Primary angle-closure glaucoma affects 20 million people worldwide and is a leading cause of irreversible blindness. Because the crystalline lens plays a major role, some argue, lens extraction is a useful intervention. Another option, of course, is laser peripheral iridotomy.
According to Alliance, Ohio’s, Richard Lehrer, MD, there are five factors to consider in patients with narrow angles. “In these patients, I consider the following: whether they have elevated pressure; the presence of a cataract; their age; whether they have any visual dysfunction due to cataract; and whether I think on gonioscopy their angle is occludable. If the person is a young patient with very little cataract, no visual dysfunction, no nerve damage, and no elevated pressure, usually I would lean toward an iridotomy. But, if the patient is a little bit older, has an incipient cataract, has any sign of disc changes or a family history of glaucoma, and has any visual dysfunction that could be attributed to cataract, I would definitely lean toward cataract surgery.”
He adds that there are some rare people who have a very crowded anterior segment. In these patients, removing the cataract and implanting an IOL doesn’t necessarily relieve the narrow angle. “These would be patients who have plateau iris and similar configurations,” he says. “In those cases, especially if they have glaucoma, I might even recommend doing endocyclophotocoagulation at the same time in order to shrink the ciliary body and create a lot more space in the eye. Having a peripheral iridotomy present in those patients can be helpful, in addition to taking out the cataract.”
 |
|
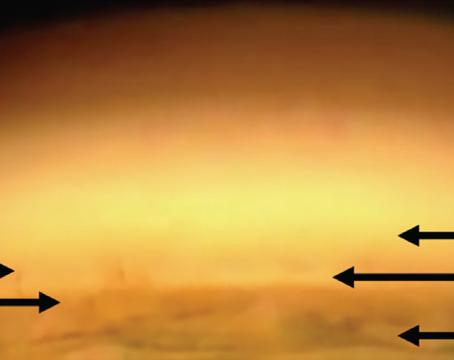
A relatively young patient with narrow angles and a clear lens is a good candidate for a peripheral laser iridotomy, experts say. (Photo courtesy of Kurt Chamberlain MS, Justin Risma, MD, Wallace L. Alward, MD, and Brice Critser, CRA.) |
When to Consider an Iridotomy
If a patient presents with anatomically narrow angles and a clear lens, and is relatively young with no angle structures seen on gonioscopy, Duke University’s Sanjay Asrani, MD, recommends proceeding with a prophylactic laser iridotomy.
“However, the ZAP study found a low risk of an angle closure event when patients have anatomically narrow angles, so it may not be necessary to proceed with the prophylactic laser iridotomy,” Dr. Asrani explains. “But, this study has some caveats. It was done in a purely Chinese population, and it was primarily looking at events such as an angle-closure attack or synechiae in the angle. Additionally, it didn’t assess for vascular events, and it was a general population, not the population that presents to an eye clinic. Having said that, the population that we deal with in the United States is likely different. Our population has a higher possibility of borderline blood sugar, which leads to a higher lens thickness because of sorbitol that enters the lens. The other is that our population here in the United States is more likely to take over-the-counter medications that have anticholinergic side effects that can lead to angle closures, in contrast to the Chinese population that doesn’t frequently take over-the-counter medications. So, there are some significant differences between the population that was studied in that study versus ours.”
The ZAP study is a randomized controlled trial in which bilateral primary angle-closure suspects aged 50 to 70 years were enrolled at the Zhongshan Ophthalmic Center in Guangzhou, China.1 Eligible patients received laser peripheral iridotomy in one randomly selected eye, and the other eye didn’t receive treatment.
The study included 889 treated eyes and 889 untreated eyes, and the primary outcome was incident primary angle-closure disease as a composite endpoint of elevation of intraocular pressure, peripheral anterior synechiae, and acute angle-closure during 72 months of follow-up in an intention-to-treat analysis between treated eyes and contralateral controls. The incidence of the primary outcome was 4.19 per 1,000 eye-years in treated eyes compared with 7.97 per 1,000 eye-years in untreated eyes. A primary outcome event occurred in 19 treated eyes and in 36 untreated eyes.1
The ZAP study found that laser PIs had a modest, albeit significant, prophylactic effect. Because of the low incidence rate of outcomes that have no immediate threat to vision, the benefit of prophylactic laser peripheral iridotomy was limited, and the researchers concluded that the use of widespread prophylactic laser peripheral iridotomy for primary angle-closure patients isn’t recommended.
Dr. Lehrer notes that, even though the ZAP study found that doing laser may not necessarily reduce the risk of going on to develop narrow-angle glaucoma, most ophthalmologists lean toward treatment versus observation if they think the angle really is occludable. “I determine that by gonioscopy, usually in a dark room,” he explains. “Many people use scanning technology with OCT and other modalities, like UBM and Scheimpflug imaging. This can be very helpful in showing us which angles are truly occludable. So, if you definitely have an occludable angle, and the patient is in the dark-room situation, and he or she has never had an angle-closure attack, then I would definitely lean toward treatment.
“If they’ve had an angle-closure attack in one eye already,” Dr. Lehrer continues, “I think they need preventive treatment in their other eye, once the narrow-angle-attack eye has been taken care of. It’s a whole different ballgame once they’ve already had a narrow angle attack, or if they have symptoms consistent with intermittent narrow angle attacks.”
Dr. Asrani agrees. “At academic medical centers, we keep seeing patients coming in with acute attacks of glaucoma, which aren’t as rare as that study would lead us to believe,” he says. “So, a procedure that might prevent an angle-closure attack or that might prevent intermittent angle closure, which can lead to trabecular meshwork damage in the long-run and can ultimately raise pressures in the future, is a good idea. Therefore, I typically recommend a laser prophylactic iridotomy to such patients. Of course, I’m not talking about people who are just borderline occludable. In those cases, I might wait and watch.”
He explains that there’s a significant possibility of trabecular damage in the long run due to intermittent angle closure, especially in patients who have large pupils and a phaco-morphic component. “So, these patients may not have synechiae, which is irreversible evidence of scarring in the trabecular meshwork, but, periodically, the iris damaging the trabecular meshwork cells can lead to raised intraocular pressure many years down the line,” Dr. Asrani says.
When to Consider Cataract Surgery
According to Brian Francis, MD, in practice at the Doheny Eye Institute in Los Angeles, most ophthalmologists agree that cataract surgery is best for patients with narrow angles and a visually significant cataract or a cataract that’s borderline visually significant. “Obviously, it will anatomically cure the narrow angle, so it’s more of a permanent cure than an iridotomy, and you get the added advantage of improving vision, especially if the patient has a visually significant cataract,” he says. “Generally, these patients are hyperopic, so you can improve the quality of their vision because they’re no longer hyperopic. You can make them emmetropic. You can even give them a multifocal lens to improve their near vision, as well. So there’s a lot to be said for doing the surgery, especially if the patient has a nearly significant or visually significant cataract.”
He adds that there has been controversy surrounding whether these patients require a peripheral iridotomy before undergoing cataract surgery. “I don’t believe they do,” Dr. Francis avers. “Some doctors believe that if the patient is dilated for cataract surgery, he or she could potentially go into angle closure. I don’t think that’s necessarily valid. If you dilate someone and take him or her directly to the operating room, you should be able to control for that. A young patient with no cataract is a little bit more controversial. In these patients, you can consider an iridotomy instead of a clear lens extraction, basically. But, again, there is something to be said for lens extraction in these patients because you’re going to make their quality of vision better by making them emmetropic instead of hyperopic. If someone has an iridotomy and is still narrow or still has high pressures, I think that’s an indication for taking out the lens, even if it’s a clear lens extraction.”
Dr. Asrani says that he doesn’t typically perform clear lens extractions for patients with borderline pressure and/or evidence of mild glaucoma. “However, there are exceptions in which I see that one eye already has severe glaucomatous damage, and the eyes obviously have what is called a very high lens vault, which is a big phacomorphic component of the glaucoma, and they’re already not adequately controlled on practical glaucoma medications,” he explains. “I’ll go ahead and recommend a clear lens extraction in those cases. But, in general, I do not, because after I remove the cataract, in all cases I can’t be sure that I’ll be able to achieve glaucoma or pressure control because I don’t know the level of the underlying damage of the trabecular meshwork that’s already there. I don’t want to recommend a clear lens extraction only to realize, after taking the lens out, that the pressure is still uncontrolled because there’s already irreversible trabecular meshwork damage.”
In the EAGLE study, clear-lens extraction showed greater efficacy and was more cost-effective than laser peripheral iridotomy.2 The researchers determined that it should be considered an option for first-line treatment.
The EAGLE study enrolled patients from 30 hospital eye services in five countries. Patients were assigned to undergo clear-lens extraction or receive standard care with laser peripheral iridotomy and topical medical treatment. Eligible patients were aged 50 years or older, didn’t have cataracts, and had newly diagnosed primary angle closure with intraocular pressure 30 mmHg or greater or primary angle-closure glaucoma.
Of the 419 participants enrolled, 155 had primary angle closure, and 263 had primary angle-closure glaucoma. Two hundred eight patients were assigned to clear-lens extraction, and 211 were assigned to standard care. Additionally, 351 (84 percent) had complete data on health status, and 366 (87 percent) had complete data on intraocular pressure. The mean health status score, assessed with the European Quality of Life-5 Dimensions questionnaire, was 0.052 higher and mean intraocular pressure was 1.18 mmHg lower after clear-lens extraction than after standard care.2
“There’s pretty compelling evidence that taking out the lens is basically curing the problem, so it’s preferable in most cases, unless the patient is young, has no cataract at all, has 20/20 vision, and isn’t at high risk for angle closure,” says Dr. Francis. “Then, it makes sense to do an iridotomy until the patient reaches that point or needs his or her cataract done. I also think it’s important to tell patients that an iridotomy isn’t curative. The iridotomy will change the anatomy and will help prevent angle closure but, over time, you’ll get progressive narrowing of the angle due to enlargement of the lens from cataract formation, so they’re going to eventually need surgery at that point. The PI just buys you time. In many cases, it can buy you several decades before you need surgery.”
Cataract surgery has significantly improved in the past 20 years, and the lens designs have also improved. “You can argue that the lens designs will be even better 10 years from now, so if you can postpone a patient’s cataract surgery and do an iridotomy to cover the next 10 years, the patient may end up doing even better,” Dr. Francis muses. “It’s an interesting conversation. There’s no real right or wrong answer, but I think the tide is shifting a little bit more toward lens extraction.”
Drs. Asrani, Francis and Lehrer have no relevant financial interests to disclose.
This article has no commercial sponsorship.
1. He M, Jiang Y, Huang S, et al. Laser peripheral iridotomy for the prevention of angle closure: A single-centre, randomized controlled trial. Lancet 2019;393:10181:1609-1618.
2. Azuara-Blanco A, Burr J, Ramsay C, et al, EAGLE study group. Effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE): A randomized controlled trial. Lancet 2016;388:10052:1389-1397.