The fact that a refractive surgerypatient can see 20/20 but still be unhappy with his vision concerns both ophthalmologists and the makers of excimer lasers, who want to make their patients "20/Happy" if not 20/20 or better. In response to the possibility of this unfortunate result, laser makers have turned to everything from altered ablation patterns to wavefront-guided ablations to improve not just how many letters a patient can see, but how well he can see them. However, to improve visual quality, the patient may have to sacrifice something, such as corneal tissue.
In this, the final article in a three-part series on this apparent trend toward emphasizing qualitative vision post-LASIK, Review looks at Visx's wavefront-guided ablations.
The Qualitative Question
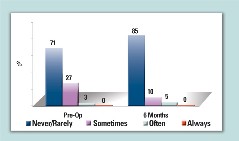
Table 1. Frequency of Glare, Custom Treatment
Surgeons who took part in the latest Visx trial of its WavePrint system for customized ablation say the shift toward qualitative results may not be overt.
"I don't know if I'm overtly trying to say that we're going for 20/15 or 20/10," says Chicago surgeon and Visx investigator Colman Kraff. "I think we got caught up with it as a result of the wavefront studies we did, though the goal of the Visx studies wasn't to give people 20/10 vision."
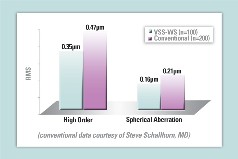 |
| Table 2. Comparison of One-Month Aberrations |
"I think were realizing that Snellen acuity isn't a real good way to measure a patients satisfaction with his vision," he says. "Just because you can read smaller letters doesn't mean you're necessarily happier with your vision. Plus, how small of a letter do you really need to read? Our world is set up so that if you can read a sign from four miles away rather than one mile, it doesn't really give you much of an advantage. Patients also don't want annoying side effects such as glare or halo."
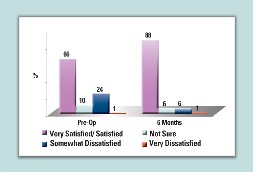 |
| Table 3. Patient Satisfaction: Vision at Night |
The WavePrint System
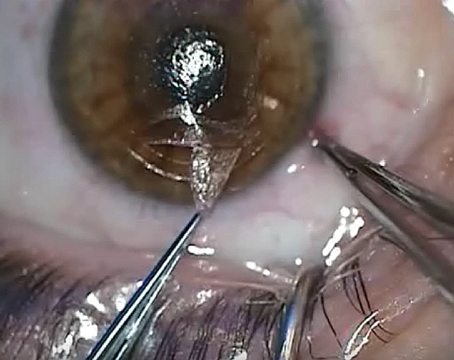
This system uses a Hartmann-Schack based aberrometer to plot a customized LASIK ablation. In addition to correcting higher-order aberrations, the system also allows the user to leave the patient with a more prolate-shaped cornea, which could reduce spherical aberration. The system is in the final stages of its U.S. Food and Drug Administration clinical trial.
To create a custom ablation, the patient's eye is first imaged by the aberrometer. It then creates a custom laser shot pattern for the patient's cornea, and allows the user to decide on how much of a trade-off he wants to make between correcting the aberrations and the depth of the ablation. Its also at this time that the user decides how prolate he wants the cornea to be postop. The user enters the desired residual bed thickness, the expected flap thickness and pachymetry, and the computer informs him how much tissue will need to be removed to eliminate a certain percentage of the wavefront aberrations.
As an example (these numbers aren't accurate but for discussion purposes only), Dr. Hardten says if the surgeon wants to make a 7-D myope so prolate that his spherical aberration is reduced to nearly zero, it might take 350 µm of tissue to maintain his 41 D central steepness and a 38-D K in the mid-periphery. However, if he wanted to instead place a milder oblate shape on the cornea, maybe 42 D in the center and 41 in the mid-periphery, it might only take 120 µm to do this. The balance between depth of tissue removal and optimum corneal shape is still evolving. There are also disadvantages to going too deep.
• Results. In the Visx FDA study, 320 eyes of 173 patients underwent wavefront guided LASIK. Their average preop spherical equivalent error was -3.2 D.
At six months, they showed a greater improvement in aberrations compared to conventional treatments. Seventy-percent of patients had either a decrease in the root mean square value of their wavefront, which describes the level of aberrations in their eye, or an increase of smaller than 0.1 µm. (Tables 1-3 show some qualitative and aberration data from the Visx FDA study). Dr. Kraff says that longer-term data is unavailable at press time, as the FDA is reviewing it.
Though an aberrometer can tell a surgeon the amount of aberrations in a patient's eye, experts still aren't sure what those actually mean as far as patients being happy or unhappy.
"I've got some extremely happy patients with 1.0 µm of higher order aberrations, which would be a lot to some people," says Dr. Hardten. "And others with 0.21 µm who aren't happy at all." Knowing this fact, the result that will make a patient happy or not, may be the toughest goal of all, but it's the one everyone's reaching for.