This year, studies shed new light on using contact lenses to deliver drugs to the eye; orthokeratology; scleral lenses; contact lens comfort; keeping lenses clean; and contact lenses’ impact on myopia progression. (Unless noted in the text, studies had no commercial support.)
Delivering Drugs to the Eye
A new contact lens designed to elute latanoprost, developed by researchers at the Massachusetts Eye and Ear Infirmary and Massachusetts Institute of Technology, was tested in vitro and in vivo using rabbits to determine how the drug released over time and how much drug reached the anterior chamber fluid compared to using standard eye drops.
For the in vitro test, the lenses were placed in phosphate-buffered saline kept in continuous rotation; the media was sampled and changed every day. Measurement showed that the lenses released a burst of the drug on the first day and then eluted a sustained, therapeutic amount every day for four weeks.
For the in vivo test, a contact lens was placed on the left eye of three New Zealand white rabbits for 10 days. The right eye of each rabbit received topical drops of latanoprost 0.005% solution. Through 14 days of continuous wear, the lenses showed no signs of toxicity, and they delivered more drug to the anterior chamber every day than the topical drops.479
An in vivo rabbit study conducted at Toho University in Tokyo, supported by the SEED company (Kounosushi, Japan), tested a new soft hydrogel contact lens designed for sustained release of gatifloxacin or moxifloxacin. Concentrations in the cornea, aqueous and crystalline lens were compared to eyes receiving topical drops.
• Maximum GATI concentration in the cornea at 10 minutes was 9.5 µg/ml in the contact lens group, vs. 0.7 µg/ml in the topical drop group. Maximum MOXI concentration in the cornea at 10 minutes was 23 µg/ml, vs. 2.4 µg/ml in the drop group.
• Maximum GATI concentration in the aqueous humor at 60 minutes was 13.4 µg/ml, vs. 1.1 µg/ml in the topical drop group. Maximum MOXI concentration in the aqueous humor at 60 minutes was 60 µg/ml, vs. 6.4 µg/ml in the topical drop group. All corneal and aqueous concentration differences were statistically significant.
• After 72 hours of contact lens wear, GATI concentration in the cornea was 0.04 µg/ml; MOXI concentration was 0.89 µg/ml. In the aqueous humor GATI concentration was 0.08 µg/ml; MOXI was 3.2 µg/ml.
Antibiotic concentrations in both the aqueous humor and cornea were approximately 10 times higher in eyes wearing the contact lens than in eyes receiving topical drops. The contact lens provided sustained release of the antibiotics through 72 hours.6102
Preventing Biofilm
A group of researchers at Texas Tech University Health Science Center in Lubbock, Texas, has found that selenium covalently incorporated into contact lens case material may inhibit the formation of biofilm for many weeks. (Two of the study authors work for Selenium Ltd.)
The authors note that silver has been used for this purpose, but it has several drawbacks, including cost, minimal effectiveness against S. aureus and some fungi, and having to leach out of the material to be effective. Selenium is less costly and doesn’t have to leach out of the case to work; it kills via the catalytic formation of superoxide radicals.
Selenium-imbued polypropylene was injection molded into contact lens cases. S. aureus bacteria were allowed to grow in the presence of the polypropylene, with or without selenium, for 24 hours. The selenium-imbued case showed complete inhibition of S. aureus, and was fully active after soaking in phosphate buffered saline for the equivalent of eight weeks.6081
Contact Lenses and Myopia
Researchers at multiple schools of optometry and universities conducted a retrospective study, supported by Alcon, designed to describe predictive factors associated with myopic progression in young soft contact lens wearers. (Several of the authors had consulted for CIBA Vision, Johnson & Johnson and Bausch + Lomb.) The authors reviewed the charts of a myopic cohort from the Contact Lens Assessment in Youth study. Subjects were myopes aged 8 to 22 with at least -0.5 D spherical correction in the less-myopic eye, and a maximum of 1 D of cylindrical correction in the most astigmatic eye. Subjects (666 experienced and 246 neophyte contact lens wearers) were observed at 4,341 visits with a mean follow-up of 24.4 months. At baseline, 37 percent wore hydrogel lenses and 63 percent wore silicone hydrogel lenses.
The data showed:
• Significant factors relating to myopia increases were: starting contact lens wear at age 8 to 13 years; higher starting contact lens power; shorter time to first change in power; and lens material.
• The mean change in power over the observation period varied inversely with age, ranging from -0.4 D/yr. in 8 to 10 year olds to -0.1 D/yr. in 20 to 22 year olds (p<0.0001).
• Of the 551 wearers who increased in minus during the observation period, increases of -0.5 D or greater occurred more often in moderate myopes (defined as greater than -3 D), compared with low myopes of the same age (p=0.003).
• After controlling for age, less progression was observed in users of SiHy materials (p=0.003).4719
Multiple centers in Sydney, Australia, Guangzhou, China and Houston, Texas, conducted a two-phase, randomized study to determine whether reducing peripheral hyperopic defocus using distance-center relatively plus peripheral power soft contact lenses slows myopia progression.
In phase 1, 40 children aged 8 to 14 years with myopia -0.5 to -4 D and cylinder of 0.75 D or less were randomized to wear either: A) a test lens with a relatively narrow 2.3-mm central optical zone, with back vertex power to correct the child’s distance vision and a +1.5 D peripheral optical zone; or B) a single-vision control lens in the same material, monitored for 43 ±4 months. In phase 2, the remaining subjects wore test lenses in both eyes for two more years. Refractive error and axial length were measured every six months. The data showed:
• During phase 1, refractive error in the test lens group vs. control lens group was -0.37 ±0.43 D vs. -0.59 ±0.32 D at 12 months; -0.61 ±0.30 D vs. -0.99 ±0.46 D at 24 months; and -0.99 ±0.58 D vs. -1.63 ±0.66 D at 43 months. Axial length in the test lens group vs. control lens group was 0.12 ±0.12 mm vs. 0.21 ±0.10 mm at 12 months; 0.22 ±0.15 mm vs. 0.39 ±0.17 mm at 24 months; and 0.41 ±0.24 mm vs. 0.67 ±0.29 mm at 43 months.
• The slopes of change in refractive error and axial length over 43 months were significantly less for the test lens than for the control lens (p<0.0001).
• The test lens reduced LCVA by 0.12 logMAR units (p=0.021).
The peripheral plus design lenses slowed rate of progress of myopia by 39 percent and axial elongation by 41 percent over 43 months.6300
The Power of Scleral Lenses
Two studies reported this year focused on the utility of rigid gas permeable lenses, which rest on the sclera and maintain a fluid reservoir between the lens and the cornea, for managing different ocular conditions.
One retrospective study conducted at the Mayo Clinic in Rochester, Minn., sought to evaluate the usefulness of these lenses when managing ocular surface disease. Chart data for 114 patients with ocular surface disease (age r: 6 to 85) who were fit with Jupiter scleral lenses (Visionary Optics & Essilor Contact Lens) between June 2006 and November 2011 were reviewed. Conditions managed with the lenses included:
• chronic graft vs. host disease;• exposure keratopathy;• neurotrophic keratopathy;• Salzmann’s nodular degeneration;• limbal stem cell deficiency;• Sjögren’s syndrome;• post-refractive surgery dry eye;• ocular cicatricial pemphigoid;• and uncomplicated dry-eye syndrome.
Most patients had previously tried other interventions.
The data showed that completion of the fitting process required an average of three visits (r: two to six), and an average of 1.4 lenses (r: one to three) per eye. (All patients were successfully fit.) In addition to managing the ocular surface problems, median visual acuity improved from 0.22 logMAR (Snellen equivalent, 20/33) with habitual correction, to 0.08 log MAR (Snellen equivalent, 20/24) after scleral lens wear (p<0.003, n=183).4715
A second retrospective study, conducted at Moorfields Eye Hospital in London, sought to determine the effectiveness of scleral lenses for managing corneal transplant and keratoconus patients. (One author has a financial interest in a scleral lens manufacturing company.) The authors reviewed data from 612 patients managed with scleral lenses (mean age: 56 years). In the study, 81.4 percent of the eyes (n=700) had undergone penetrating keratoplasty; 17.9 percent (n=160) had keratoconus.
In the keratoconus group, mean unaided visual acuity improved from 2/60 to 6/11; 75 percent achieved a visual acuity of at least 6/12; 23.8 percent achieved a visual acuity of at least 6/6. In the corneal transplant group, mean unaided VA improved from 3/60 to 6/10; 81.9 percent of eyes achieved a visual acuity of 6/12 or better; 37.9 percent reached 6/6 or better.4716
Comfort and Surface Impact
| |||||||||||||||||||||||||||||||||
Seventy-eight subjects were enrolled; 41 had previously reported reduced comfort and vision after wearing lenses for several weeks; 37 were asymptomatic. All wore their usual lenses for two 30-day cycles of daily wear. During one randomized cycle, the lenses were replaced with new lenses at day 28, without the knowledge of the wearers. Investigators were masked as to which cycle included the switch. Comfort and vision were graded at days one, 14, 27 and 29 in each cycle.
The data showed that comfort and vision decreased significantly with lens age in both the symptomatic and asymptomatic groups, although the overall decrease in ratings and the speed of the decrease was greater in the symptomatic group. Most interesting, masked replacement at day 28 had no significant effect on the subjects’ ratings at day 29 (p=0.524), in either group.4722
Researchers at the University of Waterloo in Ontario and the School of Medicine at Deakin University in Geelong, Australia, funded by CIBA Vision, have developed a new way to rate contact lens comfort. They noted that general end-of-day ratings of comfort exclude cases in which subjects removed lenses earlier in the day due to discomfort. The new system incorporates these cases into the equation by summing comfort scores for each hour of lens wear, producing a “cumulative comfort” score.
Subjects (n=104) wore three types of lenses: Dailies Total1; Clariti 1-Day; and 1-Day Acuvue TruEye. Each type was worn for three days. On day two, comfort ratings were recorded after four, eight and 12 hours of wear, and at the end of the day (prior to removal) whenever that occurred, using a 0-to-100 scale. Cumulative comfort was calculated using the score at each rating time, multiplied by the number of hours in the preceding segment. (See chart, above.)
|
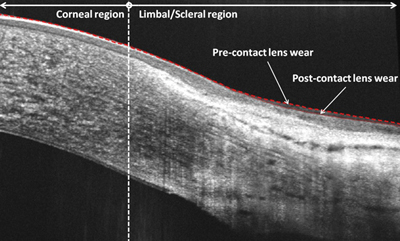
Researchers at the School of Optometry at Queensland University of Technology in Brisbane, Australia, decided to use anterior OCT to investigate the impact contact lens wear has on the limbal/scleral region of the eye. Three different contact lenses were tested: hydrogel sphere; silicone hydrogel sphere; and silicone hydrogel toric. At least one day with no contact lens wear was required between different lens tests.
Using SD-OCT, nasal and temporal horizontal 5-mm B-scans centered on the limbus were taken of six subjects, before and after six hours of contact lens wear. To assess the shape of the ocular surface, points were manually selected along the first hyper-reflective layer. Each scan was divided into corneal and limbal/scleral regions using the termination of Bowman’s layer as the dividing line. The scans revealed only a slight variation in the profile of the corneal region following contact lens wear (mean RMSE=3.8 μm); a greater variation for the limbal/scleral region was observed (mean RMSE=9.3 μm). These variations were significantly greater in the nasal location than the temporal location (p<0.05). (See image, above.)
Comparing the different contact lenses, the mean RMS errors were significantly greater for the toric lens (14.3 μm) than for the two spherical lenses (8.6 μm silicone hydrogel, 8.7 μm hydrogel). However, this was only true for the nasal location (p<0.05).4729
Analyzing Ortho-K
A study conducted at the School of Optometry and Vision Science at the University of New South Wales in Sydney, Australia, supported by Bausch + Lomb, BE Enterprises and Capricornia Contact Lens, monitored 19 myopic subjects, age 18 to 38 years, wearing BE OK lenses (Capricornia) overnight only, for a minimum of two weeks. The goal was to investigate the time course of the effects caused by the lenses. Central refractions at the outset were between -1 and -4 D.
After one, four, seven and 14 nights of OK lens wear, peripheral refraction was measured at 10, 20, 30 and 35 degrees in the nasal and temporal visual field. Corneal topography was also measured, and corneal refractive power was calculated at points along a horizontal corneal chord extending out to 2.8 mm on the nasal cornea and 1.5 mm on the temporal cornea.
The data revealed:
• There was a significant change in spherical equivalent over the 14 days of OK treatment at all positions (p<0.05) except at 35 degrees in the temporal visual field and 20 and 30 degrees in the nasal visual field.
• At the positions showing a change in spherical equivalent, the general trend was a hyperopic shift, except at 35 degrees in the nasal field where there was a myopic shift.
• The most significant change occurred between baseline and day one.
• There was a significant change in corneal refractive power at all positions along the horizontal corneal chord (p<0.001).
• The general trend was a reduction in corneal power or flattening of the cornea at all positions, except at 2.4 mm and 2.8 mm on the nasal cornea, where there was an increase in corneal refractive power.4713
Keeping Lenses Clean
A retrospective study was conducted at multiple centers in Australia and India to find out whether continuous-wear contact lenses would be associated with fewer corneal erosions if the lenses were cleaned or replaced in the morning or in the evening.
The researchers looked at data collected during previous continuous-wear studies conducted at the same locations. All subjects wore silicone hydrogel lenses (lotrafilcon A, CIBA Vision) on a 30-night overnight wear schedule. One group (n=87) discarded worn lenses and replaced them with new lenses every morning; a second group (n=90) replaced their lenses every evening; a third group (n=100) removed and cleaned their lenses every morning with a commercial multipurpose solution (Complete Easy Rub, AMO) and immediately reinserted them. A fourth, control group (n=95) wore their lenses for one month and then discarded them. Clinic visits were conducted at one week, one month and three months.
Analysis showed the risk of mechanical events—corneal erosion, superior epithelial arcuate lesion or contact lens papillary conjunctivitis—was 0.8 percent for morning lens replacement, 1 percent for morning lens cleaning, 3.4 percent for nightly lens replacement and 5.2 percent for monthly lens replacement. The reduction in risk was significant for morning lens replacement (p=0.013) and morning lens cleaning (p=0.031) at one month and at three months (p=0.042), compared to the alternative protocols.
The authors note that the mechanical events were primarily corneal erosions, the incidence of which was 0.6 percent for morning lens replacement, 0.5 percent for morning lens cleaning, 3.4 percent for nightly lens replacement and 3.1 percent for monthly lens replacement. They conclude that mechanical adverse events might be reduced by switching patients to a morning replacement or cleaning protocol.6092 REVIEW
Dr. Asbell is a professor of ophthalmology and the director of cornea and refractive surgery at the Mount Sinai School of Medicine.