Once upon a time, ophthalmic surgeons in the
For example, in the most recent survey of U.S. members of the Inter- national Society of Refractive Surgery surgeons, conducted by Richard J. Duffey, MD and David Leaming, MD, less than half of the surgeons responding (46 percent) said they implant phakic IOLs (although the number has gradually increased in recent years). Only 4 percent said they do more than five phakic IOL cases a month. And despite its purported advantage as a treatment for high myopes, only 43 percent of respondents listed it as their preferred option for a 30-year-old -10 D myope. (Notably, phakic IOLs seem to be a much more accepted option in countries outside the
What accounts for this situation? Here, six surgeons from the
Current Phakics: Good Outcomes
An outsider pondering this situation might guess that the reason for the drop in interest in the
Parag A. Majmudar, MD, a partner at Chicago Cornea Consultants and associate professor of ophthalmology at Rush University Medical Center in Chicago, recently co-authored a paper with the Ophthalmic Technology and Assessment Committee for the American Academy of Ophthalmol-ogy, reviewing the history of phakic IOLs and clinical data relating to them.1 "I don't think there's any question that the modern versions of these lenses produce great results," he says. "In fact, if you're careful about patient selection, the results are nothing short of miraculous. I had a patient come in with 30 D of nearsightedness. Be- cause the phakic lenses were only available up to about 20 D, I had to do some PRK in addition to implanting a phakic lens to correct his vision. But before the procedure, his best corrected vision was about 20/60; after we were done, he was about 20/30 uncorrected. It's mind-blowing how much impact this kind of procedure can have."
"I think major progress has been made in the design of phakic refractive lenses in the past five years," says Jorge L. Alio, MD, PhD, professor and chairman of the Department of Ophthalmology at
So: What happened?
"Before phakic IOLs came out, everybody was anxious to use them," observes Asim Piracha, MD, medical director at
for the Artisan/Verisyse lens and is currently participating in the FDA trial for the Veriflex, a foldable version of the Verisyse.) "We needed phakic IOLs for high myopes. Because we didn't have them we were doing refractive lens exchanges, increasing the risk of retinal detachments. Then the Verisyse lens was approved, followed by the ICL. The new lenses got a lot of mainstream media coverage; they were written up in Time magazine twice. But it soon became apparent that only a few surgeons were implanting a lot of ICLs, and not many were implanting a lot of Verisyse lenses. In short, they kind of fizzled out."
Dr. Piracha sees several reasons for this. "One problem is the patient's perspective," he says. "Suppose a patient comes into your office and he's -9 D, with a normal cornea but not enough tissue for LASIK. You tell him he can have PRK or a phakic IOL. The lens implant will provide better vision and a quicker recovery, but it's twice as expensive, the patient has to go to the OR, and it has potential long-term complications. In my experience, patients seldom choose the lens implant. It's a harder sell, not only because of the fear of intraocular surgery, but also because of the cost. I think this is great technology—far more convenient than PRK—but the patient has to accept it.
"A second factor is that excimer laser technology has improved," he continues. "Prior to wavefront-optimized and wavefront-guided treatment, I didn't feel confident doing more than 7 D of myopia correction with the laser. Above that range the quality of vision was poor, the optical zone was small, spherical aberration was high and night vision wasn't good. But with modern excimer lasers, I can treat as high as -12 D and leave many patients with 20/15 uncorrected vision. About 88 percent of these patients end up 20/20 or better, and their quality of vision is fine. PRK has also benefited from mitomycin-C, which largely eliminates the need to worry about haze. That allows us to go up to -11 or -12 D and still feel pretty good about the outcomes.
"Third, phakic IOLs don't currently correct astigmatism," he says. "The Verisyse can provide some astigmatism correction because of the large incision, and you can always add a limbal relaxing incision, but the lens is not treating the astigmatism. So some of these patients need laser vision correction following phakic IOL implantation in order to get a perfect outcome. That means the patient has to undergo two procedures. In contrast, you may be able to treat everything with a single procedure using PRK or LASIK.
"A fourth problem is the surgeon's learning curve," he notes. "My partner and I have a lot of experience with the Verisyse lens, but I seldom implant more than one patient a month. I think a lot of surgeons balk at the prospect of learning a new skill set and dealing with all of these measurements for a procedure they perform a half dozen times a year. And it's difficult to become comfortable with a procedure you rarely perform.
"Last, but not least, surgeons worry about potential long-term complications," he adds. "So there are multiple factors working against the popularity of phakic IOLs."
Additional Concerns
Stephen S. Lane, MD, managing partner at Associated Eye Care and clinical professor of ophthalmology at the University of Minnesota in Minneapolis, sees other problems as well. "The greatest 'wow factor' I have as a refractive surgeon is in my phakic IOL population—more so than from cataract surgery, premium IOLs or LASIK," he notes. "So the potential of these lenses is great. The problem is that, for the moment at least, the use of phakic IOLs has largely been reserved for the patients surgeons aren't comfortable doing LASIK on—mainly the high myopes in the neighborhood of -9 to -10 D and above.
This limits the number of eligible patients." (Dr. Majmudar points out another factor that may be limiting the number of available patients: the possibility that American surgeons may have exhausted the early-adopter population for this procedure.)
In terms of safety, Dr. Lane notes that this is an intraocular procedure. "Although the potential for endoph-thalmitis is very small, it's real," he says. "Also, phakic-IOL-induced cataract is a reported complication and a legitimate concern. Furthermore, American surgeons are concerned about endothelial cell loss. We don't have to be reminded about the previous angle-supported lenses in Europe that were taken off the market as a result of endothelial cell decompensation. That has produced a healthy amount of skepticism on the part of American surgeons."
However, not all surgeons see phakic IOLs as a high-risk option. "I think some surgeons believe that implanting phakic lenses is a dangerous process," says Dr. Alio. "It is not. Many problems in the past related to poor indications or poor lenses. Fortunately, most of the lenses available today have been very well-studied, so there is very little risk to using them."
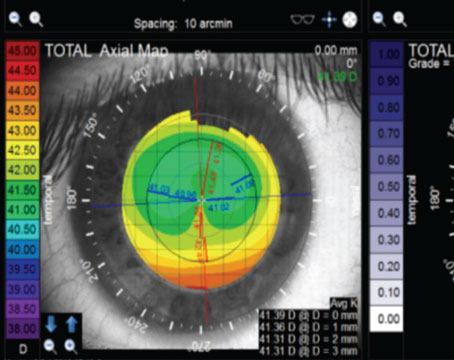
Dr. Alio adds that one problem with phakic IOL use in the past that may have contributed to this "risky" perception was difficulty measuring anatomy. "Accurate measurement used to be a big issue—one of the reasons not to indicate these lenses," he says. "Today we not only have better lenses, we have better measuring capability using tools such as the Visante OCT. We're not making anatomy-related errors the way we did in the past."
Like Dr. Piracha, Dr. Lane sees cost as a significant problem. "Having to do the procedure in an operating suite increases the cost to the patient, and insurance won't pay for these lenses, or the facility fees, or the cost of the procedure," he points out.
"Where a LASIK procedure might cost $2,000 per eye, a phakic IOL could cost $4,000 or more per eye be-cause of the added facility fees. The result of all of these considerations is that when a patient is borderline—say a -7 or -8 D myope or less—the vast majority of refractive surgeons are probably more comfortable recommending LASIK than a phakic IOL."
Dr. Majmudar agrees. "A patient of mine recently canceled a phakic IOL implantation because she had just lost her job," he says. "She was ready, but now she can't afford it. So the current relatively low level of phakic IOL popularity partly reflects the economic downturn."
All of these concerns fly in the face of the theoretical benefits to offering phakic IOLs. "Implanting phakic IOLs avoids corneal issues such as ectasia and dry eye," Dr. Piracha points out. "Recovery is very quick compared to PRK, and in a worst-case scenario the lens can be removed. Plus, we're not changing the corneal shape—the optics of the eye—so someday down the road if the patient gets a cataract he won't have to worry about IOL power calculations, spherical aberration and so forth. But phakic IOLs still have all of those other factors working against them."
The European Perspective
Phakic IOLs are more readily available and have a longer history outside of the United States, which may partly account for their greater popularity in Europe. However, European surgeons have differing perspectives on their current level of use. "Phakic IOLs are being used more and more, at least in my environment," says Dr. Alio.
"Correcting more than 10 or 12 D of myopia with a laser seems unreasonable when we know that a phakic IOL, properly selected and properly indicated for the patient, will produce much better quality of vision. In my practice, I use phakic lenses for myopes needing more than 10 to 12 D of correction, for hyperopes needing more than 6 to 7 D, and for patients with more than 5 to 6 D of astigmatism—especially myopes. Of course, these cases are much less frequent than low refractive errors. I'm also using more phakic lenses in special cases such as keratoconus, and following lamellar or penetrating keratoplasty."
Dr. Alio notes two significant differences between America and Europe that impact usage. "In Europe we don't have so many LASIK centers and clinics for refractive surgery," he says. "They're just not as popular. At the same time, most LASIK centers in the United States don't have the facilities to operate and implant phakic IOLs."
A somewhat different perspective is offered by Georges D. Baikoff, MD, professor of ophthalmology at the Monticelli Clinic in Marseilles, France, and inventor of the Vivarte/GBR phakic IOL. (His experience with phakic IOLs consists largely of anterior chamber implantation using angle-supported or iris-fixated lenses.) "In Europe today, I believe phakic IOLs are less popular than a few years ago," he says. "The femtosecond laser allows us to do very thin LASIK flaps—90 to 100 µm thickness—which increases the indications for myopia treatment. We can therefore treat up to -10 or -12 D on corneas of normal thickness. Moreover, companies are inclined to encourage crystalline lens extraction. As a result, I really don't know what the future is for phakic implants over 10 D. In addition, in Europe medical rules and regulations have, in general, been less restrictive than those set by the FDA, giving us the opportunity to find out the advantages and inconveniences of these lenses. It's possible that with hindsight, this experience has led us to be more selective than before."
In spite of this perceived decline in use, Dr. Baikoff says his own numbers are stable. "Phakic IOLs represent a little less than 10 percent of my total refractive surgery," he notes. "I don't think that has varied a great deal these past few years."
Other factors also appear to be contributing to differences in usage patterns between Europe and the United States. Dr. Majmudar notes that the range of correction considered acceptable changes the size of the eligible population. "In the United States the typical cutoff for switching from laser to phakic IOL is around -10 D," he says. "In Europe, the cutoff seems to be closer to -7 D; they at least consider a phakic IOL for anyone more nearsighted than that. That increases the eligible population significantly."
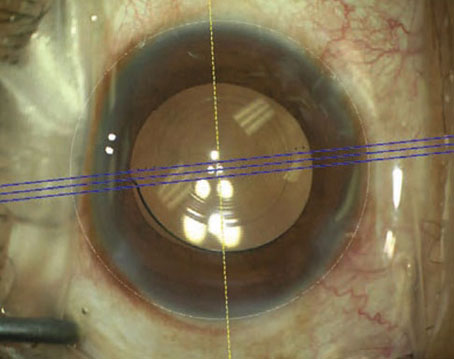
Dr. Piracha, who has extensive experience with the Verisyse lens, notes that there are also differences in lens style preferences between the United States and Europe. "Two out of three surgeons in Europe who implant phakic IOLs are using the Verisyse/Artisan iris-claw lens," he observes. "In the United States, two out of three are using the ICL instead. One reason for this is that with the ICL both implantation and removal are easier.
The Verisyse/Artisan requires bimanual dexterity and a larger incision, so you have to manage the wound and it's possible for the iris to prolapse or the chamber to collapse.
Most surgeons don't do 6-mm incisions or corneal sutures any more. I know of several surgeons who implanted one Verisyse and then stopped; it's just too stressful for some people."
Dr. Majmudar notes another reason for both types of phakic IOLs' limited acceptance in the United States. "The mindset of the American public is a little different than the mindset in Europe," he observes. "The Artisan lens, the equivalent of the Verisyse, has been in use in Europe for almost 20 years, so a whole generation of Europeans has heard about this technology; they're familiar with the results, and have come to accept it the way Americans accept LASIK as a correction for myopia. It took LASIK a number of years to reach its current level of acceptance, and phakic IOLs have only been approved in the United States since 2004. So it makes sense that over time the general public acceptance of phakic IOLs will increase, probably to the levels we see in other countries, once they've been around long enough and most people know someone who's had one implanted."
Will New Approvals Bring Change?
It's not hard to imagine that the likely eventual approval of Alcon's angle-supported Cachet IOL and AMO's Veriflex, the foldable version of the Verisyse, could have a significant impact on the popularity of phakic IOLs in America. In particular, American surgeons seem interested in the Cachet.
"I hope the angle-supported lens works great whenever it's approved," says Dr. Ferguson. "It should avoid most of the concerns I have with the ICL. To the best of my knowledge, you won't need to do a peripheral iridotomy. You won't have to get near the crystalline lens. You'll only have to make a small incision. You can come in from any side you like."
"If Alcon's angle-supported Cachet lens is approved, it will add more tools to the refractive surgeon's toolbox," notes Dr. Lane. "As an angle-supported lens it's relatively easy to place, and it has a shorter learning curve than lenses such as the ICL and Verisyse. Additionally, because of the distance from the crystalline lens, the concern of developing a cataract is minimized. On the other hand, its close proximity to the cornea makes endothelial cell loss a serious potential problem. Surgeons considering it will undoubtedly recall the lenses that were taken off the market in Europe.
"Despite the fact that the Cachet IOL is a very different lens design made of a very different material, it will require some time and education to differentiate the two in surgeons' minds," he adds. "However, Alcon is a major ophthalmic company with a good reputation, and many surgeons have seen the excellent clinical results reported to date. By the time it's approved, the safety of the lens will be well-established. I think there will be increased use of phakic IOLs with this new generation of lenses."
Dr. Piracha shares many surgeons' concerns about these potential problems.
"Colleagues who are involved in the trial of the Alcon angle-supported lens report that they love it, including some who are well-versed in the problems caused by earlier angle-supported lenses," he notes. "Nevertheless, it seems reasonable to expect that putting lens haptics into the angle will lead to some sort of iris, angle and trabecular meshwork problems over time. Previous angle-fixated IOLs had problems with pupil ovalization, glaucoma, pigment dispersion and iris atrophy. I can't imagine such a lens being completely inert and quiet for 10 or 20 years. I have no experience with the Alcon lens, and I don't want to be a naysayer, but if it's approved I'll look very carefully at the FDA data and probably wait a year before trying it. You don't really learn about a lens until after it's approved and everyone is using it."
Dr. Baikoff believes that if the AcrySof Cache IOL produces good results, phakic IOLs could become more popular. "However, I don't believe that anterior chamber phakic IOLs are meant to remain in the anterior segment indefinitely, because of anterior chamber modifications that occur with age—the crystalline lens progressively bulges forward, volume increases, and so forth," he says. "This IOL will require not only meticulous measuring of the anterior segment before implantation but also evaluation of the modifications likely to occur over the years. And, surgeons will need to explain to the patient that after a number of years the implant will have to be removed."
Dr. Alio is a little more optimistic. "Angle-supported lenses have always been more popular, and they are the easiest to implant," he says. "I think phakic IOLs will be used much more frequently once an angle-supported lens is available in the United States."
Dr. Piracha is currently taking part in the FDA trial for the Veriflex, the foldable version of the Verisyse. "If the Veriflex were approved today, I'd be using it in every patient that needs a phakic IOL," he says. "To me, it has all the advantages of the ICL, in terms of small incision and quick recovery, and all the benefits of the Verisyse, in terms of long-term safety and lack of complications. However, I don't know whether that will sway surgeons; it won't change the iris enclavation process, which some surgeons dislike. But, if you want the wow factor while avoiding sutures, then the Veriflex will be a great option."
Despite being hopeful about the potential impact of new phakic options, Dr. Piracha isn't convinced their popularity will soar. "I think more surgeons will offer them," he says. "But it won't change the cost problem, or eliminate patient fears about going to the OR and having surgery inside the eye. It will still be a challenge to get patients to sign up and be excited about it."
How High Can They Fly?
Given the advantages offered by phakic IOLs and their drawbacks—some real, some potential—are these lenses ever likely to achieve widespread popularity, especially in America?
"It takes time for new ideas to become popular," notes Dr. Alio. "Phakic IOLs are not really a new idea, but many surgeons are still in a conservative position or don't have the technology to measure the eye accurately to ensure that the lens will be problem-free. Nevertheless, as important companies such as Alcon enter into this field with backup data from major clinical studies, I believe these lenses will become even more important in refractive surgery."
"With phakic IOLs, the name of the game is safety," says Dr. Lane. "Some of the newer lenses have shown really excellent safety margins in the short term. The question is, how will they fare after 10 or 20 years in the eye? Until that question is answered, I think there will be a certain amount of hesitancy of the part of surgeons to use them. But once sufficient long-term safety info is available, I think you'll see much wider-spread acceptance of these lenses. I don't think anyone questions how efficacious they are; they work well and produce great results. And the wow factor will keep surgeons coming back for more."
"Phakic IOLs are really a great option," agrees Dr. Majmudar. "Yes, the volumes are low. They're a niche product. I don't think phakic IOLs will ever equal LASIK in terms of volume. But in terms of efficacy and safety, they've really come a long way."
Dr. Piracha has been a paid speaker for AMO and Alcon, and Dr. Lane is a consultant for Alcon and Staar; Drs. Majmudar, Piracha and Alio are taking part in current clinical trials of phakic IOLs. However, none of the surgeons interviewed for this article have a financial interest in any of the lenses mentioned.
1. Huang D, Schallhorn SC, Sugar A, Farjo AA, Majmudar PA, Trattler WB, Tanzer DJ. Phakic intraocular lens implantation for the correction of myopia: a report by the American Academy of Ophthalmology. Ophthalmology 2009;116:11:2244-58.