 |
|
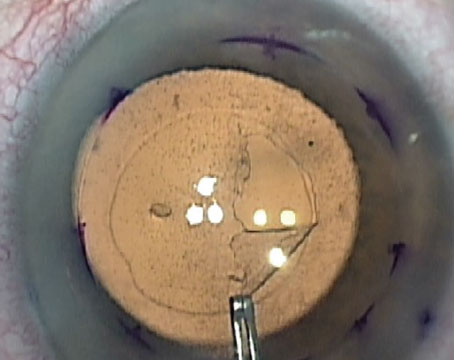
Figure 1. An incorrectly oriented graft. |
Descemet’s membrane endothelial keratoplasty is the gold standard for the surgical treatment of corneal endothelial disorders, offering fast visual recovery, good visual outcomes and low graft rejection rates.1,2 The most frequent postoperative complication of DMEK is partial graft detachment.3 It’s commonly addressed by rebubbling with air or 20% sulfur hexafluoride.
Risk factors for rebubbling may include older recipient age and surgical complications;4,5 however, findings in the literature have been mixed, with some studies reporting that donor characteristics; graft preservation, preparation and cell count; and recipient lens status have no effect with regard to rebubble rates.6,7
Rebubbling can be performed in the operating room or at the slit lamp. I’ve found that rebubbling at the slit lamp is a good alternative approach to the OR that can be incorporated into the clinic day without throwing a wrench in my schedule. If OR access is limited,8 the slit lamp provides flexibility. Here, I’ll describe my technique.
When to Rebubble
Fortunately, DMEK rebubbling rates are low, especially with the primary use of 20% SF6 gas at the time of surgery. I generally have a low threshold for rebubbling if a patient’s vision isn’t recovering as it should. Though minor DMEK detachments will often reattach on their own if given enough time, the patient’s vision may suffer during that period. Bullae or haze may develop if there’s significant corneal edema over a period of time.
I consider rebubbling if more than 30 percent of the graft area is separated from the posterior cornea, especially if it’s in the center of the visual axis; if the patient’s vision isn’t improving as expected; and if there’s curling of the graft and/or progressive separation from the posterior cornea.
Graft Orientation
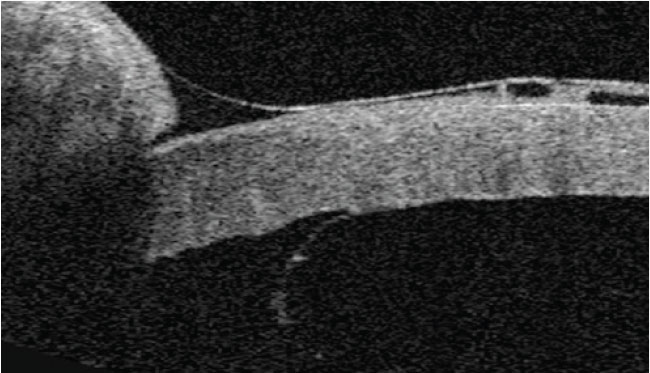
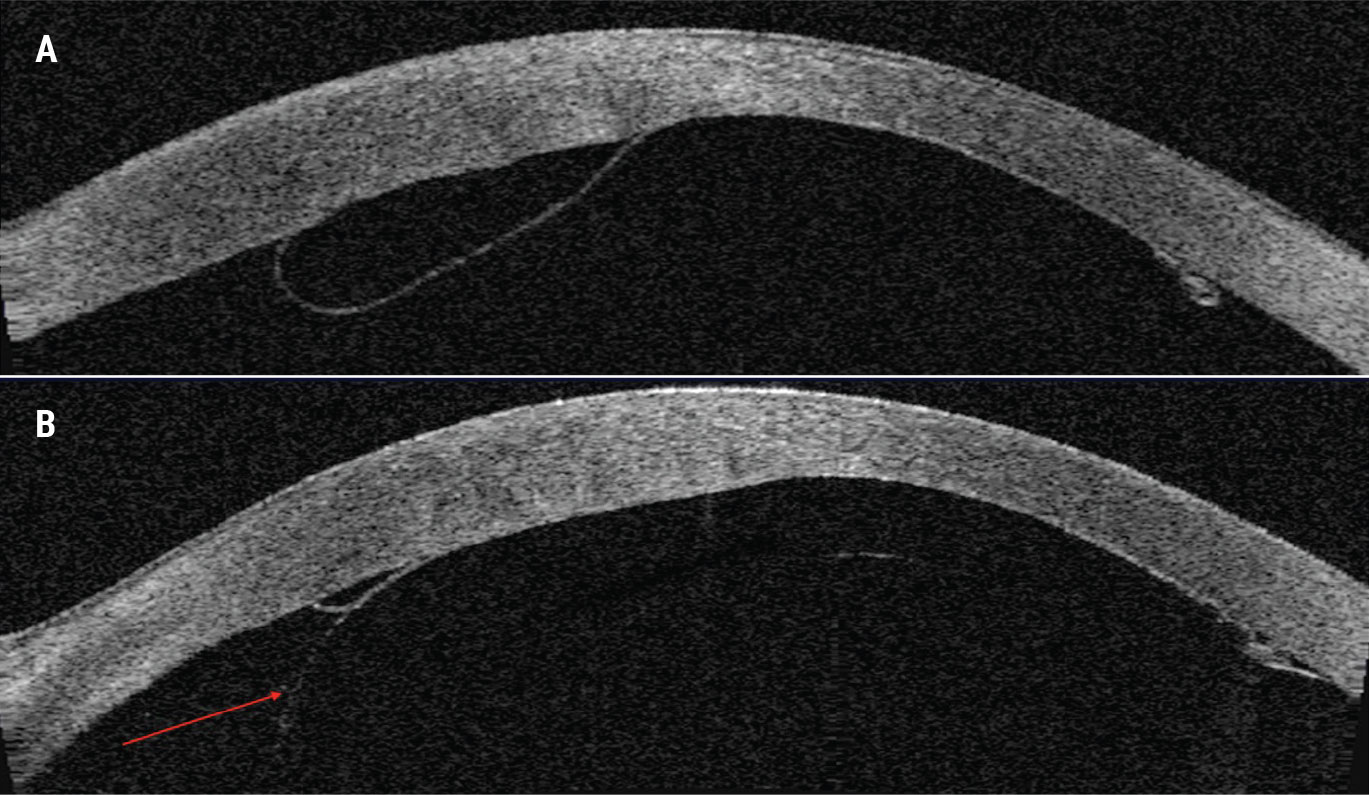
When assessing a detachment, first ensure the graft orientation is correct, with the endothelium down and the orientation marker, such as an “S” or “F” stamp, facing the correct way. Anterior segment optical coherence tomography is helpful for evaluating detached grafts and for determining whether the graft is curving in the proper direction or not (Figure 1). In my practice, we use AS-OCT to find areas of detachment that may otherwise not be fully apparent at the slit lamp (Figures 2-3).
 |
|
Figure 2. A partial detachment in a correctly oriented graft (A). The graft reattaches inferiorly after injection of a gas bubble (red arrow) (B). |
The Setup
 |
|
Figure 3. A diffuse detachment with good central apposition to the posterior stroma (A) but inferior and superior detachment and corresponding thickening of the overlying cornea (B, C). After rebubbling, the graft shows good apposition against the posterior cornea as well as stromal thinning (D). |
Check to make sure the patient is comfortable in the slit lamp, and also be mindful of your own comfort. This is a one-handed technique with some assistance from your second hand, so a comfortable hand position with the slit lamp aperture out of the way and good visualization are key. Having something under your elbow to support may help, though there is some free-floating involved. It’s not the most comfortable procedure by any means but it becomes much more efficient to perform in the clinic than having to go to the operating room. Usual sterile precautions are followed.
The Procedure
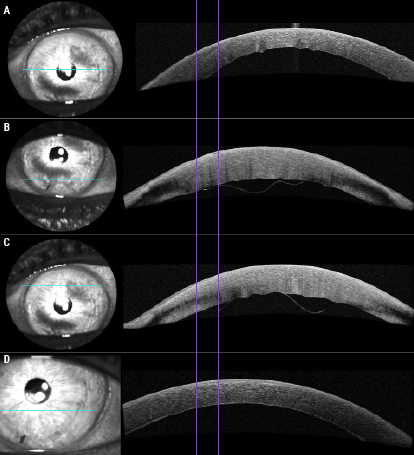
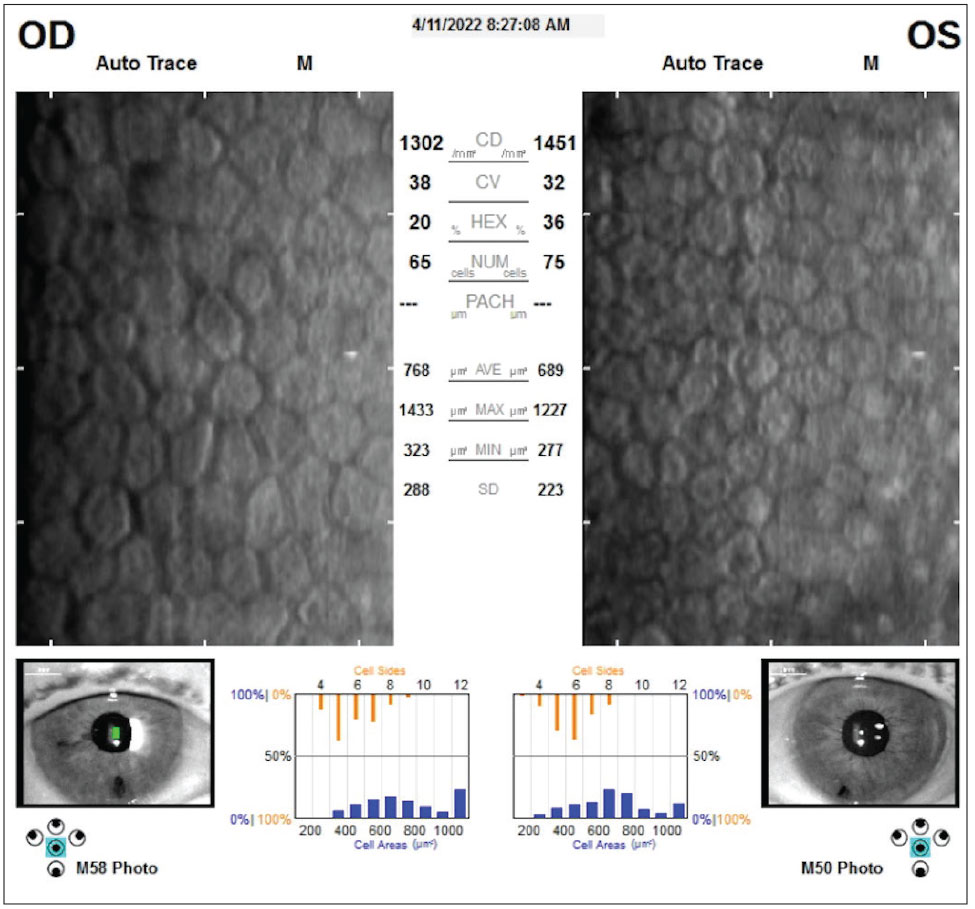
A DMEK rebubbling procedure at the slit lamp takes about three to five minutes. The final outcome in terms of endothelial cell count is often equivalent to that of eyes that didn’t require rebubbling (Figure 4). Here’s my approach:
Place the topical anesthesia and then place the speculum. To ensure I’ve cleaned adequately, I like to do a limited Betadine prep and some topical antibiotics within the eye. Then, I prepare my cannulas: one with air and one with BSS.
One key step is releasing some aqueous from the anterior chamber by gently depressing the lip of your paracentesis wound with the 30g cannula. You want to create space to place your air fill. Often, surgeons will inject without releasing any fluid from the eye, and that causes the IOP to spike.
Insert the cannula. When you insert the cannula after releasing some aqueous, ensure the cannula is anterior to the iris and posterior to the graft. This may sound obvious, but sometimes when the visualization is poor it can be hard to determine where the cannula is in relation to the DMEK graft. If you’re not sure, don’t inject. Check that the patient is looking straight ahead.
 |
|
Figure 4. Comparison of the right and left eyes of a patient who underwent bilateral DMEK. Only the left eye required rebubbling. Specular microscopy shows little to no difference between the appearance of each eye’s endothelial cells. |
Inject air behind the graft until the bubble fills the chamber. I usually inject air from below, even if I have a superior paracentesis, for two reasons: one, it’s ergonomically easier, and two, there’s less air loss as you’re injecting. If you go superiorly, sometimes the injected air comes right back out. If you go from below, the air tends to stay in the eye better. If necessary, release some pressure from an existing paracentesis superiorly. (If you don’t have a 30-gauge cannula, a 30-gauge needle will work. Create a fresh incision using the needle, go inferiorly and inject through the needle.)
When you inject, inject slowly. Very commonly surgeons will inject with a quick burst of air. When the patient isn’t anesthetized with a block or is on the table or in a setup where they could move, that quick influx of air may make the patient jump. Aim for a nice, easy fill over a few seconds. You can generally see the graft reattach to the posterior cornea as you do that.
Once you’re done, confirm the patient’s vision. Rebubbling can lead to very high pressures in the eye. If the pressure goes up significantly it can overcome the circulation in the back of the eye. Be sure the patient can see at least hand motion.
Finally, place the topical antibiotic. I usually leave patients supine for 10 to 15 minutes to give the graft time to adhere and then check the patients’ pressures.
In conclusion, if you do DMEK, knowing how to rebubble is key. Performing this procedure for partial graft detachments at the slit lamp is a convenient alternative to the OR, and one that’s often easier on the patient.
Dr. Garg is a professor of ophthalmology, the vice chair of clinical ophthalmology and medical director of the Gavin Herbert Eye Institute, University of California, Irvine. He’s a consultant to Allergan, Avellino, CorneaGen, Dompé, Glaukos, Johnson & Johnson Vision, Kala, LensGen, New World Medical, Novartis, Oyster Point, Sight Sciences, Tarsus, Trefoil Therapeutics, Visus and Zeiss.
1. Tourtas T, Laaser K, Bachmann BO, eta l. Descemet membrane endothelial keratoplasty versus Descemet membrane stripping automated endothelial keratoplasty. Am J Ophthalmol 2012;153:6:1082-1090.
2. Singh A, Zarei-Ghanavati M, Avadhanam V, Liu C. Systemic review and meta-analysis of clinical outcomes of Descemet membrane endothelial keratoplasty versus Descemet stripping endothelial keratoplasty/Descemet stripping automated endothelial keratoplasty. Cornea 2017;36:11:1437-1443.
3. Deng SX, Lee WB, Hammersmith KM, et al. Descemet membrane endothelial keratoplasty: Safety and outcomes: A report by the American Academy of Ophthalmology. Ophthalmology 2018;125;2:295-310.
4. Dunker S, Winkens J, van den Biggelaar F, et al. Rebubbling and graft failure in Descemet membrane endothelial keratoplasty: A prospective Dutch registry study. Br J Ophthalmol 2023;107:1:17-23.
5. Achiron A, Nahum Y, Tiosano A, et al. Descemet membrane endothelial keratoplasty outcomes between young and old graft recipients. Curr Eye Res 2021;46:10:1460-1466.
6. Godin MR, Boehlke CS, Kim T, Gupta PK. Influence of lens status on outcomes of Descemet membrane endothelial keratoplasty. Cornea 2019;38:4:409-412.
7. Straiko MD, Bauer AJ, Straiko MMW, et al. Donor DMEK tissue characteristics: Association with rebubble rate and 6-month endothelial cell loss. Cornea 2020;39:10:1267-1273.
8. Franka M, Mistry M, Moustafa M, eta l. Rebubbling of detached Descemet membrane endothelial grafts at the slit lamp with 50% air fill after PI-less DMEK during COVID-19 era. Eur J Ophthalmol 2021;31:3:1413-1416.