleb over the cornea and then try to reinforce the flap either with additional interrupted sutures, mattress sutures or by securing graft material over the flap to tamponade it with mattress sutures,” says Dr. Piltz-Seymour. “I want to stress that if you need to place a graft, use mattress sutures over the graft to put pressure on the bleb; interrupted sutures around the edge of the flap are less useful. And trypan blue again can help to identify the exact area of overfiltration.”
 |
|
Performing a surgical revision of the bleb is a good way to proceed if you need a significant increase in IOP to avoid the consequences of doing cataract surgery on a hypotonous eye. This should be done prior to the cataract surgery to ensure that optical measurements are made with the eye at a normal pressure. |
She emphasizes that, in the presence of macular striae, you really need a definitive approach to raising the IOP. “We sometimes like to elevate the pressure into the 20s for a short time to flatten out that macula and then have a plan to lower the IOP back to the target level,” Dr. Piltz-Seymour says. “When securing the scleral flap either with transconjunctival sutures or an open technique, it’s advisable to place two sets of sutures, tight ones to initially raise the IOP into the low 20s that can be released, and looser ones to stay long term. If using graft material over the flap, the tight sutures will need to be releasable sutures. In reality, it may not be that easy to titrate the IOP with tighter and looser sutures, especially when placed transconjunctivally, since the actual fistula is so localized. Usually, what I recommend is to take out the cataract, place the transconjunctival sutures and if I don’t get the result that I want, plan to do an open approach.”
Finally, as a last resort, you can excise the old bleb, secure the flap as described above, and bring fresh conjunctiva down, Dr. Piltz-Seymour continues.
IOL Calc Considerations
Hypotony can impact IOL calculations and in extreme cases should be addressed prior to taking those measurements, say both surgeons.
“A hypotonous eye becomes shorter, and if the hypotony reverses, the eye expands, but not usually to the full baseline axial length,” says Dr. Piltz-Seymour. “Whether you performed biometry measurements before the hypotony developed or after, there will be issues with IOL accuracy.”
Dr. Boese says calculations may not be thrown off too much if the pressure only needs to come up slightly, but it still influences her target. “If I’m planning to do cataract surgery along with a glaucoma surgery and I’m planning to lower the pressure I might choose a slightly more myopic target because I know that eye might be a little bit shorter,” she says. “The opposite might be true for when I’m purposely trying to increase the axial length and increase the eye pressure. I might end up picking a target closer to plano or even slightly hyperopic if I’m really pretty certain that I can get that axial length a little bit longer. I think in general, a lot of us prefer to be slightly myopic than slightly hyperopic, so I just might not need to aim quite so myopic with my calculations.”
Astigmatism is another factor to consider. “One thing to be wary of is when that pressure is low, not only will your axial length be changed and your IOL calcs be different, but it can also trick you into thinking that there’s a lot more astigmatism in the eye than there actually is,” Dr. Boese continues. “The eye actually can have pretty significant regular with-the-rule astigmatism just because the eye is sinking in on itself a little bit. If you were to look at that out of context, you might say, ‘Well, gosh, I might put a toric lens in this person,’ and actually end up inducing astigmatism when the pressure goes up.”
Similarly, if additional flap sutures are going to be placed, changes in astigmatism can develop, adds Dr. Piltz-Seymour. “Patients need to be warned that there may be a need for glasses if the adjusted measurements aren’t right on the mark. Most of these patients won’t be multifocal candidates so postoperative vision can be corrected with glasses if needed.”
In order to achieve optimal outcomes, Dr. Boese says preop planning is going to be your best friend.
“Not only are there all of those impacts on the IOL calculations, but you also want to make sure you’re setting patient expectations appropriately,” she says. “Hypotony can be hard to fix. It’s so much easier for us to lower a high pressure than to raise a really low one. Have realistic expectations of what you can expect with each of these tools, and also decide whether or not you want to address the hypotony and cataract in a staged approach. Cataracts can usually wait. If delaying the cataract surgery with a staged approach works better and it puts you in a better position for good outcomes, I don’t think anyone would fault you for that.”
Dr. Boese reports no financial disclosures. Dr. Piltz-Seymour is a consultant and speaker for Aerie Pharmaceuticals and Alcon; and consultant for Nanoscope Therapeutics.