In the 1870s, Leber proposed a model of IOP regulation that most ophthalmologists today are familiar with, one in which a passive flow-filter mechanism governs aqueous outflow. The model posits an obstruction in the juxtacanalicular space caused by extracellular matrix, which acts as a filter to impede fluid flow. Ultimately, fluid passes through endothelium via pores with the extracellular matrix regulating the filter’s function. However, this theory was formulated based on observations from enucleated eyes lacking normal intraocular pressure and normal ciliary body tone, and preserved ex vivo with fixative—a stark departure from physiological conditions in living organisms.
Our understanding of aqueous outflow today takes a different shape, reminiscent of the lymphatics mechanism proposed by Leber’s contemporary, Schwalbe. The model presented here is a pulsatile flow motion model based on frameworks that have evolved over the last century since 1942, when dynamic pulsatile flow out of the anterior chamber and into the episcleral veins was first demonstrated. Here, I’ll provide an overview of this system and its implications for clinical practice and surgical management.
Pulsatile Flow Motion Model
The trabecular meshwork along with the inner wall endothelium and Schlemm’s canal are in constant motion, dependent on pressure gradients. Fluid is forced into this valve system, i.e., the Schlemm’s canal inlet valve, which then pumps fluid into the Schlemm’s canal. The fluid is then driven out of the canal into collector channels and ultimately into the episcleral veins.
The ocular pulse and intraocular pressure undergo oscillatory changes, typically fluctuating by about 3 mm on average with each pulse wave. At the slit lamp, you can watch the mires oscillate when performing tonometry. These oscillations reflect the pressure gradient changes occurring within the anterior chamber. That pressure is transmitted to the trabecular meshwork, which undergoes dynamic motion in response to the intraocular pressure changes.
The underlying power behind this process is the heart. The pressure generated by the heart drives the trabecular meshwork, causing it to move outward. The trabecular meshwork’s elastic properties allow it to stretch, store elastic energy and then recoil when pressure decreases, releasing its stored energy. It’s a highly dynamic system. The trabecular meshwork responds in a similar manner to the heart undergoing oscillatory compression of a chamber, driving fluid.
 |
Figure 1. Homeostasis in the dynamic model.10 The central vertical panel (B, E, H) shows the TM position in SC at homeostatic IOP, while the left panel (A, D, G) is below-optimal IOP, reducing aqueous flow, and the right panel (C, F, I) is above IOP setpoint, increasing aqueous flow. Pulsatile flow oscillates around homeostatic TM position. TM, trabecular meshwork; EW, external wall; SC, Schlemm’s canal; SCE, SC inner wall endothelium; EVP, episcleral vein pressure; SIV, SC inlet valve; CCO, collector channel ostia; SOV, Schlemm’s canal outlet valve; JCS, juxtacanalicular space; ISC, radial intrascleral channel; CDSP, circumferential deep scleral plexus, aka: outer canal, circumferential vascular channel. (Used with permission of the authors under Creative Commons Attribution (CC BY) license (creativecommons.org/licenses/by/4.0).) |
Valved Distal System
Before more recent advances in OCT imaging, we’ve known that that the trabecular meshwork is the wall of Schlemm’s canal, and that Schlemm’s canal is a chamber whose volume changes with intraocular pressure. Aqueous-containing endothelial-lined conduits arise from the inner wall of the canal. These conduits have a tubular shape. They cross the canal and attach to the external wall.
Over the last 12 years, in my lab and in Dr. Ruikang K. Wang’s lab, we’ve demonstrated that a Schlemm’s canal inlet valve apparatus is functionally present using various techniques, including dissecting microscopy, bright-field microscopy, bright-field blockface, scanning electron microscropy, confocal native fluorescence, Nomarski DIC, nanoparticle tracers and high-definition OCT, both static and phase-based (See Further Reading).
Here’s a rundown of the system (Figure 1):
• Schlemm’s canal inlet and outlet valves. Schlemm’s canal has both inlet valves and outlet valves, which can be visualized at the dissecting microscope. The inlet valves are flow pathways to Schlemm’s canal that also connect the trabecular meshwork to the collector channel valves. Inlet valves attach to the outlet valves at collector channel entrances. There are approximately 70 inlet valves around the circumference of the canal. These require canal dilation to be seen.
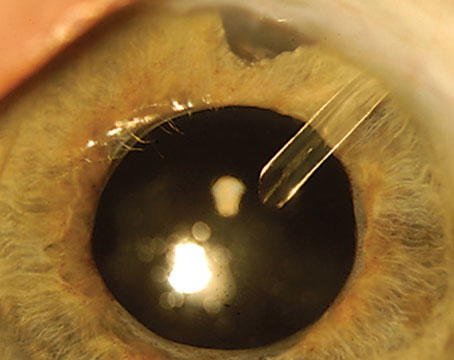
Inlet valves permit aqueous flow and prevent blood reflux. Schlemm’s canal inlet valve structure has been documented by light, scanning and transmission electron microscopy, and microsphere and red blood cell tracer studies have documented inlet valves’ function as conduits. When we unroof Schlemm’s canal, the inlet valves break and discharge aqueous. During gonioscopy, inlet valves discharge oscillating waves of aqueous into the canal.
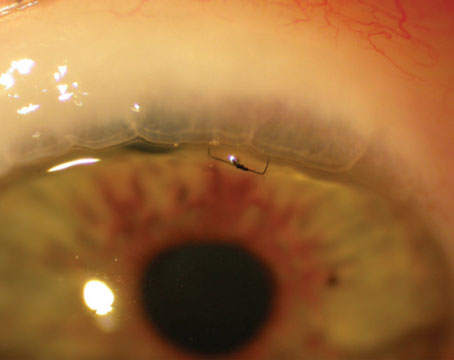
• Septa. Between Schlemm’s canal and the outer canal lie the septa. Still images of the dynamic motion of a septum controlling distal flow are pictured in Figure 2.
 |
| Figure 2. Still images of a septum in dynamic motion. Septa are located between Schlemm’s canal and the outer canal. They control distal flow. |
• Collector channels. The collector channels leave the eye in a remarkably regular fashion, all in the same plane, exiting from Schlemm’s canal, then entering a circumferential set of vascular channels, also known as the circumferentially oriented deep scleral plexus or the outer canal, before reaching the surface episcleral veins. Basically, the fluid must pass through these circumferential vascular channels before moving into the radial channels and reaching the surface.
Using ex vivo high-resolution OCT, we’ve observed that the collector channel valve entrances have collagen flaps attached only at one end. These hinged flaps undergo pressure-dependent changes in position, which allow the hinged flaps to open and close the collector channels, acting also as Schlemm’s canal outlet valves.
• Circumferentially oriented deep scleral plexus. These channels are adjacent to Schlemm’s canal, separated from it by thin septa. They move by pressure-dependent mechanisms, opening and closing like a second pressure-dependent chamber.
Real-time imaging of tissue motion using ex vivo high-resolution OCT shows that the trabecular meshwork beams, Schlemm’s canal inlet and outlet valves, and the circumferentially oriented deep scleral plexus all undergo rapid cyclic pulsatile movement. The motion of these structures’ volume changes is all synchronous, made possible by cellular attachments between the structures. The amplitude and motion velocity of the pulsatile movement can account for all of the aqueous outflow.
Interestingly, an independent embryogenesis study1 of 61 eyes preserved with clarification and microvascular casting, reported five gestational intervals, with collector channels developing at six weeks of gestation, sprouting from Schlemm’s canal. These developed into circumferential channels, joining one another to create the circumferential vascular plexus. This ultimately joins with the episcleral and intrascleral vessels to form a complete system.
Under Pressure
As glaucoma worsens, fluid movement into and out of the canal slows. This indicates a change in the pulsatile motion. You can see this in the clinic by pressing on the gonioprism to apply light pressure to the episcleral veins. In healthy patients, the pressure on the episcleral veins drives blood rapidly into Schlemm’s canal and fills it completely. As pressure is released, the blood escapes rapidly, indicating that the trabecular meshwork is capable of rapid motion in response to pressure changes.
Homeostatic responses in the trabecular meshwork are well documented and can be observed in the clinic with tests such as the water drinking test, which involves having the patient drink a quart of water very quickly, driving up the fluid pressure within the eye. This rise in pressure occurs due to osmotic changes that draw fluid from the bloodstream into the eye to maintain osmotic balance, ultimately elevating intraocular pressure.
The example in Figure 3 shows video screen captures of visible pulsatile flow at an intraocular pressure of 10 mmHg. As the pressure gradually rises during the water drinking test, new regions begin to exhibit pulsations, indicating an increase in the stroke volume of pulsatile flow. At 12 mmHg, the pulsatile flow is notably larger, driving fluid farther along the vein and into the episcleral veins on the surface. Even more pronounced pulsatile behavior is seen with each pulse wave at 14 mmHg. The larger stroke volume of aqueous drives fluid into a more distal region, entering a larger episcleral vein.
 |
| Figure 3. The water drinking test provides an opportunity to observe pulsatile flow in the clinic. (IOP: 10 mmHg, top; 12 mmHg, middle; 14 mmHg, bottom.) As the intraocular pressure rises following rapid consumption of a quart of water, the ocular pulse increases along with pulse pressure and oscillatory flow. This leads to an increased volume of aqueous pumped out of the eye with each cardiac pulse wave, ultimately lowering intraocular pressure to its pre-water drinking test level. |
This provides clear evidence of pulsatile aqueous outflow, which serves as a regulatory mechanism. When intraocular pressure rises, so does the ocular pulse, along with pulse pressure and oscillatory flow. This leads to an increased volume of aqueous pumped out of the eye with each cardiac pulse wave, subsequently lowering intraocular pressure and ultimately returning it to its pre-water drinking test level.
This homeostatic return of flow to its normal level also occurs with medications such as miotics, adrenergics and prostaglandins such as latanoprost and travoprost. When the patient is at a homeostatic setpoint for pressure, upon initiating medication (typically within five minutes for adrenergics and 15 minutes for prostaglandins and miotics) the stroke volume of aqueous starts to rise and continues to rise for about an hour or so. As the stroke volume rises, the pressure begins to drop as aqueous is pumped out of the eye. Finally, the pressure moves to a lower homeostatic setpoint.
The eye is one of many vascular loops of the heart, along with the arterial, venous and lymphatic systems. In these systems, the principle remains the same: Return is regulated by valves and a pulsatile mechanism. With each systolic pulse wave, aqueous is discharged from the intrascleral channel into the episcleral vein, driving the episcleral venous blood backwards. As that wave progresses, it drives fluid along the aqueous vein, discharging farther.
Thanks to in vivo phase-sensitive-OCT developed by Dr. Wang’s Imaging Lab, we’re now able to see the response to intraocular pressure gradient changes in patients in real time. Compared to the limited sensitivity of spectral domain-OCT systems using a 810-nm wavelength, a 1,310-nm PhS-OCT system resolves motion of approximately 20 nm and quantifies trabecular meshwork velocity and displacement. Figure 4 shows video screen captures of a PhS-OCT heat map of the trabecular meshwork’s outward motion in red and recoil in blue.
 |
| Figure 4. Phase-sensitive OCT enables in vivo imaging of dynamic tissue motion. These heat maps of the trabecular meshwork show outward motion in red and recoil in blue. |
TM-Ciliary Muscle Complex
Pinpointing the causes of glaucoma remains challenging. We hypothesize at least two fundamental pathways: 1) The ciliary body moves forward with age, but pathologically so in glaucoma; and 2) the trabecular meshwork stiffens with age, like other collagen tissues of the body. This stiffening may be accentuated in glaucoma, however. Taken together, these changes in stiffness and elastance of the trabecular meshwork-ciliary muscle complex may underlie intraocular pressure abnormalities.
The ciliary muscle maintains uniform tension throughout the outflow system, from the trabecular meshwork to the septa and collector channels. When the ciliary muscle contracts, it increases tension on the scleral spur and trabecular meshwork lamellae, causing the trabecular meshwork to move away from the external wall of Schlemm’s canal. This increase in stress on the trabecular meshwork changes its elastance and allows it to distend and recoil in a homeostatic range. Loss of ciliary muscle tension and increased intraocular pressure result in Schlemm’s canal collapse.
The trabecular meshwork possesses mechanisms to maintain homeostasis and repair tissue. Like the aorta, which is fairly analogous to this system, elastin provides recoil while collagen maintains stability and resistance. As we age, particularly between ages 40 and 70, elastin fragments and is replaced by collagen. This age-related process leads to tissue stiffening and likely affects the trabecular meshwork lamellae similarly, impeding its ability to move back and forth. The aorta undergoes a 50-percent enlargement with age. As the trabecular meshwork stiffens, it distends into Schlemm’s canal, narrowing its lumen. This change may contribute to Schlemm’s canal wall apposition and closure.
Shear stress issues with age are a fundamental problem in this area, much like in the cardiovascular system. The aorta experiences approximately 31 million distension and recoil cycles annually. So does the trabecular meshwork. Basically, the lumen of Schlemm’s canal is constantly oscillating, also around 31 million times a year, exposing it to significant stresses. As we age, every cardiac pulse wave is driven at a much higher speed because it’s a stiffer system.
The endothelial walls of these vascular pathways are constantly sensing and adjusting shape in response to pressure gradient changes. The vasculature is highly dependent on maintaining a tightly regulated flow pattern, which regulates the dimensions of the vessel walls. Disruption of this flow pattern, such as with the removal of a normal regulatory system (e.g., the trabecular meshwork and Schlemm’s canal inlet valves), results in exposure to abnormal shear stresses, which over time leads to cytokine release, fibrotic changes and involution or closure of the vessel walls.
A Role in Surgical Planning
Studying pulsatile flow patterns in the clinic to check for potential outflow structure damage may assist with surgical planning when it comes to identifying MIGS placement locations. While pulsatile flow from the aqueous to episcleral veins is visible at the slit lamp, this approach (i.e., the water drinking test) is time consuming and of limited clinical use. On the other hand, hemoglobin imaging, a new technique that can be employed at the slit lamp in the clinic, offers noninvasive, real-time quantification of flow rate by differentiating aqueous and episcleral venous blood.2-5
Alex S. Huang, MD, PhD, and colleagues reported that injecting a fluid bolus into the anterior chamber during MIGS surgery will displace blood in the episcleral veins, resulting in a pulsatile episcleral vein bolus and regional blanching that indicates the openness of structural pathways from the anterior chamber to the aqueous and episcleral veins. Another approach studied in primates and humans involves injecting dyes into the anterior chamber of Schlemm’s canal to visualize pulsatile behavior. These approaches may assist with MIGS placement.6-8
It’s important to note that MIGS don’t work by a physiologic mechanism since they disrupt the outflow system structures. Nevertheless, they’re an important component in the surgical management of glaucoma and reduce patients’ medication burden as well as the need for trabeculectomies.
Restoring Normal Pump Function
Cataract surgery is one procedure that restores normal pump function and avoids structural damage to the outflow system, potentially by improving scleral spur traction. A 2010 paper9 by Susan A. Strenk, MD, and colleagues suggests that cataract surgery’s intraocular pressure reduction mechanism is related to anterior chamber deepening and the residual lens capsule positioned posterior to Schlemm’s canal. This alignment causes the trabecular meshwork and scleral spur attachments to rotate backward in response to ciliary muscle tension, increasing tension on the trabecular meshwork and enlarging Schlemm’s canal.
As long as there’s ciliary muscle tone, pilocarpine temporarily restores pulsatile flow in glaucoma by increasing ciliary muscle tension. This miotic response may explain some of the effects of transscleral micropulse laser, which induces heat, tightening the ciliary muscle and opening the proximal and distal outflow pathways. The effects of laser trabeculoplasty such as SLT and ALT also induce heat, resulting in collagen shrinkage and potentially increasing trabecular meshwork tension to restore pulsatile outflow.
In summary, the aqueous outflow system is a vascular loop of the circulatory system, where pulsatile tissue motion, chambers and valves work together to control the stroke volume of aqueous discharge and regulate IOP.10 As a system with collagen- and elastin-containing tissues, its motility decreases with age. It’s believed this stiffness occurs pathologically in the setting of glaucoma. Further research on the restoration of normal pump function may hold clues to developing future glaucoma procedures and therapeutics.
Dr. Johnstone is a clinical professor of ophthalmology at the University of Washington School of Medicine in Seattle. He leads the Johnstone Lab, which studies regulation of aqueous outflow in glaucomas through studies of tissue biomechanics and related morphology. He is a consultant for Alcon and Elios Vision.
Further Reading
1. Johnstone MA, Grant WG. Pressure-dependent changes in structures of the aqueous outflow system of human and monkey eyes. Am J Ophthalmol 1973;75:365-383.
2. Johnstone MA, The aqueous outflow system as a mechanical pump: evidence from examination of tissue and aqueous movement in human and non-human primates. J Glaucoma 2004;13:421-438.
3. Johnstone M, Martin E, Jamil A. Pulsatile flow into the aqueous veins: manifestations in normal and glaucomatous eyes. Exp Eye Res 2011;92:318-327.
4. Li P, Reif R, Zhi Z, Martin E, Shen TT, Johnstone M, Wang RK. Phase-sensitive optical coherence tomography characterization of pulse-induced trabecular meshwork displacement in ex vivo non-human primate eyes. J Biomed Opt 2012;17:076026.
5. Li P, Shen TT, Johnstone M, Wang RK. Pulsatile motion of the trabecular meshwork in healthy human subjects quantified by phase-sensitive optical coherence tomography. Biomed Opt Express 2013;4:2051-2065.
6. Hariri S, Johnstone M, Jiang Y, Padilla S, Zhou Z, Reif R, Wang RK. Platform to investigate aqueous outflow system structure and pressure-dependent motion using high-resolution spectral domain optical coherence tomography. J Biomed Opt 2014;19:106013.
7. Xin C, Wang RK, Song S, Shen T, Wen J, Martin E, Jiang Y, Padilla S, Johnstone M. Aqueous outflow regulation: Optical coherence tomography implicates pressure-dependent tissue motion. Exp Eye Res 2016.
8. Xin C, Johnstone M, Wang N, Wang RK. OCT study of mechanical properties associated with rrabecular meshwork and collector channel motion in human eyes. PLoS One 2016;11:e0162048.
9. Xin C, Song S, Johnstone M, Wang N, Wang RK. Quantification of pulse-dependent trabecular meshwork motion in normal humans using phase-sensitive OCT. Invest Ophthalmol Vis Sci 2018;59:3675-3.
10. Poley BJ, Lindstrom RL, Samuelson TW, Schulze R. Intraocular pressure reduction after phacoemulsification with intraocular lens implantation in glaucomatous and non-glaucomatous eyes: Evaluation of a causal relationship between the natural lens and open-angle glaucoma. J Cataract Refract Surg 2009;35:1946-1955.
11. Johnstone M, et al. Micropulse laser effect assessment by high-resolution OCT imaging. IOVS S1-2825, 201.
12. Johnstone M, Xin C, Acott T et al. Valve-like outflow system behavior with motion slowing in glaucoma eyes: Findings using a minimally invasive glaucoma surgery-MIGS-like platform and optical coherence tomography imaging. Front Med (Lausanne) 2022;9:815866.
13. Johnstone M, Xin C, Tan J, Martin E, Wen J, Wang RK. Aqueous outflow regulation–21st century concepts. Prog Retin Eye Res 2021;83:100917.
14. Johnstone M, Xin C, Martin E and Wang R. Trabecular meshwork movement controls distal valves and chambers: New glaucoma medical and surgical targets. J Clin Med 2023;12:6599.
1. Ramírez JM, Ramírez AI, Salazar JJ, Rojas B, De Hoz R, Triviño A. Schlemm’s canal and the collector channels at different developmental stages in the human eye. Cells Tissues Organs 2004;178:180-185.
2. Khatib TZ, Meyer PAR, Lusthaus J, et al. Hemoglobin video imaging provides novel in vivo high-resolution imaging and quantificationof human aqueous outflow in patients with glaucoma. Ophtahlmol Glaucoma 2019;2:327-335.
3. Lusthaus JA, Khatib TZ, Meyer PAR, et al. Aqueous outflow imaging techniques and what they tell us about intraocular pressure regulation. Eye 2020;35:216-235.
4. Lusthaus JA, Meyer PAR, Khatib TZ, et al. The effects of trabecular bypass surgery on conventional aqueous outflow, visualized by hemoglobin video imaging. J Glaucoma 2020;29:656-665.
5. Lusthaus JA, Meyer PAR, McClusky PJ, et al. Hemoglobin video imaging detects differences in aqueous outflow between eyes with and without glaucoma during the water drinking test. J Glaucoma 2021;31:511-522.
6. Huang AS, Camp A, Xu BY, Penteado RC, Weinreb RN. Aqueous angiography: Aqueous humor outflow imaging in live human subjects. Ophthalmol 2017;124:1249-1251.
7. Huang AS, Li M, Yang D, Wang H, Wang N, Weibreb RN. Aqueous angiography in living nonhuman primates shows segmental, pulsatile, and dynamic angiographic aqueous humor outflow. Ophthalmology 2017;124:793-803.
8. Huang AS, Saraswathy S, Dastiridou A, Begian A, Mohindroo C, Tan JCH, Francis BA, Hinton DR, Weinreb RN. Aqueous angiography-mediated guidance of trabecular bypass improves angiographic outflow in human enucleated eyes. Invest Ophthalmol Vis Sci 2016;57:4558-4565.
9. Strenk SA, Strenk LM, Guo S. Magnetic resonance imaging of the anteroposterior position and thickness of the aging, accommodating, phakic, and pseudophakic ciliary muscle. J Cataract Refract Surg 2010;36:235-241.
10. Johnstone M, Xin C, Martin E and Wang R. Trabecular meshwork movement controls distal valves and chambers: New glaucoma medical and surgical targets. J Clin Med 2023;12:6599.