NOW THAT MOST REFRACTIVE SURGEONS have become familiar with the epi-LASIK devices on the market and how they work, they want to delve deeper and find out what results they can expect from them. Here's a sampling of the latest outcomes and surgeons' impressions of two of the instruments. Next month's column will cover the remaining epi-LASIK separators.
Barrie Soloway, MD, director of vision correction surgery at the New York Eye and Ear Infirmary, thinks one of the secrets to his success with epi-LASIK is managing the number of drops he uses before surgery.
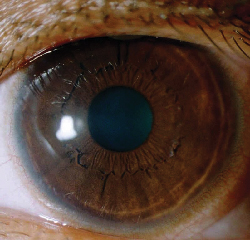 |
| Corneal appearance three days post epi-LASIK with the Moria Epi-K. |
Dr. Soloway says one of the challenges is keeping suction times down, because the separator takes a relatively long time to complete its pass. He uses Genteal drops as the separator is making its pass, and tries to keep the area wet. He begins in position three, the fastest of the device's three speeds, then drops down to the slowest, position one, as soon as the separator meets the epithelium. Dropping to this speed allows him to see the beginning edge of the flap being made. "Once you have that edge," he explains, "advance to position two to slowly go about halfway across the eye. Then, watch for when the separator comes alongside the letter 'I' in 'Epi-K,' which is engraved right in the middle of the suction ring. When you hit that mark, go to position three to speed things up." He says creating the epithelial sheet calls for about 30 to 35 seconds of regular suction.
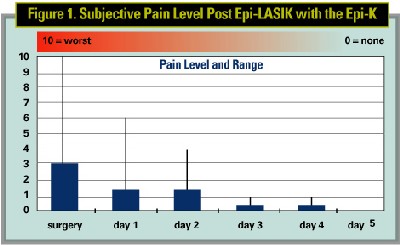
As for results, Dr. Soloway says that, on the first postop day, some patients will have pain in a range from zero to six, with the average being a three (on a 1 to 10 scale from least to most pain). (The acuities at that time are around 20/40. On the second day, he says the pain gets better but the acuities actually dip down to about 20/50. By the third day, he says patients usually recover their vision and most can return to work. Most re-epithelialize by the fourth postop day.
Out of 40 patients in a study performed by Dr. Soloway and Mark Swanson, MD, of Mexico, four eyes improved by one line at three months and three patients' uncorrected vision was a line better than their best-corrected. Their average preop error was -4.5 D, with an average cylinder of -0.84 D. Six months postop, all eyes saw 20/40 or better uncorrected, and 87.5 percent saw 20/20 or better.
Istanbul, Turkey, surgeon Efekan Coskunseven recently completed one-year follow-up on 92 eyes of 49 patients who underwent epi-LASIK with the Centurion SES device, and says he's learned a few things along the way.
"In the first 70 eyes, we marked the epithelium with a standard LASIK marker," he says. "But now I am using a special Pallikaris epi-LASIK marker that's much simpler to manipulate. Also, in the first group of patients, I used a wet sponge to put the flap back, but now I am using a spatula, which causes less epithelial damage."
Dr. Coskunseven subscribes to the thinking that cooling the stromal bed during surgery helps alleviate postop pain.
"In all cases, after the ablation, we use a cold block to cool the ablation area for 15 seconds," he says.
The use of cold blocks was a concept developed by Greek physician and epi-LASIK inventor Ioannis Pallikaris. Users of the blocks believe they increase the comfort level of the patient in the postoperative period.
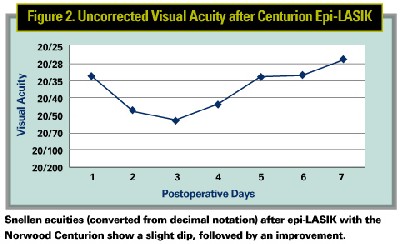
In his study, the average preop refractive error was -3.92 D ±1.64. Postop, it decreased to -0.43 D at one year. The average uncorrected visual acuity went from around 20/150 (0.14 in decimal notation) to nearly 20/20 (0.91 in decimal). And, similar to Dr. Soloway's experience with epi-LASIK, the acuity dips before it increases again.