Presentation
A 29-year-old white male with a remote history of vertigo presented to the Wills Eye Emergency Room with a three-day history of a visual distortion and dizziness. The patient described oscillopsia and difficulty looking upwards. At the time of presentation the patient denied associated diplopia, headache, tinnitus, weakness, numbness, gait instability or trauma.
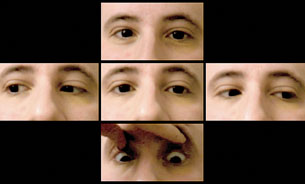 |
| Figure 1. Clinical photos demonstrating patient’s motility. The patient’s globes were noted to pull inward and retract with attempted upgaze. |
The patient had a remote history of vertigo approximately three years prior to presentation that subsequently resolved. His past ocular history was significant for high myopia. His family history and review of systems were noncontributory. The patient denied tobacco, alcohol and intravenous drug abuse.
Examination
The patient’s examination revealed a corrected visual acuity of 20/400 in each eye at distance and 20/20 in each eye at approximately 13 mm. Color plates were 8 out of 8 briskly in each eye with normal Amsler grids bilaterally. Gross exam showed no mass, proptosis, lid lag or lid retraction. Pupils were briskly reactive without an afferent pupillary defect or Horner’s syndrome. Visual fields were full by confrontation and by Humphrey’s perimetry. The patient had 90 percent normal abduction in both eyes with absent elevation and convergence-retraction nystagmus on attempted upgaze (See Figure 1). Slit-lamp exam was white and quiet. Intraocular pressure was 11 mmHg and 13 mmHg in his right and left eyes, respectively. Dilated fundus exam was normal.
What is your differential diagnosis? What further workup would you pursue?



