Only health-care employees face this challenge: the possibility that what was exemplary job performance just a few years ago could today draw charges of gross negligence. Since the 1950s, practitioners have relied on continuing medical education to stay informed about evolving health-care standards, and almost every state mandates some minimum of CME credits for re-licensure. In short, everyone agrees on CME’s vital contributions to the profession.
Unfortunately, among interested parties, that is largely where agreement ends. Over the past decade, the CME world has undergone a sort of slow-moving, self-appraising upheaval, mainly centered upon what role the pharmaceutical industry should play in the funding and content of educational courses. Between 1990 and 2006, spending on prescription drugs in this country grew fivefold.1 As their market expanded, pharmaceutical companies began taking greater interest in physician instruction. Between 1998 and 2007, direct commercial contributions to CME activities quadrupled, from $301 million to $1.2 billion.2 Critics said those funds amounted to veiled advertising, and matters culminated in a 2007 Senate hearing during which the CME industry took a public beating. Although the debate sparked reforms that put barriers on bias and commercial influence, and by 2013 industry’s CME contributions had receded to $666 million, the backlash continues. Many critics are still calling for additional, stricter reforms, and some for the complete elimination of industry funding. The most recent hot-button issue has been whether CME will be exempted from the Affordable Care Act’s so-called “Sunshine Act” provisions. (See Here Comes the Sun, right).
|
On a different level, CME is undergoing other, less volatile changes as well. Education providers are moving away from traditional, lecture-hall-centered formats in favor of more interactive, competency-based strategies that include online teaching tools, point-of-care CME and patient outcomes measurement aimed at tracking practitioner performance improvement. If some of these efforts are successful, they could radically change the way physicians acquire professional development in the years ahead.
The Wild West
Ophthalmology has long had a pro-scholarship mien. In 1916, it was the first specialty to establish a board, the American Board of Ophthalmology, which in turn was one of the founding members of the American Board of Medical Specialists (ABMS) in 1933. A decade ago ophthalmology led the way among specialties in creating a core curriculum (the Practicing Ophthalmologists Curriculum), which has served as a model for other medical societies seeking to devise educational criteria. It can even be said that many of the changes described in this article owe a great deal to the efforts of one particular ophthalmologist, Bruce E. Spivey, MD, MEd, MS.
When he became president of the Council of Medical Specialty Societies in 2000, one of Dr. Spivey’s first acts was to appoint a task force to investigate ways to reform and reposition CME. The task force, named The Conjoint Committee on CME, issued its first report in 2002, and has released several others since then. The committee’s works have served as foundational documents for many of the reform efforts that have occurred over the past decade. One of its main themes is the call for greater reliance on adult learning techniques, such as “directed self-learning” and “non-traditional” educational approaches.
“The effectiveness of traditional CME has been questioned for some time,” Dr. Spivey has written about his decision to appoint the task force. “The literature documents a lack of behavioral change as a result of the traditional lecture format, and a variety of alternatives to traditional CME have been proposed.
“The idea was not to not to dismiss all aspects of present CME,” Dr. Spivey continued, “but to systematically review the literature and the variety of proposals for change that have been expressed.”
At the core of Dr. Spivey’s motivation was the idea that that CME system as it existed left considerable room for improvement. In one paper he wrote: “Throughout most of our CME experience, the predominant modality of delivery is journals and the large lecture hall—dimly lit, sporadic in focus, often with topics primarily of interest to the speaker (teacher) and too often, an opportunity for la siesta. And even if a lecture is captivating, a number of studies have demonstrated that isolated, single-exposure, lecture based CME does not result in physician behavior change.”3
Around this time, scrutiny also began to fall on the burgeoning influx in commercial money to the CME system. In 2003, the Department of Health and Human Services issued guidelines prohibiting those with commercial interests to have control over certified CME content. The following year, the Accreditation Council on CME, the organization that credentials CME providers, updated and strengthened its “standards for commercial support” of CME activities. The new standards set criteria for independence, resolution of conflicts of interest, and development of unbiased content. In 2007 the ACCME strengthened those standards and broadened the definition of “commercial interest,” requiring all CME providers to cut off all relationships with industry marketing/promotional employees. In 2009, it implemented rapid response measures to identify compliance infractions and place accredited providers on probation.
One industry-sponsored white paper refers to the period before 2005 as the “pre-reform era,” and puts forth the notion that any studies based on data from that time period should be considered outdated.4 The authors add: “Some CME professionals looked back on the period between 1984 and 2004 and labeled it the ‘wild west.’ While this may be an overstatement, there were a number of unhealthy practices in need of reform, including but not limited to dialogues between CME funding organizations and accredited providers regarding faculty selection and content.”
The pre-reform era’s laissez-faire approach to ethics finds confirmation elsewhere. In her blog, “CME in the Raw,” Brandee Plott describes starting out as pharmaceutical rep in the 1990s and working her way up to a medical education professional. “When I hear stories about the bad actors who gave medical education a bad public reputation, I believe all of it and more because I’ve seen it with my own eyes,” she wrote in a post last year, recounting a cardiologist who offered to prescribe her company’s drug more frequently if she would agree to send him to an “advisory board” meeting at a five-star hotel in the tropics. Describing her time at a medical communications company in the early 2000s, she wrote: “Back then pharma companies were not called commercial supporters. They were just called clients. I organized a CME satellite symposium at the biggest infectious disease meeting of the year. The pharma company’s marketing department sent the faculty slide sets for their presentations, and during the final slide review, it was the pharma company’s product manager calling the shots.”
Such behavior no longer occurs, she says. “People in the industry on the provider side, pharma side and organizations like the ACCME, IOM [Institute of Medicine] and others cared enough about CME to come together and make some major changes. Now, medical education is evidence-based and commercial support is closely regulated.”
Masked Marketing?
While reforms have had a positive impact, many critics believe they have failed to address some fundamental issues, and commercial funding therefore remains problematic. As the general public’s favorable opinion of large pharmaceutical firms continues to decline, calls for additional regulation have found a sympathetic audience. A report published by Pew Charitable Trusts last year recommended the elimination of all industry-funded CME wherever possible. “In situations where industry funding is nonetheless being considered, academic medical centers should implement additional safeguards beyond compliance with the [ACCME]’s Standards for Commercial Support,” the report concluded. “Examples of such safeguards might include: creating a ‘blinded’ pool of industry funds; requiring that any activity be funded by more than one company; calling for physicians to use some of their own money (such as paying for their own meals); and locating the continuing medical education activity within an academic setting or other appropriate venue conducive to education [instead of vacation resorts, etc.].”
Concerned about the knotty ethical questions still extant, in recent years some academic institutions and health-care systems have taken the step of declining industry supported CME programs altogether, the report notes. These include Memorial Sloan-Kettering Cancer Center; Stanford University Medical Center; University of Michigan Medical School; Kaiser Permanente; and Brody School of Medicine of East Carolina University.
Even the American Medical Association, hardly a hotbed of radical politics, saw fit in 2011 to speak out against industry-funded CME. Its Council on Ethical and Judicial Affairs concluded that CME activities should be developed without industry support “when possible,” and adopted ethical guidelines discouraging both industry funding and CME lecturers who have relationships with industry.
Another broadside aimed at industry funding erupted late last year from a pair of Journal of American Medical Association articles. In one, a retrospective study of 2010 grant registries of 14 pharmaceutical and device companies, investigators found that, of 6,493 recipients of more than $657 million in industry-sponsored grant awards, privately owned communication firms received 26 percent of the grant money—more than academic medical centers or disease-targeted organizations.5
In the companion article, Lisa M. Schwartz, MD, MS and Steven Woloshin, MD, MS, of the Center for Medicine and Media, Dartmouth Institute for Health Policy and Clinical Practice, delivered a cri de coeur against private CME providers that accept money from industry: “All companies will feel unconscious (and perhaps explicit) pressure to present their clients’ products in the best light. Bias can easily occur in the selection and training of speakers, in their presentations, on the websites, and even in the test questions.”6
Elaborating on the editorial, Dr. Schwartz explained the question was not so much whether industry directly influences content, but rather whether CME providers paid millions by industry could reliably produce objective content about that industry. “If the financial entity as a whole is beholden to a particularly high-paying customer, to what degree does that influence produce content to satisfy that customer? The [companion] article documented how much money is coming from pharmaceutical companies into CME. It’s substantial. Industry wouldn’t necessarily be happy with content that portrayed their products in a negative way. That’s the concern.”
Puncta Caecum
Though it is possible to find practitioners with strongly held opinions on both sides of the CME funding issue, most fail to see it as more than a minor concern. Physicians tend either to believe that industry has little influence on CME course material, or that if it does, the profession is smart enough to separate facts from marketing, according to Adriane Fugh-Berman, MD, an assistant professor of pharmacology and physiology at Georgetown University, and director of PharmedOut, an industry watchdog organization.
What many practitioners fail to realize, Dr. Fugh-Berman explains, is that marketing for a new drug can begin as long as seven to eight years before it gains Food and Drug Administration approval. Companies may put out CME materials about a disease’s prevalence (invariably described as under-diagnosed and underappreciated) or a rival therapy’s inadequacies long before the drug even exists. “Can doctors pick up on overt advertising of a drug? Sure. But you’re never going to see overt advertising in a CME,” she says.
For example, CME may suddenly be inundated with programs about a newly discovered system, such as the endocannabinoid system. “Well, of course that was meant to prepare the market, for—surprise—an endocannabinoid drug.”
But even if we ignore the overt financial and marketing forces that taint industry funded CME, other hazards can undermine the impartial practice of medicine, says Dr. Fugh-Berman. These are non-financial and subconscious inducements.
In a paper published last year by the Journal of Law, Medicine and Ethics, Dr. Fugh-Berman and a co-author explored sales techniques aimed at exploiting subconscious bias.7 Most physicians view with repugnance the idea that they would accept gifts or compensation in exchange for making therapeutic choices. “Physicians who would never, for example, engage in a quid pro quo exchange of money for prescriptions, may believe that such a conscious and genuine commitment to ethical behavior renders them immune to commercial influence. This righteous but wrong assumption derives from not knowing that many psychological processes occur below conscious awareness,” according to the paper.
“For example, studies consistently show that promotion increases the prescription of targeted drugs, yet research also finds that physicians believe their own prescribing behavior is unaffected by industry influence, although they concede that other physicians are susceptible to such influence,” the authors write. Social psychology has found that humans have a “bias blind spot” rendering them more likely to identify bias in others than in themselves, according to the paper.
In addition, CME represents a main avenue for the influence of nonfinancial inducements, which the paper defines as “the use of deference, the opportunity to be revered as an expert, and the publication productivity facilitated by industry-funded ghostwriters that furthers the health care professional’s career.”
Or to put it another way, CME offers the opportunity to become a key opinion leader, a role usually reserved for high-status, respected, academic physicians. Industry not only sends these influential physicians to CME events to sway and guide the opinions of their peers but also dangles the possibly of becoming a KOL to entice rank-and-file practitioners, according to the study. “The industry’s use of opinion leaders is clearly a use of authority, but it also is a use of scarcity—the concept that opportunities are more valuable when they are limited: not every physician is eligible for the plum job of KOL.”7
Dr. Fugh-Berman sees no place for industry funding in any aspect of continuing education, even if that prohibition results in fewer CME events. “We have enough non-industry funded CME just on our [PharmedOut’s] website for physicians to get all of their credits if they want. There’s a lot of CME out there that is not industry funded,” she says, concluding that, “participation in industry funded CME can only worsen your prescribing habits.”
Mistaken Conflation
Defenders of industry-sponsored CME concede that many real and potential conflicts of interests exist in the relationships between commercial enterprises and medical practitioners. However, they contend those conflicts have been misidentified as occurring in the world of accredited CME. There is widespread confusion about the distinction between promotional programs—which often combine educational messages with marketing ones and are sometimes even labeled “education”—and certified CME presented by accredited providers that adhere to ACCME standards, they say.
“Most reports comingle discussion of conflicts under the broad category of ‘education,’ which often includes certified CME activities under the same umbrella as promotional programs that are directly funded by industry,” according to an industry white paper. “The confusion appears to occur when authors and editorialists consider all forms of so-called ‘education’ as certified CME. The CME enterprise often is impugned based on the fact that authors do not acknowledge the separate rules that govern accredited CME providers.”4
Indeed, the JAMA article cited above that studied grant registries made just such an error, according to Murray Kopelow, MD, president of the ACCME. It erroneously lumped medical communication companies together with medical educational companies. “By conflating medical communication companies with medical education companies, the article presents a misleading, inaccurate, and imbalanced picture of accredited continuing medical education and the stringent requirements in place to safeguard its independence,” he said in an interview published on a website that covers event planning and medical meetings.8
|
There is no hint of marketing in anything his company does, Mr. Sullivan says. “At this point everything in this business is pretty much completely separated from marketing. There is no one in marketing involved, even at the smallest company. Our only goal is to educate physicians. It’s no longer about positioning a drug in the marketplace. Those days are long gone.”
Additional reform efforts, especially those imposed by the federal government such as the Sunshine Act, will only result in chasing more industry dollars out of the CME business at a time when health care needs medical education programs more than ever, according to Mr. Sullivan. “We’ve seen commercial funding decline year after year for about the last seven years now. It’s created a sort of perfect storm for doctors, because they are getting less travel money from their employers, and even the government is sending fewer people to conferences. More doctors are taking CME classes online, which is not necessarily a bad thing, but it does cut down on the kind of interaction you get at a live conference where physicians can exchange ideas with experts.”
Of particular concern is the deepening estrangement of primary-care doctors from specialists, says Mr. Sullivan. In decades past, primary-care physicians and specialists would mingle with each other at hospital settings. But now hospitals are increasingly hiring their own full-time physicians, who interact less often with their specialist colleagues in private practice. “When they took primary-care physicians out of doing rounds and put in ‘hospitalists,’ what happened was the primary-care physician now has less access to experts. They don’t talk to specialists because they don’t run into them in the hospital hallway anymore.” More frequent participation in live CME events would help to integrate a health-care system ever more subject to what many call the “silo-ization” of human resources and knowledge, he says.
Virtual OR
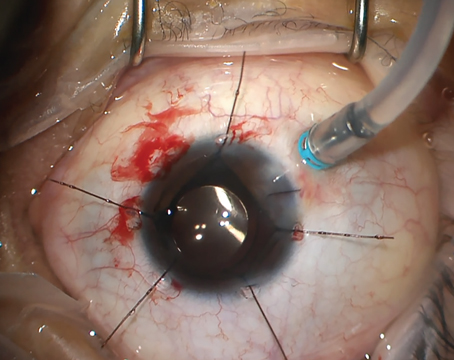
When 41-year-old orthopedic surgeon Selene G. Parekh, MD, MBA, began wearing Google Glass in the OR, it was originally meant as a strategy for live broadcasting educational videos to India, where he had been performing charity clinics for several years. But he soon realized the instructional potential of the device—which is essentially a head-mounted, voice-activated smart phone—was a two-way street.
“In my mind, one of the most significant features Google Glass offers is it can bring any surgeon from around the world into any OR around the world to affect patients’ health,” he explains. If a surgeon encounters an anomaly during a procedure, he or she could, via voice command, contact another surgeon who is an expert in the field and is also wearing a Google Glass. “You can bring that expert into the OR with you at the exact moment when you need help,” he says. “To me that is an amazing power.”
The next generation of learners, the ones who have recently graduated medical school or are in it now, will have a greater interest in learning in this point-of-care fashion, according to Lawrence Sherman, FACEHP, CCMEP, senior vice president of educational strategy at Prova Education. “These people are ready for a fast-paced, ever-changing, lifelong learning environment,” he says. “So we are going to have to keep up with their needs, to provide CME at the point of care, on the mobile device, in the operating room, at places where the clinical question comes up.”
Groundbreaking change, however, will not occur overnight. Although point-of-care and quality-improvement CME credits have been available since 2005, as a practical matter, putting these sorts of CME programs into practice, especially on a global scale that crosses national borders, still presents many daunting challenges, says Mr. Sherman: “Not all best practices cross borders. Not all procedures are the same. Not all formularies are the same. So at the end of the day the education that is developed in the U.S. may not even be relevant in the practice environment in which learners in other countries are operating.”
Unintended Consequences
It seems axiomatic in a field as complex, unpredictable and multifarious as medicine that the manufacturers of the products designed to serve that field should have some sort of official channel of communication to the end-users of those products, no matter how regulated or fiercely guarded that channel may ultimately need to be. Even the Pew report cited above concedes that exceptions to its suggested prohibition of commercial funding be made for device manufacturers to instruct physicians on how to operate new instruments. And the federal government appears to endorse the importance of commercial funding via the FDA’s Risk Evaluation and Mitigation Strategies (REMS) program, which compels pharmaceutical companies to educate practitioners about problematic drugs.
Moreover, the absence of commercially funded CME could force industry to turn to non-accredited educational events, such as dinner lectures at restaurants and satellite symposia at professional society meetings, venues devoid of any oversight whatsoever. A too-harsh stance toward CME regulation could result in “unintended consequences,” according to one journal editorial: “If changes in the CME landscape drive physicians away from accredited events toward these non-accredited activities, the overall state of medical education will not have improved.”9
On the other hand, despite industry’s commendable efforts at self-regulation, the issues of topic choice and true content objectivity remain matters that appear to merit additional scrutiny.
Few believe CME’s long transformation has run its course. When asked if a decade’s worth of reform had had an impact, Dr. Spivey put it succinctly: “It’s a work in progress.” REVIEW
Mr. Celia is a freelance health-care writer based in the Philadelphia area.
1. D. Carpenter. Reputation and Power: Organizational Image and Pharmaceutical Regulation at the FDA. (Princeton: Princeton University Press, 2010).
2. Accreditation Council for Continuing Medical Education. ACCME 2013 annual report data. 2014 http://www.accme.org/sites/default/files/630_2013_Annual_Report_20140715_0.pdf) Accessed Aug. 25, 2014.
3. Spivey BE. Reforming and Repositioning Continuing Medical Education. Saudi J Ophthalmol 2007;21(1):19-24.
4. CME Crossroads: A Survey of Continuing Medical Education Analysis, Criticism, Research and Policy Proposals. Published by Global Education Group, Oct. 2010. Available at: www.globaleducation.com.
5. Rothman SM, et al. Medical Communication Companies and Industry Grants. JAMA Dec. 2013;310(23):2254-2558.
6. Schwartz LM, Woloshin S. Editorial: Medical Communication Companies and Continuing Medical Education, Clouding the Sunshine? JAMA Dec. 2013;310(23):2254-2558.
7. Sah S, Fugh-Berman A. Physicians Under the Influence: Social Psychology and Industry Marketing Strategies. J Law, Med Ethics 2013;41(3):665-672.
8. ACCME Responds to JAMA Articles Slamming ‘Medical Communication Companies,’ by Sue Pelletier. Published on meetingsnet.com. Accessed Aug. 1, 2014.
9. Steinman MA, et al. Industry Support of CME—Are We at the Tipping Point? N Eng J Med March 2012;366(12):1069-1071.