|
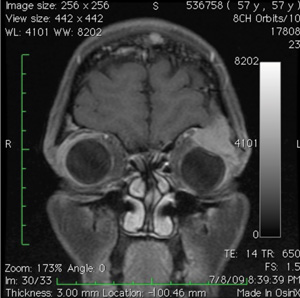
New ptosis must be evaluated in the context of other presenting symptoms.Anisocoria or limitation of extraocular movements may indicate a third cranial nerve palsy or Horner syndrome. In the absence of these signs, aponeurotic, myogenic or mechanical ptosis must be considered. Given the patient’s history of cancer and the relatively quick development of ptosis, MRI imaging was urgently obtained to rule out orbital metastatic disease.MRI revealed a superotemporal orbital mass (See Figure 2). Further CT imaging characterized bony erosion by the mass.
Differential diagnosis for superotemporal orbital mass includes inflammatory or neoplastic lesions. Inflammatory conditions include sarcoidosis, idiopathic orbital inflammatory syndrome, lymphoid hyperplasia or infectious cellulitis. Neoplastic entities in this location include adenoid cystic carcinoma, pleomorphic adenoma, lymphoma and metastatic disease.
Given the patient’s history, orbital multiple myeloma, or secondary plasmacytoma, was the favored diagnosis. Biopsy was deferred given the characteristic location and appearance of the lesion on imaging.The patient’s oncologist was contacted, and radiation therapy was considered.Chemotherapy was adjusted and augmented by her oncologist, and this resulted in decreased tumor size. The left-sided ptosis eventually resolved without need for radiation or surgical intervention (See Figure 3).
The patient continues to undergo periodic imaging to monitor for recurrence of tumor growth, but has remained in remission thus far.
Discussion
Multiple myeloma is a common hematologic malignancy consisting of clonal proliferation of plasma cells within bone marrow. It is often discovered incidentally.
While numerous therapies, such as stem cell transplantation, lenalidomide and bortezomib, have extended overall survival, 10- year survival for patients diagnosed under the age of 60 remains around 30 percent. Multiple myeloma may be asymptomatic, or manifest with skeletal pain due to lytic bone lesions, fatigue due to anemia, renal failure or hypercalcemia.
Orbital involvement in multiple myeloma is considered rare, though intraocular manifestations occur more frequently. Corneal crystal deposition, serous retinal detachment and hyperviscosity retinopathy may be observed as first presentation of the disease, or in patients with a known history of multiple myeloma.
Orbital multiple myeloma may present as a plasmacytoma, which is an isolated clonal proliferation of plasma cells in the absence of other skeletal lesions.
Another lesion on this spectrum is primary/solitary extra medullary plasmacytoma, which occurs in soft tissue rather than bone, and may invade the orbit via the sinuses. In a patient with a known history of multiple myeloma, the presentation of such lesions is considered a secondary plasmacytoma. There is some suggestion that patients with IgG heavy chain multiple myeloma may have greater orbital involvement than those with IgA, though some studies find no statistically significant difference between the two groups. Patients with isolated tumors have a better prognosis than those who have or develop systemic multiple myeloma.
Treatment of these orbital tumors includes focal irradiation or chemotherapy; the latter is often an adjunct for those with systemic signs of disease. Surgery is usually contraindicated due to its low success rate, unless there are signs of neurologic or structural compromise.
As with any orbital process, presenting signs and symptoms may include proptosis, diplopia, ptosis and hypoglobus.Onset of orbital multiple myeloma tends to be insidious, but two-thirds of patients who present already carry a known diagnosis of systemic multiple myeloma.Therefore, physicians should have a low threshold for imaging patients with the above symptoms, especially if a history of neoplasm exists. CT imaging is preferred, as it provides superior representation of bony structures and lesions. REVIEW
Multiple myeloma is a common hematologic malignancy consisting of clonal proliferation of plasma cells within bone marrow. It is often discovered incidentally.
|
Orbital involvement in multiple myeloma is considered rare, though intraocular manifestations occur more frequently. Corneal crystal deposition, serous retinal detachment and hyperviscosity retinopathy may be observed as first presentation of the disease, or in patients with a known history of multiple myeloma.
Orbital multiple myeloma may present as a plasmacytoma, which is an isolated clonal proliferation of plasma cells in the absence of other skeletal lesions.
|
Treatment of these orbital tumors includes focal irradiation or chemotherapy; the latter is often an adjunct for those with systemic signs of disease. Surgery is usually contraindicated due to its low success rate, unless there are signs of neurologic or structural compromise.
As with any orbital process, presenting signs and symptoms may include proptosis, diplopia, ptosis and hypoglobus.Onset of orbital multiple myeloma tends to be insidious, but two-thirds of patients who present already carry a known diagnosis of systemic multiple myeloma.Therefore, physicians should have a low threshold for imaging patients with the above symptoms, especially if a history of neoplasm exists. CT imaging is preferred, as it provides superior representation of bony structures and lesions. REVIEW
The author would like to thank attending physician Sara Lally, MD, of the Wills Eye Ocular Oncology Service.
1. Aggio FB, Cariello AJ, Almeida MS, Rodrigues CA, et al. Bilateral central retinal vein occlusion associated with multiple myeloma. Ophthalmologica 2004 Jul-Aug;218(4):283-7.
2. Brenner H, Gondos A, Pulte D. Recent major improvement in long-term survival of younger patients with multiple myeloma. Blood 2008;111:2521-6.
3. Burkat CN, Van Buren JJ, Lucarelli MJ. Characteristics of orbital multiple myeloma: A case report and literature review. Surv Ophthalmol 2009;54(6):697-704. Epub 2009 Aug 25.
4. C-M Hsueh, P-Y Lin, S-M Lee and W-M Hsu. Corneal crystalline deposits as the initial manifestation of IgA-kappa multiple myeloma. Eye 2004;18:644–645.
5. Fung S, Selva D, Leibovitch I, Hsuan J, Crompton J. Ophthalmic manifestations of multiple myeloma. Ophthalmologica 2005;219(1):43-8.
6. Gonnering RS. Bilateral primary extramedullary orbital plasmacytomas. Ophthalmology 1987;94:267-9.
7. Knapp AJ, Gartner S, Henkind P. Multiple myeloma and its ocular manifestations. Surv Ophthalmol 1987;31(5):343-51.
8. Palamar M, Shields CL, Ghassemi F, Ehya H, Shields JA. Choroidal plasmacytoma in a patient with multiple myeloma. Diagnosis by fine-needle aspiration biopsy. Graefe’s Arch Clin Exp Ophthalmol 2008;246:1195-7. Epub 2008 Apr 2.
9. Palumbo A, Anderson K. Multiple myeloma. N Engl J Med 2011 Mar 17;364(11):1046-60.
10. Shields JA, Shields CL. Eyelid, Conjunctival and Orbital Tumors. Philadelphia: Lippincott, Williams, and Wilkins, 2008.