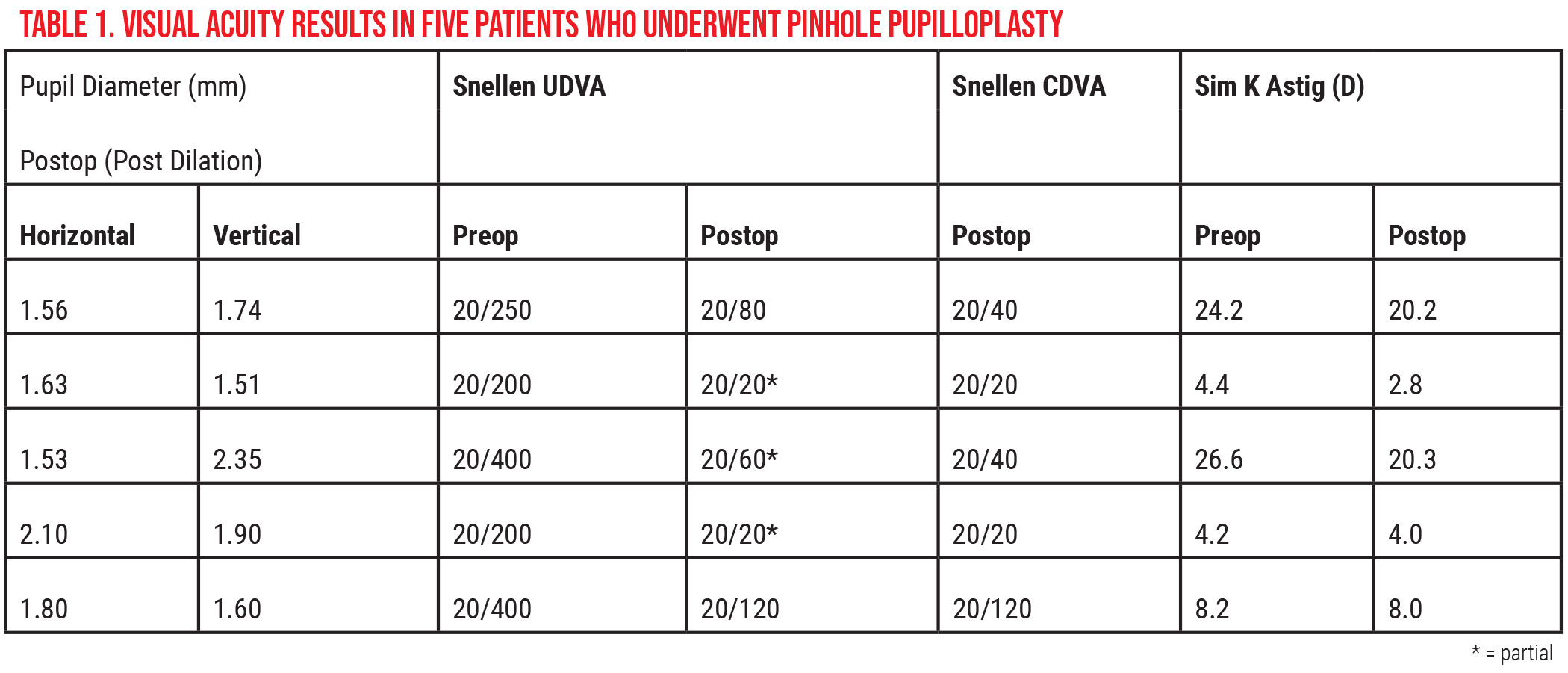
The effectiveness of small-aperture optics for patients with irregular astigmatism is well-known, leading manufacturers to develop IOLs with an integrated pinhole to improve visual acuity. However, there are still areas of the world where such devices aren’t yet available or may not be viable for certain patients. Driven by their motivation to make patients happy, a group of surgeons developed and studied a new technique, dubbed the “pinhole pupilloplasty,” with the goal of improving visual acuity and reducing aberrations. We spoke with one of the lead authors, Priya Narang, MD, MS, director of the Narang Eye Care and Laser Centre in Ahmedabad, India, about this technique and the outcomes she has achieved with it.
Mastering Pinhole Pupilloplasty
According to Dr. Narang, patients who specifically suffered from higher-order aberrations and corneal irregularities weren’t happy with any treatment offered to them. “Any intraocular procedure that you do doesn’t work well, whether it’s cataract extraction with IOL implantation, or a keratoconus patient and you do cross-linking, there’s some amount of fibrosis going on and these patients are never happy with their visual outcomes,” she says.
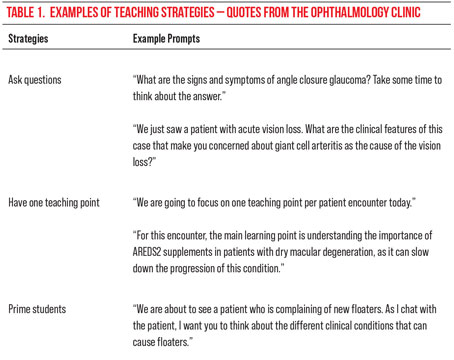
 |
|
Figure 1. Pre- and postop topography of a patient with keratoconus and 10 D of astigmatism who underwent a pinhole pupilloplasty. |
This feedback led Dr. Narang and her colleagues to offer the advantage of small-aperture optics to these patients beginning approximately five years ago. They developed a pinhole pupilloplasty technique that would address patients’ glare and photophobia while achieving adequate image and visual quality.1
Dr. Narang calls pinhole pupilloplasty a “technically demanding procedure.” “A surgeon should be well-versed with doing the basic pupilloplasty procedure before attempting a pinhole pupilloplasty,” she points out.
In a PPP, a surgeon performs a single-pass, four-throw pupilloplasty, an earlier technique developed by Dr. Narang and Amar Agarwal, MD, MS, in which a needle is passed through the edges of an iris defect along the margin of the pupil. The suture end is then passed through the loop with four throws in a modification to the Siepser slip-knot technique, creating a self-retaining and self-locking helical configuration.2
But in the instance of a PPP, Dr. Narang says a modification is made to incorporate more iris tissue into the 10-0 needle “which then is passed through the iris tissue much more centrally so that iris tissue close to the center of pupil is approximated.”1
One prerequisite for a pinhole pupilloplasty is having a good amount of iris tissue, says Dr. Narang. “You can’t do it in cases where the iris tissue is atrophic or if the eye has any other disorders, because what happens in a PPP is you bring down the pupil from all four sides, down to the center, so you need a good amount of tissue everywhere to do that,” she explains.
Determining the size of the pinhole is important. “The pinhole pupil should be centered on the Purkinje image,” Dr. Narang says. “In the preoperative period, you can have the patient lie down on the operating table, and with your surgical microscope light on, ask the patient to look into the light with a coaxial illumination. From there you can just put a mark on the center of the cornea because we have to do this procedure under a surgical block, and when you put a block, many times the eye can rotate. If the eye rotates, your centration won’t be there.”
During surgery, Dr. Narang advises that one side could be much more drawn, while the other side is a bit retracted. “You must remember that this is human tissue, it’s not a mechanical thing,” she says. “What happens is that wherever there’s overlapping of the iris tissue in the Purkinje 1, we use the vitrector probe in the anterior chamber and we remove that iris tissue.”
Patient Outcomes and Other Thoughts
Patients have been pleased with their results, Dr. Narang says, especially since those undergoing a PPP have never seen with any sort of clarity before.
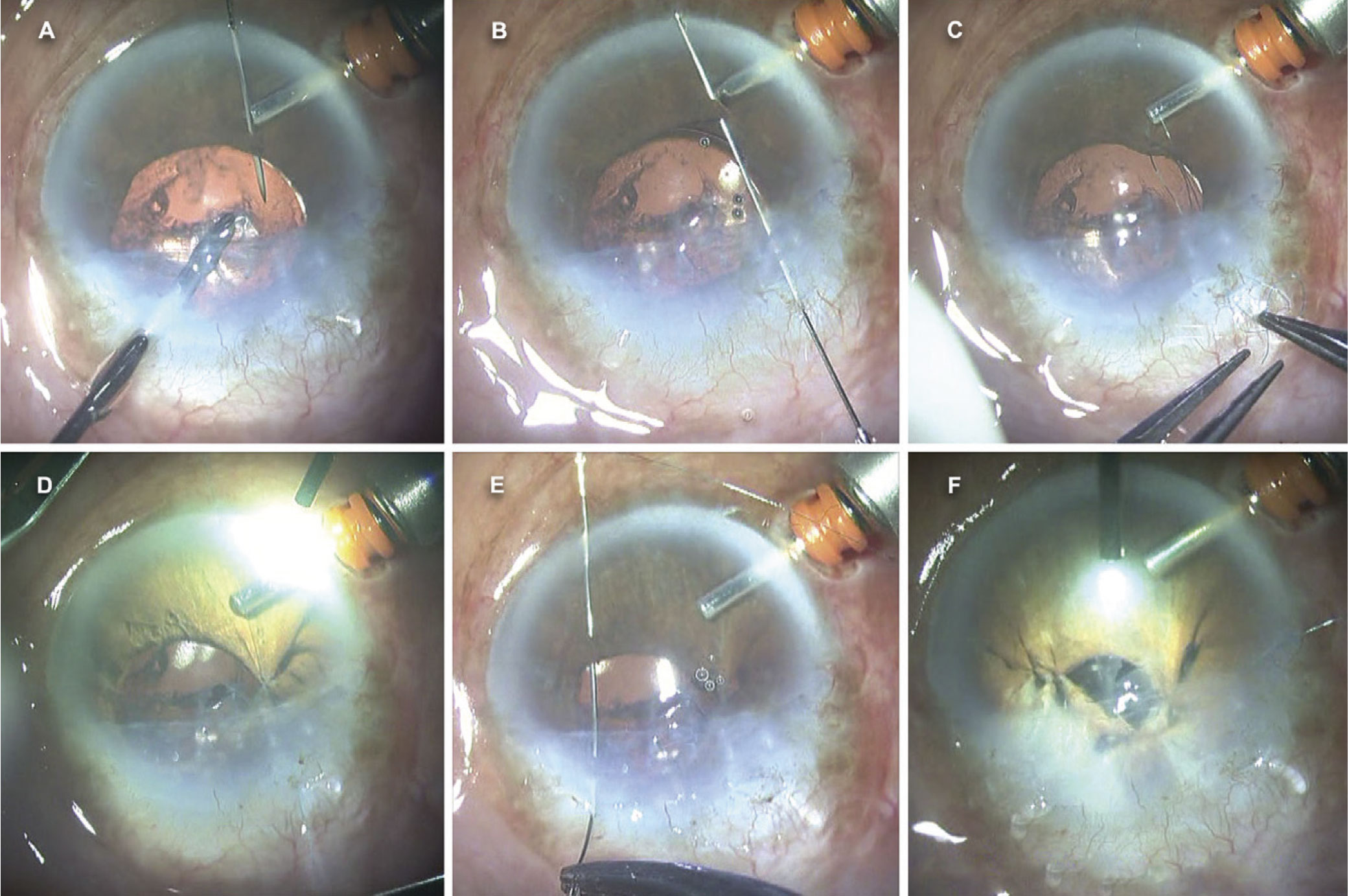
Postop UDVA for one of the five patients in the initial study went from 20/250 to 20/80.1
“We take up cases with higher-order aberrations and do a Pentacam. If their RMS value is more than around 0.35 or 0.4, these are the cases that are specifically chosen for PPP,” she says. “After surgery, it’s not uncommon for patients to start crying. I mean, they’re so happy about it and wonder why this didn’t happen to them sooner.”
From a technical standpoint, Dr. Narang says these patients end up with very good distance, intermediate and near vision thanks to the pinhole providing extended depth of focus. “In our studies we’ve measured a depth of focus that ranges from -2.5 D to +1.5-2 D; there’s a depth of accommodation of about 4 to 5 diopters and that’s phenomenal for these patients.”
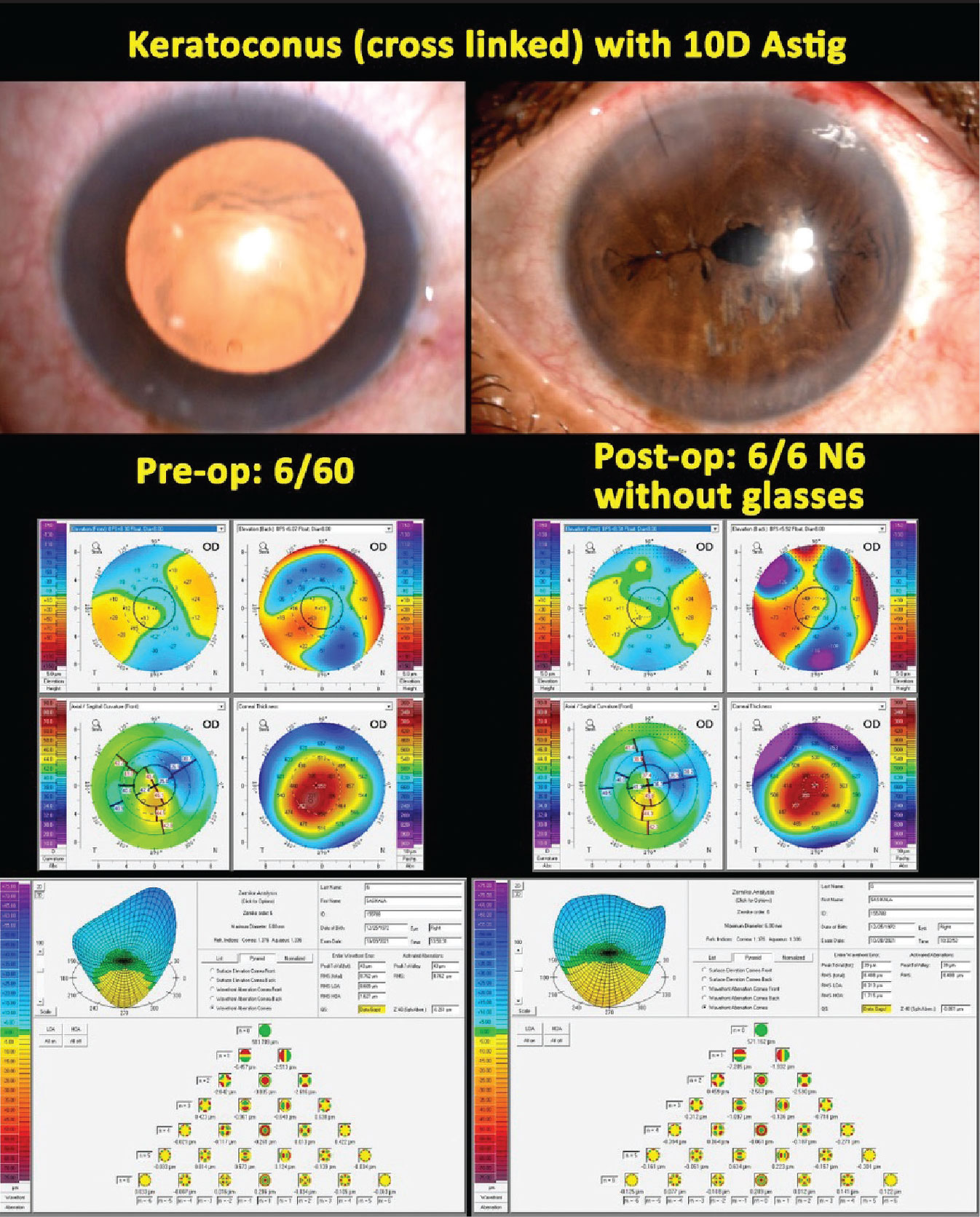
 |
|
Figure 2. A pinhole pupilloplasty performed using a single-pass, four-throw method. |
As Dr. Narang and co-authors travel and present this research, there are some common questions they hear from other surgeons.
“First and foremost, they ask about night vision for these patients, and secondly, they ask how we can see the fundus in the postop period,” she notes.
“Regarding the night vision, I’ve recently finished an analysis of one of our studies wherein we looked at approximately 30 cases and there were only two patients who noted that they do have slight difficulty in the evening or in dim lighting, but they were fine with it because the other benefits outweigh it,” Dr. Narang explains. “These patients are not very demanding because they’ve never seen like this before, unlike refractive surgery patients who are more demanding.”
 |
In terms of viewing the fundus through a PPP, it could pose a challenge. Dr. Narang says that, in certain cases, “a retina surgeon might have to cut down the sutures—it can be removed at any time, you just need micro scissors and you can cut it for any posterior intervention that happens.” Because of this possible difficulty, some retina specialists don’t recommend this technique in patients with or at high risk for peripheral retinal pathology.
Finally, Dr. Narang emphasizes her point about familiarizing yourself with the basic pupilloplasty. “This technique has been adopted worldwide, and I’ve seen even newcomers to the field learning this, so I think it’s not very difficult if anyone wants to venture into it,” she speculates. “Even for those who do have access to the pinhole IOLs, maybe that’s an easier solution, but for a PPP, there’s no additional cost to the patient. Also, for other parts of the world, this is a solution for this specific set of patients.”
Dr. Narang has no disclosures to report.
1. Narang P, Agarwal A, Ashok Kumar D, Agarwal A. Pinhole pupilloplasty: Small-aperture optics for higher-order corneal aberrations. J Cataract Refract Surg 2019;45:5:539-543.
2. Narang P, Agarwal A. Single-pass four-throw technique for pupilloplasty. Eur J Ophthalmol 2017;26;27:4:506-508.