In the past year, there have been numerous reports comparing the results seen with the femtosecond laser to the visual results when a mechanical microkeratome is used. But few of these studies have included a large number of eyes.
In our most recent LASIK study conducted at the
The results show that there are some definitive clinical benefits to using the femtosecond laser for LASIK flap creation, chief among them being a much more reproducible flap.
Our primary interest in performing the study was to look at flap thickness reproducibility and postoperative quality of vision. We also collected data to assess the safety, efficacy and refractive stability following surgery. A secondary outcome of the study was to examine the induction of higher-order aberrations created by the flap itself. To do this, we broke the study group into two with one subset of patients undergoing a step procedure (staged treatment) with a gap of one month between the time the flap was cut and the wavefront-guided laser treatment was performed. The second group underwent a standard wavefront-guided LASIK.
Pre- and postoperative investigations included uncorrected visual acuity and best-corrected visual acuity measurements, manifest and cycloplegic refraction, low-contrast visual acuity, wavefront analysis of higher-order aberrations, corneal pachymetry and intraocular pressure. Patients were seen at one day, one week, one month and three months postop and were also given a psychometric questionnaire preoperatively and again at the three-month postop visit.
Results
When we evaluated the flap reproducibility results, it was clear that the IntraLase laser had the lowest standard deviation of the three keratomes. The range was 94 to 195 µm in the Amadeus group (±18 µm) and 72 to 164 µm (±18 for the 160-µm head and ±24-µm for the 180-µm head) in the Hansatome group. In the IntraLase group, the range was 55 to 126 µm (±16 µm).
Looking at the clinical results, we found that the IntraLase patients fared better at each stage compared to the mechanical microkeratome groups with 68 percent achieving 20/16 on day one postoperatively, compared to 49 percent in the Amadeus and 42 percent and Hansatome groups. Results were similar at one week and the trend continued at one month.
At three months we found that 88 percent of IntraLase eyes were 20/16 or better, compared to 79 percent for Amadeus (p<0.01) and 78 percent for Hansatome (p=0.03). MSE remained significantly better for IntraLase compared to Amadeus (p<0.001) and Hansatome (p=0.001), however the accuracy (% ±0.5 D) was not significantly different. 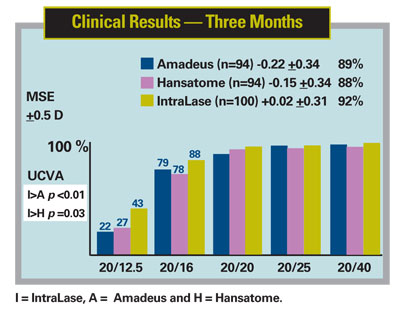
When we compared the three-month UCVA results to the preop BCVA results, the IntraLase group again demonstrated better visual results compared to the mechanical microkeratome groups: 30 percent of the IntraLase group gained one or more lines of vision compared to 13 percent for the Amadeus and 18 percent for the Hansatome. However, there was only a statistically significant difference in the results between the IntraLase and the Amadeus groups (p=0.03). In eyes treated with the femtosecond laser, 85 percent attained UCVA at three months that was as good or better than preoperative BCVA. This is compared to only 70 percent for Amadeus and 69 percent for Hansatome treated eyes.
Quality of Vision
One of the key outcome factors in our study was to assess the quality of vision following LASIK. We measured this in four ways: photopic low-contrast (5 percent) acuity; mesopic low-contrast (25 percent with neutral density filter) acuity; wavefront measurement of higher-order aberrations; and subjective patient self-assessment questionnaires.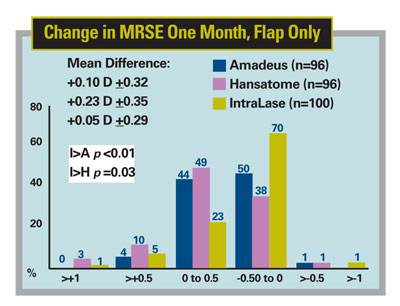
Low-contrast acuity testing at photophobic and mesopic lighting conditions demonstrated that the IntraLase patient groups had superior results compared to the other two groups, particularly at 25-percent contrast acuity. Under mesopic conditions, 42 percent of the IntraLase group gained one or more lines of vision, compared to 17 percent in the Amadeus group (p<0.001) and 36 percent in the Hansatome group (p=0.04). However, we found less of a difference in visual performance at 5-percent (photopic) contrast acuity, with the Hansatome and IntraLase groups posting almost similar results and outperforming the Amadeus group.
Flap Results
When we looked at aberrations induced by creation of the flap itself, we found a trend toward the mechanical keratomes inducing more overall higher-order aberrations, although the differences were not statistically significant. There were no distinct differences in induction of individual aberrations (coma, trefoil or spherical aberration) based solely on the type of keratome used.
When we compared the results between the standard and the staged groups there were no statistical differences in mean MSE at three months postoperatively.
There were also no differences between the staged and standard groups in terms of percentage of patients within ±0.5 D of the intended correction at three months postoperatively.
However, when we looked at the low-contrast visual acuity results, there was a statistically significant difference (p<0.01) between the standard and the staged groups for the Amadeus microkeratome at 5-percent (photopic) testing, in favor of the staged group. We found no significant differences with respect to low-contrast acuity in the treatment groups for Hansatome and IntraLase.
Our study, the largest to date to compare the latest generation of keratomes, provides clear evidence that the IntraLase femtosecond laser performs better than the Amadeus and Hansatome in terms of clinical results (faster visual recovery, more predictable postoperative MRSE and better postoperative UCVA) following wavefront-guided LASIK.
Today there are around 1,000
Dr. Tanzer is the Navy Refractive Surgery Program manager and director of the



