Allergies occur in an estimated 20 percent of the population, and one-third of allergy sufferers develop ocular symptoms. With more than 35 million contact lens wearers in the United States, a significant number of our patients may be suffering from ocular allergies. These patients typically must remove their lenses during periods of ocular symptoms. But with careful evaluation, adjustments in lens materials and care solutions, along with topical therapy, we may be able to keep our patients in contact lenses safely and comfortably.
Type I, Type IV
Reviewing the pathophysiology of ocular allergy, we find that it's most commonly associated with Type-I and Type-IV hypersensitivity reactions. In Type-I reactions, allergens come into direct contact with the ocular surface and bind with immunoglobulin E (IgE) on the conjunctival mast cells. This leads to mast-cell degranulation, with release of mediators such as histamine, prostaglandins and leukotrienes. These mediators cause the common allergic conjunctivitis symptoms of itching, redness, tearing and chemosis. Seasonal allergic conjunctivitis (SAC) is the most common form of ocular surface Type-I reaction. Type-IV hypersensitivity reactions can also occur in our contact lens patients. Activation of the complement system occurs when the allergen binds with circulating antibodies. This type of reaction is usually related to topical medications and preservatives such as thimerasol.
 |
| Acute allergic conjunctivitis develops rapidly and resolves soon after contact with the allergen ends. |
SAC usually affects our patients for two or three months in the spring and then again in late summer and early fall. Pollens and grass antigens are usually responsible for springtime allergies, while ragweed allergies occur in the late summer. Allergens and time of year will vary based on geographic location. Perennial allergic conjunctivitis can also cause problems for our contact lens wearers. Animal dander, house dust and molds are common perennial antigens. Symptoms can occur year round, and although they're typically milder than those of seasonal allergic conjunctivitis, they can worsen occasionally and require a fresh look at treatment.
While the scope of this article does not allow a complete review of all types of allergic conjunctivitis, these should be in your differential diagnosis: atopic keratoconjunctivitis, vernal keratoconjunctivitis and giant papillary conjunctivitis.
Allergy or Other?
At times, allergic conjunctivitis in our contact lens wearers may be difficult to distinguish from dry eye or other contact lens-related irritations. A thorough history is important to help identify the allergic patient. Include a review of the patient's systemic and ocular allergy history, medications and contact lens history. Systemic medications including antihistamine may be causing dryness, and self treatment with over-the-counter allergy drops may cause irritation. The preservatives can build up in the contact lens matrix, which can cause superficial punctate keratitis, redness and stinging. Ask patients if there is a seasonal relationship to their symptoms, or if they have noted specific exposures to allergens, such as grass while mowing the lawn, that may trigger an allergic reaction. Itching is the most common symptom associated with allergies, along with redness, burning, tearing and swelling.
Examination
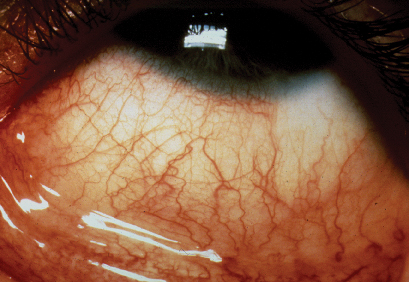
When evaluating the patient, start with an external examination. With severe allergies, periocular edema may be seen. Medication-induced allergies may include an allergic dermatitis with lichenification, erythema and flaking of the lids. At the slit lamp, be sure to evaluate both the bulbar and palpebral conjunctiva for injection, chemosis, follicles, and papillae. SAC and PAC are usually associated with a watery discharge, but a rope-like mucoid discharge may be seen with some allergic conjunctivitis.
What to Consider
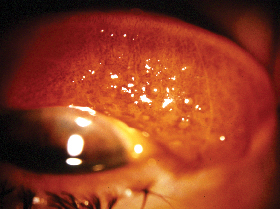
The incidence of giant papillary conjunctivitis is higher and the symptoms appear to be more severe with soft lenses than with rigid lenses.
Patients suffering from allergies do not automatically have to discontinue contact lens wear. There are options available that can help us reduce ocular surface irritation and maintain successful lens wear. So how do we manage these patients? Ideally, if we could identify and then avoid or eliminate the offending allergens, we could solve the problem. However, this is not usually possible. Alternative approaches include appropriate topical therapy, careful adjustments in lens wear, and new materials and lens care solutions.
Lens Material Options
Rigid gas permeable lenses were the only contact lens option for these patients before daily disposable lenses became available. RGP lenses have a lower water content and absorb less allergen in the lens matrix than soft lenses. However, some patients cannot wear or choose not to wear RGP lenses.
For these allergy sufferers, a lens that reduces coating and protein deposition is best. The more frequently a lens can be replaced, therefore, the less the accumulation of allergens. Daily disposables are an excellent option. One-day lenses include Vistakon's 1-Day Acuvue, CibaVision's Focus Dailies and Bausch & Lomb's SofLens one-day. Options for low astigmats and presbyopes are also available with CibaVision's one-day torics and progressives, as well as Vistakon's Acuvue line.
CooperVision's Proclear Compatibles have allowed successful lens wear for many lens-intolerant patients bothered by dry eye. The omafilcon A material doesn't attract lipids and proteins, and the lenses contain phosphorylcholine, a substance that makes the lens biocompatible, increasing patient comfort. These lenses come in monthly replacement for most lens wearers. Hydrogel Vision Corp.'s Extreme H2O lens, made of hioxifilcon A, is another option for dry-eye symptoms. This is a two-week lens that maintains its hydration well, improving lens tolerance.
Silicone hydrogel lenses used in a daily-wear regimen may also help patients with allergies and associated dry eye. Vistakon's new Acuvue Advance lens contains a substance called hydraclear, an internal wetting agent, that helps resist lens dehydration. This lens has three times the oxygen transmission of a traditional hydrogel lens.
Care Products
Review the various lens-care products with allergy patients, since these patients tend to be more sensitive to chemicals in solutions and preservatives. While no-rub products are convenient, it's best to rub the contact lenses in order to remove potential allergens. Patients should be instructed to use non-preserved products. Hydrogen peroxide-based cleaning solutions are best.
Prescription Relief
Numerous therapeutic options are available to treat allergic conjunctivitis. Topical antihistamines reversibly block histamine receptors and can reduce redness and treat symptoms acutely. Mast-cell stabilizers are helpful in preventing the occurrence of symptoms by blocking mast-cell degranulation. Combination antihistamine/mast-cell stabilizers provide both blockade of the H1 receptors and prevention of degranulation. Since these medications are more effective than monotherapy, these are the most commonly prescribed treatments for allergic conjunctivitis.
Olapatadine hydrochloride 0.1% (Patanol, Alcon) was the first combined antihistamine/mast-cell stabilizer. It has H1 antagonist activity and is very effective in treating the itching, redness and chemosis associated with allergic conjunctivitis. Epinastine 0.05% (Elestat, Allergan) is the newest combination agent. It is also effective in treating symptoms. Ketotifen 0.025% (Zaditor, Novartis) and Azelastine 0.05% (Optivar, Muro) are also in this category. These drops can be applied twice daily, 20 minutes before lenses are placed and after removal.
Topical steroids are also effective for treating allergic conjunctivitis. However, steroids can predispose patients to ocular infection, increased intraocular pressure and cataract formation, so they should be used with caution. If topical steroids are necessary, the patient must discontinue lens wear.
Don't forget that nonprescription rewetting agents like CIBA's new AQuify can help increase lens tolerance. Also, preservative-free artificial tear preparations can be used to both irrigate allergens from the eyes and treat mild symptoms. Refrigerated, these drops give additional symptomatic relief.
Evaluate Individually
Customize your treatment to each individual and to the severity of the allergic reaction. Often during peak allergy periods, patients will still need to reduce contact lens time or discontinue lens wear completely.
With careful evaluation, modification of lenses and lens care products, and topical therapy we may be able to keep our allergic contact lens patients in their lenses safely and comfortably. However, even with this thorough approach, removal of the contact lenses for a period of time may be the treatment of choice.
Contact Dr. Suchecki in the ophthalmology department at the University of Connecticut Health Center: (860) 679-7580 or jsuchecki@adp.uchc.edu.




