Since its FDA approval in 2016, small-incision lenticule extraction has seemingly played the role of David up against the Goliath of LASIK. Whether it’s hesitancy to invest in the technology, doubts about outcomes or concerns about the learning curve, SMILE has been fighting an uphill battle in the world of refractive surgery. However, trends show SMILE is gaining some traction in certain parts of the world, and with advanced laser technology on the way, surgeons may not be able to ignore the advantages SMILE can offer to the right set of patients.
Accomplished refractive surgeons who have experience with performing SMILE on countless patients say that though they recognize the concerns their peers sometimes mention, they believe that the procedure should be more widely embraced. Here’s an update on the procedure.
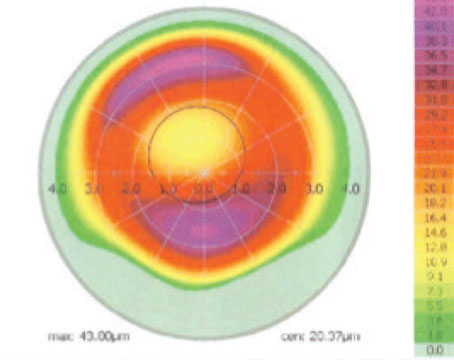
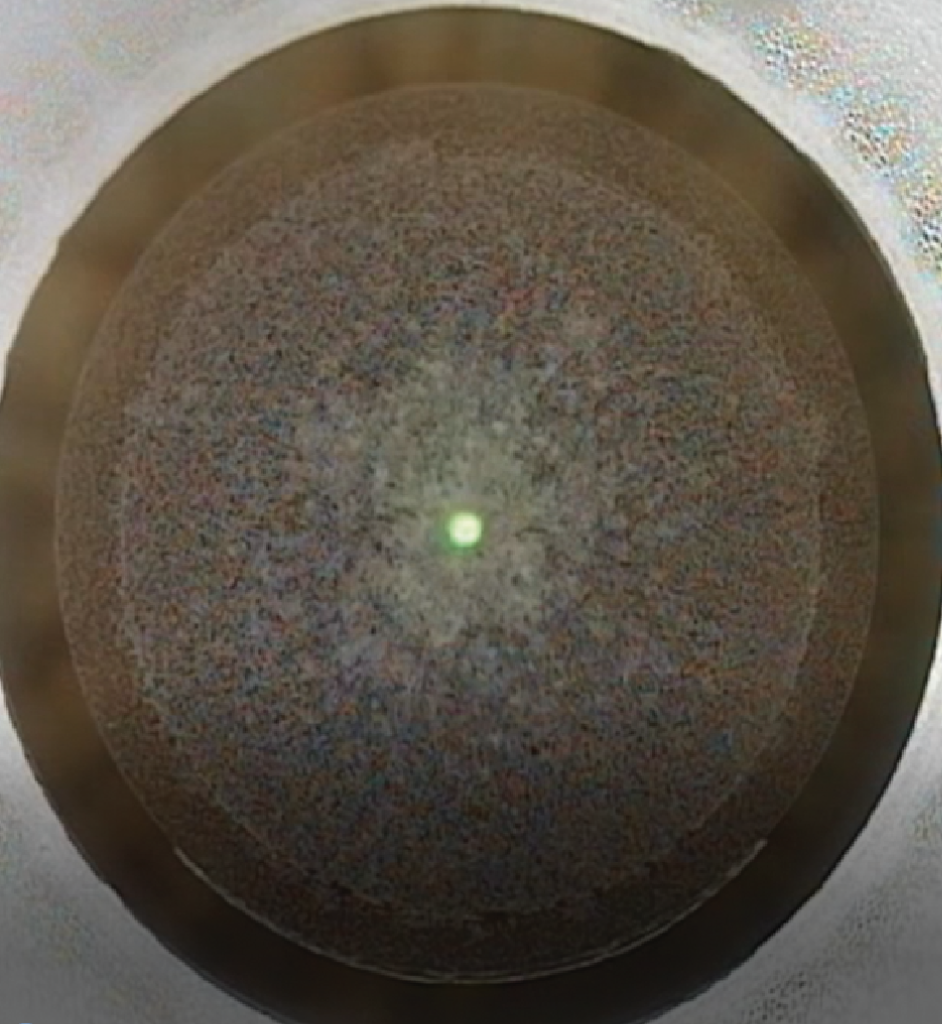
 |
| Bubble layer showing the femtosecond laser cut of the posterior plane (underside) of the lenticule. All images: Majid Moshirfar, MD, FACS. |
Challenges in the Market
There are a few factors contributing to SMILE’s slower adoption, one being patient awareness, says Majid Moshirfar, MD, FACS, director of the University of Utah’s Moran Eye Center Refractive Surgery and Cornea programs. “Unfortunately, one of the hindrances right now is patients still primarily get LASIK because their cousin got LASIK, or their mother got LASIK, and they don’t really want to hear about newer technology,” he says.
Edward Manche, MD, director of the Cornea and Refractive Surgery Service at Stanford University School of Medicine, has had similar experiences.
“When I meet patients who are interested in refractive surgery, I always present the three options of LASIK, PRK and SMILE,” he says. “Oftentimes, this is the first they’ve ever heard of SMILE, but many of them opt for LASIK because that’s what they are familiar with and had their mind set on.”
He adds that SMILE is becoming a bit more requested among patients who have friends and relatives from Asia. “In China and South Korea, for instance, SMILE has become more popular, so those patients will not only know about it, but they’ll be interested in having that surgery, so that’s where most of the SMILE-related growth in our practice has come from,” Dr. Manche says.
A recent press release from Market Scope showed the global refractive procedure break down (Figure 1), and in China, LASIK and SMILE are nearly equal, while in the U.S., SMILE still comprises only a small fraction of the procedures.
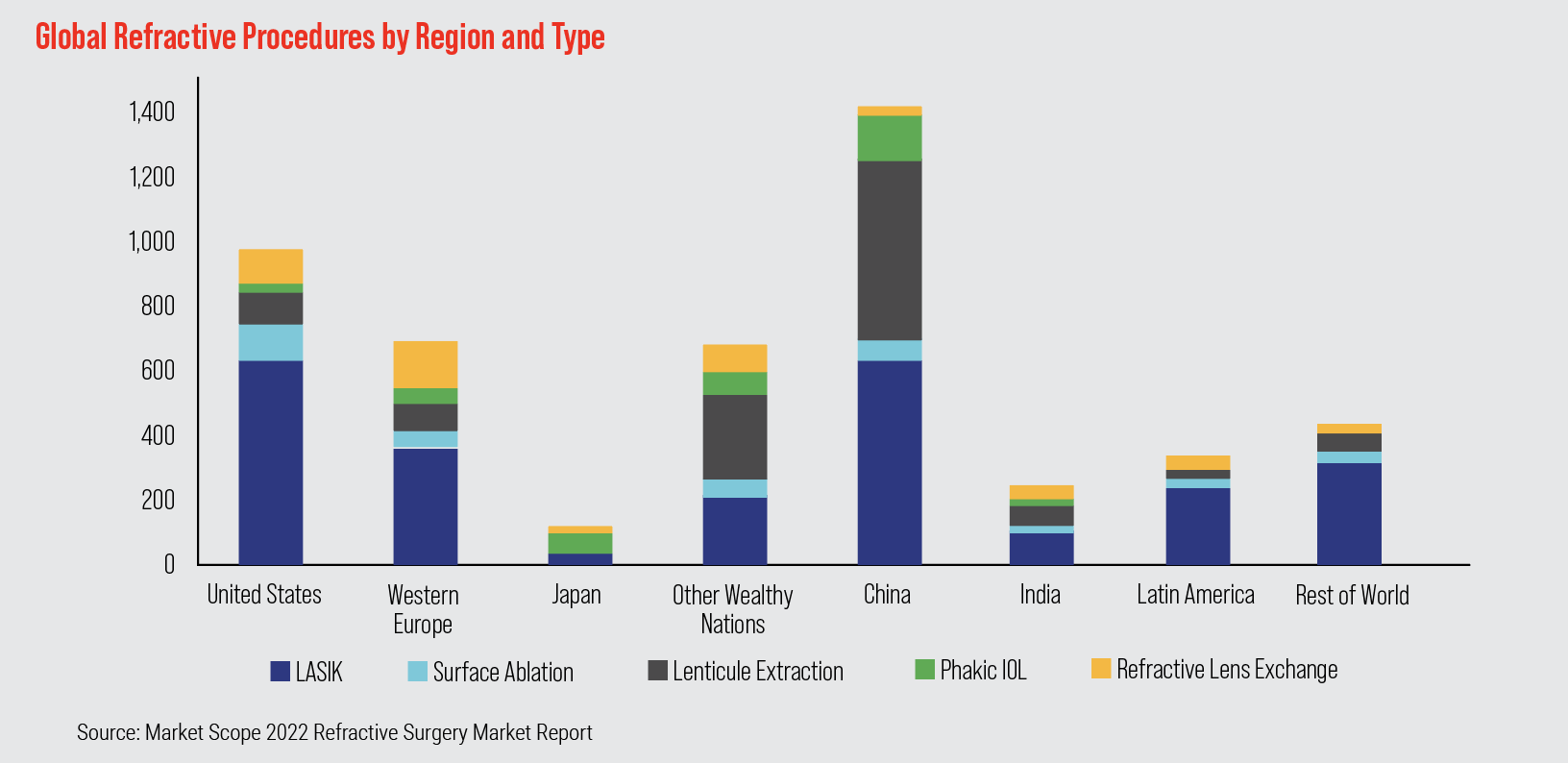 |
| Figure 1. A recent press release from Market Scope showed how SMILE stacks up against other refractive procedures internationally, and demonstrates its stronghold in Asia. |
Dr. Moshirfar estimates SMILE to be between 22 and 25 percent of his corneal refractive procedures. He attributes his own, as well as the country’s, lower adoption rates to the restrictions of the platform in the United States.
“There is a difference between the platform we have in the U.S. and the one that exists internationally,” he says. “We don’t have the flexibility of changing certain parameters. I cannot change the thickness of the SMILE cap, or the size or orientation of the incision, whereas in China and other parts of the world, they have more ability to offer SMILE to other people.”
U.S. surgeons are also limited on the level of astigmatism they can correct with SMILE, Dr. Moshirfar continues. “In the U.S., SMILE can only correct up to 3 D of astigmatism, but in Asia they can treat up to 5 D, so you can understand how that limits us.”
But he thinks percentages are bound to increase. “I wouldn’t be surprised if within three years SMILE will have a niche closer to 35 percent of patients,” he says.
This could be attributed to new femtosecond laser technology, says Dr. Manche. “There is currently only one manufacturer that makes the laser for SMILE approved in the U.S., and that’s Zeiss. Some surgeons see the purchase of another femtosecond laser as a cost barrier,” he says. “And there have been some concerns about the abilities of the machine, such as centration, post-docking adjustment and adjusting for cyclotorsion.”
Dr. Manche says there are other manufacturers outside of the U.S.-approved option, such as Ziemer and Schwind that do allow for these adjustments, and Zeiss’ next generation VisuMax 800 will also bring these capabilities.
“The new machines, including the VisuMax 800 will have the ability to center over the pupil,” he says. “This will make it significantly better and being able to compensate for cyclo-rotational movement will also help with astigmatic outcomes.” VisuMax 800 will also cut the lenticule in about 10 seconds.
“I think the technology is becoming more mature with these refinements and advancements, not only from Zeiss, which is the company that invented and popularized this procedure, but now there are other companies in the market and that will speed up development and innovation,” Dr. Manche continues.
Dr. Moshirfar says this evolution of technology is standard for any procedure and its corresponding technology, and reminds his colleagues of the earliest days of LASIK. “When I started with LASIK in 1996, it was very crude. It took years before we were able to use a flying-spot laser. Predictability got better, the hertz on the laser went up, and then we got centration, then iris registration and cyclotorsion compensation,” he says. “And now of course, all of the LASIK lasers have these abilities, and the rest is history.
“Trying to compare the latest LASIK platform to SMILE is not a fair assessment,” he continues. “It’s like comparing a professional golfer to a high school player—it’s not the same thing. I think SMILE has a couple more years to go through refinement, but I think it’s unfair for anyone to say one is better than the other or worse than the other. I think the best thing for us is to embrace both of them and use both of them for the right patient with the right need.”
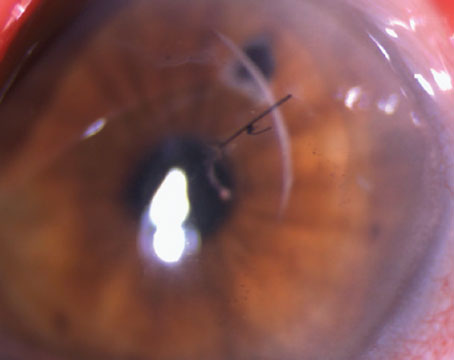
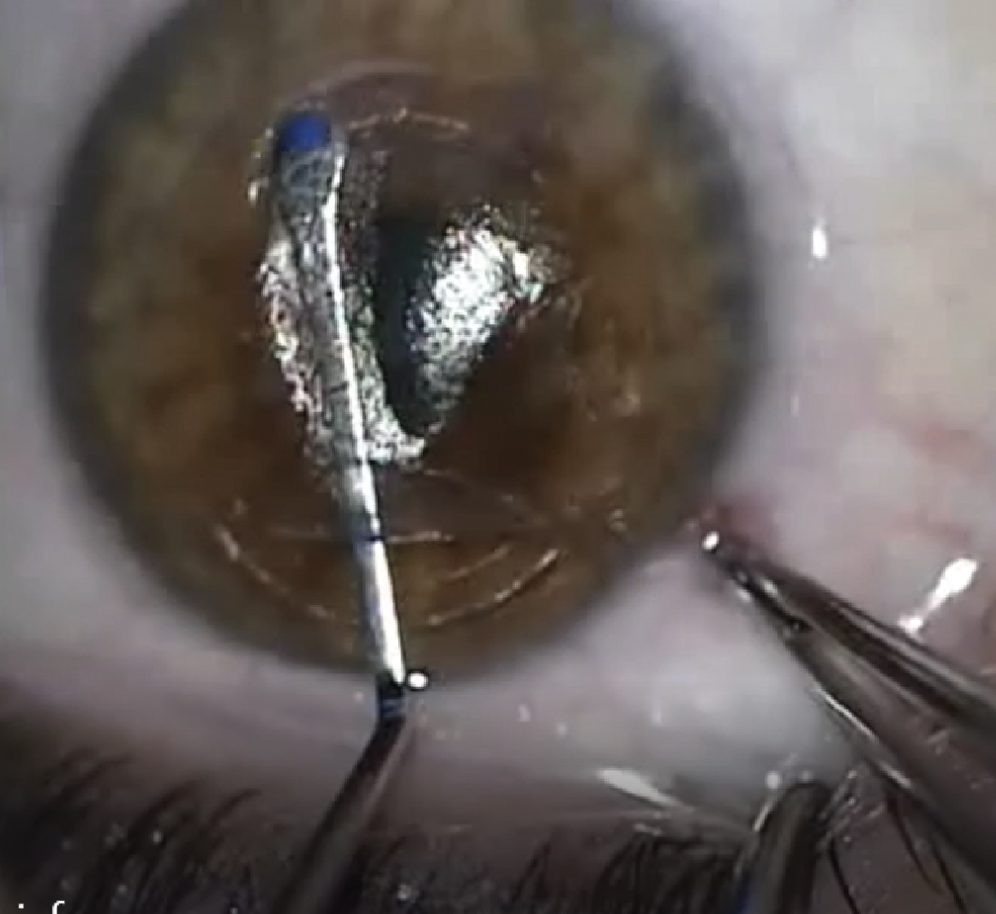
 |
| Bubble layer showing the cut of the anterior plane of the lenticule which is also the cap cut, and the 12 o’clock incision with the femtosecond laser. Notice the cap cut has a larger diameter than the posterior lenticular plane cut. |
Results and Tips On Technique
One of the misconceptions Dr. Moshirfar often hears from his colleagues about SMILE is that there’s a slower recovery of vision. He again points out that, in the early days of LASIK, patients were 20/60 or 20/50 on postop day one.
“I would say that I agree visual recovery is slower, but not to the same extent that it was in 2016 and 2017 when we first started with SMILE,” Dr. Moshirfar says. “I did six eyes last week and the worst one was 20/25. Every other eye was 20/20 or 20/20+.”
Dr. Manche says it’s important to counsel patients about this. “SMILE works very well and gets comparable outcomes to LASIK, however, LASIK patients typically see 20/20 or 20/15 on postop day one, but SMILE has a larger range,” he says. “You can see patients with 20/20, but more typically, in my hands at least, they’re 20/25 or 20/30 on postop day 1. Now, if you go out a month, they’re usually very comparable, but for the first few days patients will say the vision isn’t as clear, especially in the first 48 to 72 hours.”
SMILE is approved for patients with -1 to -10 D of myopia and -0.75 to -3 D of astigmatism.1
A meta-analysis of 12 studies involving 766 patients (1,400 eyes: 748 receiving SMILE and 652 receiving FS-LASIK)2 looked at postop clinical outcomes in high myopes after SMILE or LASIK. There were some advantages of SMILE in certain areas, including with CDVA, which was significantly better in the SMILE group than the FS-LASIK group (WMD = -0.04, 95% CI, -0.05 to -0.02, I2 = 0%, p<0.00001). Postop total higher-order aberration (WMD = -0.09, 95% CI: -0.10 to -0.07, I2 = 7%, p<0.00001) and postoperative spherical aberration (WMD = -0.15, 95% CI: -0.19 to -0.11, I2 = 29%, p<0.00001) were lower in the SMILE group than in the FS-LASIK group.2
Longer-term results are harder to come by, but a 10-year follow up of 56 of the first 91 eyes treated with SMILE between 2008 and 2009 showed no significant difference in the six-month postop data. Sixteen of the 56 eyes had gained one to two Snellen lines, and there was no loss of two or more lines.3
This gives surgeons confidence when recommending SMILE to patients, and there are other benefits to the procedure for patients to be aware of, proponents say.
“I point out that SMILE has a smaller incision than LASIK,” says Dr. Manche. “It’s a 4-mm incision, as opposed to a 20-plus mm incision for LASIK. If someone is an active athlete, boxer or mixed martial artist, there’s an argument that SMILE is potentially more advantageous because of the significantly lower risk of flap dislocation in a combat sport compared with LASIK since no flap is created with SMILE.”
Dr. Moshirfar says the lack of flap means there are fewer issues in the healing process. He anecdotally shared the story of a patient with Bell’s palsy. “I did SMILE in the eye with Bell’s palsy and LASIK in the other eye. If I had done LASIK in the eye with Bell’s palsy, the patient would have had worsening of the flap integrity and exposure keratopathy difficulty,” he says. “This is an example of using SMILE for the right patient and circumstances.”
Dr. Manche says he wouldn’t recommend SMILE if a patient has corneal scarring that would affect the formation of the cap or dissection of the lenticule. “You also want to make sure the cornea is in pristine condition and that there’s no dry eye, otherwise there’s a risk of having dry spots when you’re creating the lenticule,” he says. “Also ensure there are no meibomian gland secretions that could block the pulses. This sort of thing isn’t as important with LASIK flaps, but with SMILE it can make the dissection more challenging and you’d potentially have to abort the case.”
Dr. Manche says there are some biomechanical advantages to SMILE. He co-authored a study published in 2022 assessing corneal sensitivity in eyes that underwent SMILE and LASIK. Eighty eyes of 40 patients with myopia received LASIK in one eye and SMILE in the fellow eye. Eyes that underwent LASIK compared to SMILE demonstrated more corneal denervation at the postop one-month (mean 2.1 vs 3.6 cm, p<0.001), three-month (3.5 vs 5.4 cm, p< .001), and six-month (4.7 vs 5.7 cm, p<0.001) visits. At the 12-month visit, both groups had returned to baseline corneal sensitivity (5.9 vs 5.9 cm, p=0.908).4
Refractive surgeons often wonder about the risk of ectasia with SMILE, says Dr. Moshirfar. Ectasia development after refractive surgery may be due to a genetic predisposition. “Patients may not be developing ectasia because they received SMILE, but because of other factors. I’ve seen patients who had LASIK and then get keratoconus. Then we find out four years later, their brothers also have keratoconus but never had LASIK,” he says.
He studied this with colleagues, and in 2021 published a systematic review of ectasia after corneal refractive surgery. The study concluded that SMILE had the lowest rate of ectasia, but could prove problematic as patients get further out from surgery.5
As two surgeons who’ve been performing SMILE since its clinical trial days, they’ve refined their techniques somewhat but not drastically.
“When I first started doing SMILE, I was performing it on patients as low as -1 D up to higher corrections,” Dr. Manche says. “In my hands, I prefer not to do it in lower corrections, certainly not less than 2 D, because the lenticule becomes thinner in the lower corrections and it’s possible that it’s more prone to tearing when you’re dissecting it. For most corrections, I stay within -2.5 and above to -10 D.”
For Dr. Moshirfar, careful dissection is top priority. “My technique has always been about careful dissection of the anterior plane, followed by the posterior plane dissection,” he says. “The refinement in the spot separation and lower nanojoules of energy has helped with the ease of removing the lenticule, but the technique is the same.”
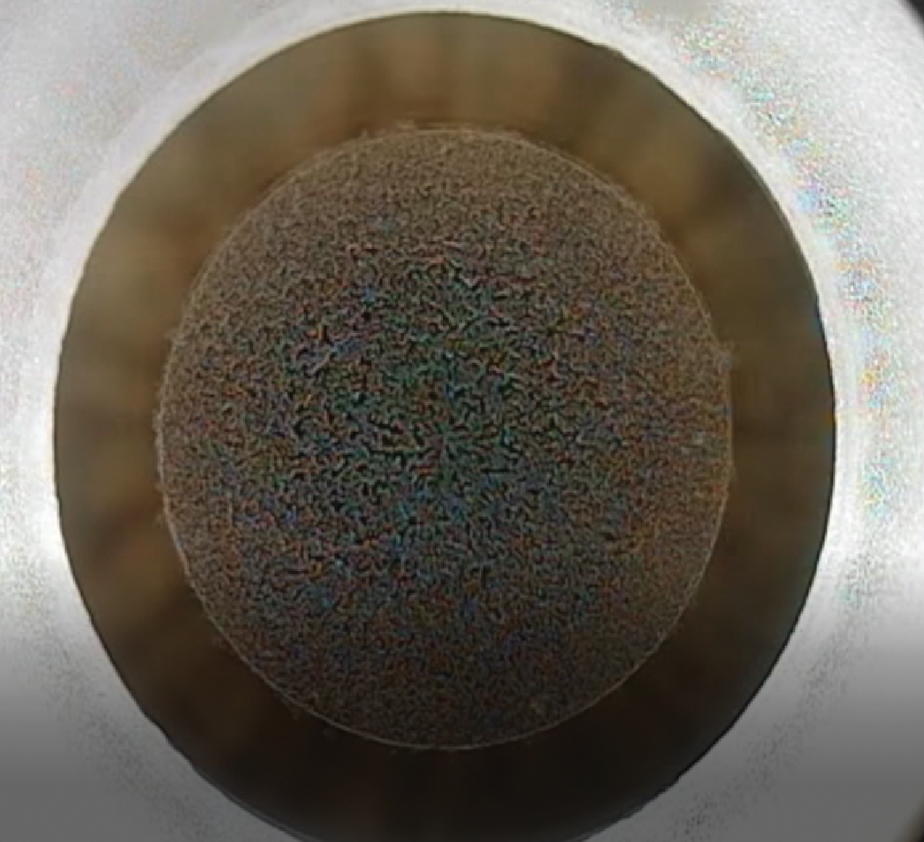
 |
| Dissection of the SMILE lenticule using a Reinstein Lenticule Separator, with forceps grasping the conjunctiva to stabilize the globe during dissection. |
He also notes that incisions were initially 4.5 mm and now they’re barely 3.9 mm. “I know internationally they have the ability of making two incisions, one on each side, each of them about 1.5 mm. I don’t have that ability in the U.S.,” he states. “But since the software and laser energy has become more refined, we’re seeing that the ease of removing the lenticule is getting better, but I don’t rush this procedure.”
Dr. Moshirfar also carefully inspects the lenticule under a microscope after removal. “I want to make sure I have removed the entire thing, and I usually save these lenticules,” he adds. “If there’s ever a question, or a patient comes back the next day and is 20/200—which hasn’t happened—I’m able to make sure I didn’t leave any remnants in the pocket of their SMILE.”
Another note for success is centration, says Dr. Moshirfar. “Always look at the patient in the clinic and make sure you know where the angle kappa is. Make sure that you know where the line of sight and the center of the pupil are with respect to one another, so that when you’re doing your centration in the laser suite, you know where the line of sight is. This may be automated in the future, but until then, this is important when you’re trying to create suction on the patient.”
Dr. Manche says that managing suction during SMILE may contribute to its reputation for a steep learning curve. “The VisuMax system is different that what most people use for traditional scleral suction where the suction ring goes directly onto the sclera and it holds the eye steady with quite a bit of pressure. With the VisuMax, it’s a curved interface instead of flat, and it uses corneal suction,” he says.
This can be good and bad. For one, it doesn’t raise the patient’s IOP, and it’s more comfortable, Dr. Manche says. “Another advantage is, since the suction is on the cornea, it doesn’t cause any subconjunctival hemorrhage. On the other hand, the gentle suction makes it potentially more prone to retreatment. If you lose suction during a LASIK flap, you can just re-engage with the same cone without issue. When you have suction loss during the first part of SMILE, you have to abort and convert over to LASIK or PRK.”
It’s best if surgeons consent patients for LASIK prior to their surgery if this happens. “We tell them, in the event we lose suction, we’ll convert to LASIK, and it’s not ideal because then they aren’t receiving their first choice procedure. It’s about one in 200 cases this may happen but it’s just one of those things that you have to be prepared for because you can’t really consent the patient for a second surgery while in the middle of the procedure,” Dr. Manche says.
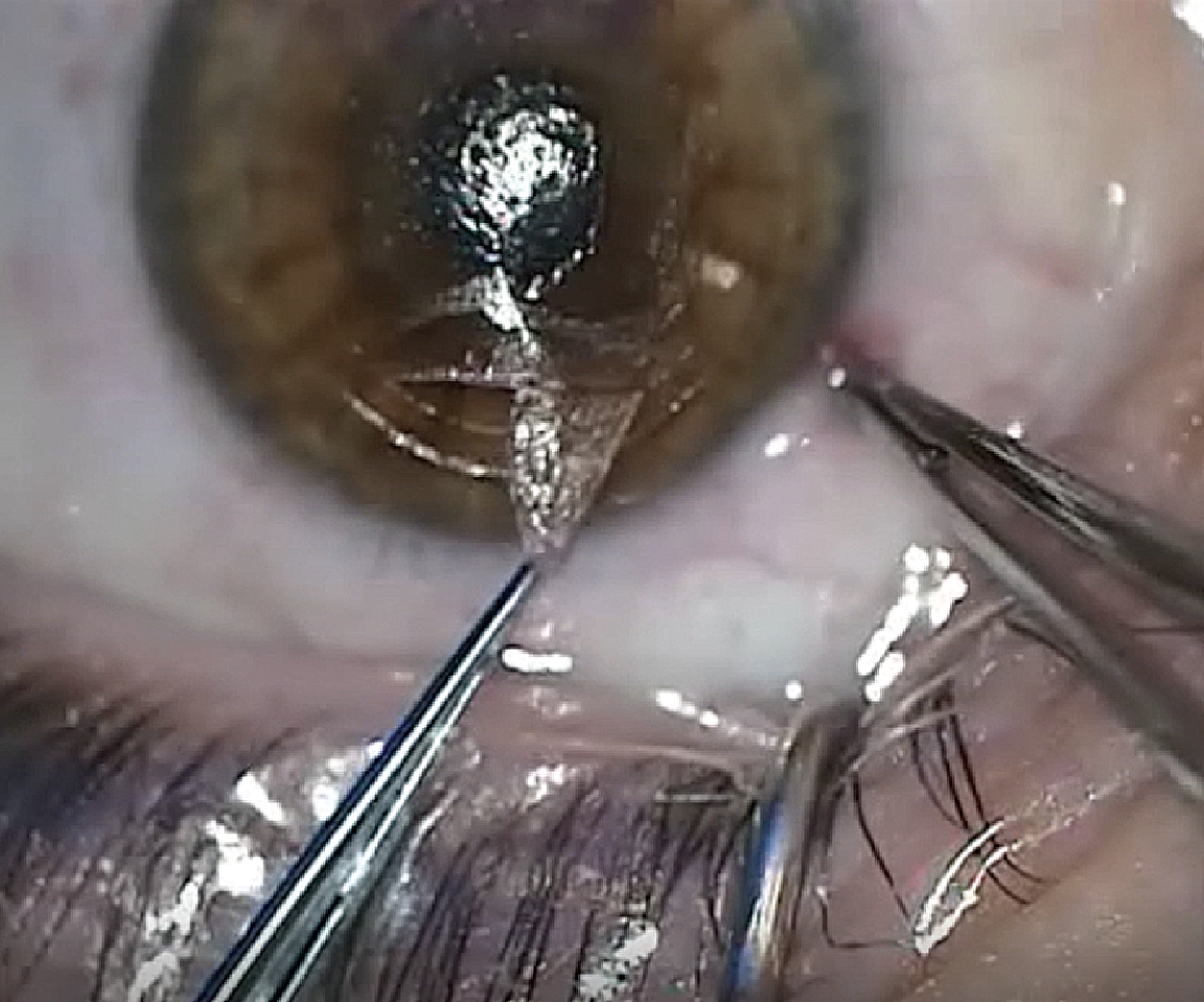 |
| Final extraction of the dissected and fully intact SMILE lenticule. |
Words of Wisdom
With regard to the learning curve, Dr. Manche says Zeiss offers a clinical application specialist who will come on site to assist with your first cases. “When we first started these surgeries, the energy settings were fixed at higher levels so patients had a delay in the visual recovery, but now we’re able to adjust the energy to lower levels and adjust the spot spacing, size and distance,” he says “When you work with the clinical application specialist, you work your way down in energy levels as you go through your cases to figure out what the optimal settings are.
“In addition to that, I recommend spending a day with another surgeon who’s doing SMILE who can walk you through what they’re doing,” Dr. Manche adds. “More importantly, if you can find someone who’s willing to work with you and help you on your initial cases, that would be helpful because it’s a newer procedure with subtleties to it.”
A pearl from Dr. Moshirfar involves bandage contact lenses and when to use them. “If you ever have a small area of epithelial aberration or defect at the time of your SMILE incision, you should always put a bandage contact lens on the surface for 24 hours,” he says. “You should have a very low threshold for these eyes.”
This also applies if a patient has silent map-dot fingerprint dystrophy. “When we dock on these patients’ eyes for LASIK, sometimes we can get into a flap complication. In SMILE, it’s much more forgiving, but they can sometimes develop irregular epithelium postop within the first four to 24 hours, and it may not be a bad idea to also put a bandage contact lens on these patients so their recovery will be faster,” Dr. Moshirfar says.
Both Drs. Manche and Moshirfar say SMILE is only going to get better as time passes and technology is introduced.
“I think that SMILE has done an incredible job to date competing with such mature technology as LASIK and PRK, and I think it will close the gap in the next few years and have virtually indistinguishable results with LASIK,” says Dr. Manche.
Dr. Moshirfar is working on a prospective, contralateral study analyzing results of LASIK in one eye and SMILE in the fellow eye. Although it’s in the early stages, Dr. Moshirfar says patients are doing equally well on both platforms.
Dr. Manche is a consultant for Avedro, Carl Zeiss Meditec and Johnson & Johnson Vision; has received research support from Allergan, Alcon, Avedro, Carl Zeiss Meditec, Johnson & Johnson Vision and Novarits; holds equity in RxSight, Placid0 and VacuSite; and holds patents assigned to VacuSite. Dr. Moshirfar reports no relevant disclosures.
1. VisuMax Femtosecond Laser. Small incision lenticule extraction (SMILE) procedure for the correction of myopia. Professional use information. Accessed Jan. 5, 2023. https://www.accessdata.fda.gov/cdrh_docs/pdf15/P150040D.pdf
2. Fu Y, Yin Y, Wu X, Li Y, Xiang A, Lu Y, Fu Q, Hu T, Du K, Wen D. Clinical outcomes after small-incision lenticule extraction versus femtosecond laser-assisted LASIK for high myopia: A meta-analysis. PLoS One 2021;16:2:e0242059.
3. Blum M, Lauer AS, Kunert KS, Sekundo W. 10-year results of small incision lenticule extraction. J Refract Surg 2019;1:35:10:618-623.
4. Ma KK, Manche EE. Corneal sensitivity and patient-reported dry eye symptoms in a prospective randomized contralateral-eye trial comparing laser in situ keratomileusis and small incision lenticule extraction. Am J Ophthalmol 2022;241:248-253.
5. Moshirfar M, Tukan AN, Bundogji N, Liu HY, McCabe SE, Ronquillo YC, Hoopes PC. Ectasia after corneal refractive surgery: A systematic review. Ophthalmol Ther 2021;10:4:753-776.