New technologies and techniques coupled with skilled surgeons are making major flap complications a thing of the past. The learning curve for creating a LASIK flap is getting easier with newer techniques and ablation technologies and the implementation of LASIK has become more controllable. While LASIK has become the refractive treatment of choice because it offers patients less discomfort, faster visual rehabilitation and less risk of postoperative haze, the procedure comes with an incidence of certain intraoperative and postoperative complications, including flap complications.1
"Intraoperatively, complications such as button holes, incomplete flaps and penetration of the anterior chamber are extremely rare now," explains Daniel S. Durrie, MD, associate clinical professor at the University of Kansas Medical Center, and in practice at the Hunkeler Eye Institute, Overland Park, Kan. "Epithelial abrasions still occur and postoperative problems, such as slipped flaps, epithelial in-growth, or interface inflammation, occur, although the incidence of all of those has decreased also."
Although the mechanical microkeratome is still the most popular tool utilized for lamellar flap creation, the femtosecond laser is gaining in use and popularity. The IntraLase laser (IntraLase Corp., Irvine, Calif.) uses femtosecond laser pulses to create lamellar flaps.2 Other technologies, such as disposable microkeratomes, and surface ablation techniques such as LASEK and Epi-LASIK are making flaps better than ever. In this article, surgeons share their research and experiences with the incidence of flap complications today.
Disposable Microkeratomes
Michael W. Belin, MD, professor at Albany College, in Albany, N.Y., says there are fewer flap complications in general with a non-automated microkeratome unit because the surgeon has complete control over the excursion of the microkeratome and can stop the travel of the microkeratome before it completes a pass. As a result the incidence of free caps is next to zero, he says. "Also, with a manual microkeratome you have the ability to correct a problem, such as a lash in the way, without having the unit jam," Dr. Belin notes.
Once he made the switch to a disposable microkeratome (which he uses now in the majority of his cases), other complications such as epithelial irregularities were dramatically lower. In Dr. Belin's study of 4,278 consecutive eyes (1,603 eyes—reusable and 2,675 eye-disposable), he compared the incidence of intraoperative epithelial defects during LASIK using the disposable and reusable Moria LSK microkeratomes.
 |
"The disposable Moria LSK One has a significantly lower incidence of epithelial defects compared to the reusable head of the same flap thickness," he says. In the study there were no defects in 97.56 percent of the disposable cases, compared to no defects in 87.8 percent of the reusable cases (See figure 2).
Cost is a consideration when purchasing the disposable unit, which can start at $12,500. Fifty to 60 cases a month is usually a transition point considering turnaround time as well, notes Dr. Belin.
Mechanical Microkeratomes
The Amadeus (Advanced Medical Optics, Santa Ana, Calif.), leaves complete control of oscillation speed [and other parameters] in the hands of the surgeon. From a design standpoint, the Amadeus keratome prevents major flap complications, according to Parag A. Majmudar, MD, assistant professor in the Cornea Service at Rush Medical College, Chicago. The fluted-edged track of keratome prohibits the possibility of an eyelash or some other object catching in the track and causing a loss of suction, which can lead to flap complications.
| Figure 2. | ||
| Defects (%) | No Defects (%) | |
| Total | 277 (6.5) | 4001 (93.5) |
| Reusable | 208 (13.0) | 1395 (87.8) |
| Disposable | 67 (2.5) | 2608 (97.56) |
| p value < 0.001 | ||
Dr. Majmudar adds that surgeons need to know their microkeratomes, evaluate their results and switch microkeratomes if they are not pleased. "Today most microkeratomes function well and flap complications in general are rare, but they still do occur," he says.
Dr. Durrie notes that he primarily used the Hanastome since 1998 and found it extremely safe. "I have reported on research of over 13,000 consecutive cases without a any major complications, such as buttonholes, incomplete flaps or cancelled cases," he says.
However, Dr. Durrie has switched to the femtosecond laser. He recently conducted a study comparing the quality of vision with the Hansatome and the IntraLase. In the study of 102 eyes, there were no flap complications in either the Hansatome or the IntraLase group. Both sets of eyes received Alcon's Custom Cornea.
"With custom ablation, we're moving into the era of quality of vision, which is going beyond 20/20 and trying to get best correct vision improvement. In addition to reducing or eliminating flap complications we may also be able to improve vision," Dr. Durrie says.
The study showed a higher percentage of patients who had uncorrected visual acuity at 20/20 and better with the IntraLase. It also demonstrated the IntraLase was more accurate and more predictable and there were more patients who gained lines of best correct visual acuity than the Hansatome group. However, Dr. Durrie notes that both groups of eyes did well from a safety standpoint. "Today we may not be looking at the laser flap just for safety; it may be a better way to make the flap for the custom ablation era we are now in," he adds.
He says after the one-month study date that the IntraLase is a promising platform for not only predictability and safety but also with the next goal of the microkeratome, which is to possibly help in the vision correction process.
Once the three-month data is analyzed a better picture will develop on contrast sensitivity and patient preference. Additional prospective multicenter studies are also needed to validate the results, he says.
Perry S. Binder, MD, associate clinical professor in the department of Ophthalmology at the University of California, San Diego, also supports the IntraLase technology. After using various microkeratomes, such as the ACS (B&L), and the SKBM (Alcon, Fort Worth, Texas) in more than 5,000 cases as well as the Moira M2 (Moria, Doylestown, Pa.), and the BD 4000 (Becton Dickinson and Co., Waltham, Mass.), Dr. Binder switched to the IntraLase femtosecond laser in June 2000 and has used it for more than 850 cases.
He says he has not had any flap complications, such as button holes, epithelial defects, decentered flaps, irregular flaps, microstriae, excessively large hinges or flap diameter or thickness surprises, with the IntraLase and cites predictability of flap thickness as well as safety as two main advantages.
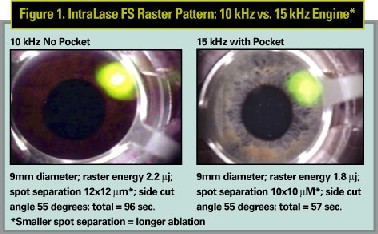
In a study on flap dimensions and clinical outcomes with the IntraLase laser using the 10- and 15-kHz laser engines (See Figure 1), Dr. Binder reports that flap predictability was superior and flap creation was safer with the IntraLase than with mechanical microkeratomes. "The 15-kHz IntraLase engine reduces time from 96 seconds to 57 seconds or less for a 9.0-mm diameter flap and the 15-kHz flap lifts easier than the 10-kHz flap," he says.
IntraLase does, however, have its detractors. First, it's more expensive than mechanical microkeratomes. "The laser costs more, even with large volumes. However, the added cost must be balanced against the safety issues for patients," counters Dr. Binder.
In addition, the surgery takes longer and the flap can be more difficult to lift with the femtosecond laser. Dr. Binder acknowledges that surgeons may have some difficulty until they become more experienced with the technology. Flap elevators are now available from several manufacturers, such as Rhein Medical (Tampa, Fla.), and Katena (Denville, N.J.), which aid the process.
Finally a patient's vision is not as good immediately postop (off the table) for the IntraLase as with mechanical microkeratomes, but Dr. Binder contends that first day postop vision is statistically the same or better than mechanical microkeratomes.
Caution is still called for, say some surgeons. Seth A. Biser, MD, and colleagues recently reported a case in which a 43-year-old woman underwent bilateral simultaneous LASIK in which the femtosecond laser was used to create the corneal flap. Postoperatively, the patient noted significantly decreased visual acuity, glare and haloes. She was diagnosed with corneal flap striae, which were treated unsuccessfully with a lifting and stretching procedure, but responded to subsequent bilateral flap suturing.3
"Despite its increased accuracy in flap creation, visually disabling flap folds can develop after the use of the femtosecond laser," Dr. Biser says.
The investigators note that although the intraoperative complications associated with the creation of the LASIK flap, including free caps and buttonholes, may be diminished with the femtosecond laser technology, the case illustrates that postop flap complication still can exist with flaps created with the femtosecond laser.
They concluded that appropriate caution should be taken in the intraoperative and postoperative treatment of patients undergoing LASIK with the femtosecond laser, and patients should be advised that laser-only LASIK is not risk-free.
Surface Ablation
The increasing incidence of reported iatrogenic ectasia, the evolution of wavefront aberrometry, and the suggestion that the LASIK flap could lead to unpredictable biomechanical corneal changes have sparked renewed interest in surface ablation and have lead to the introduction of alternative photorefractive treatment modalities, such as LASEK and Epi-LASIK.4
In LASEK (laser-assisted subepithelial keratectomy) laser ablation is performed under a hinged epithelial flap. Proponents of the LASEK technique say that advantages of the technique include the absence of stromal flap complications and greater choice in patient selection.
"The theoretical advantage of surface procedures, such as LASEK that preserve the epithelial button, stems from the repositioning of the epithelial flap over the laser-ablated corneal surface," explains Ioannis Pallikaris, MD, PhD, professor of ophthalmology at the University of Crete, Greece, who developed the Epi-LASIK procedure. "This epithelial sheet is thought to act as a natural contact lens that decreases postoperative pain and haze formation."
Epi-LASIK [Epipolis laser in situ keratomileusis], an alternative method of epithelial separation done with a device that features a blunt oscillating blade, doesn't require the use of alcohol for epithelial loosening as in LASEK or PRK.
Initial results of studies of EPI-LASIK, which uses the Centurion SES EpiEdge epikeratome from CIBA Surgical for Sub-epithelial Separation, indicate that many flap complications of LASIK will be reduced, Dr. Pallikaris says.
Because alcohol is toxic to epithelial cells, removing the alcohol application from the procedure results in faster healing and less pain for patients, he adds. The procedure's use of a mechanical, instead of alcohol-assisted, separation of the epithelium allows for a "no cut" epithelial separation.
In addition, the separation takes place under the basement membrane, thus preserving its integrity. Histological studies have shown that the epithelial basement membrane remained intact, basal epithelial cells showed no irregularities and the procedure did not adversely affect hemidesmosomes.5
Fewer Complications, Better Vision
The desire to have fewer complications coupled with better visual quality in a wavefront ablation era is pushing the envelope and helping create new technologies and techniques to meet these goals, according to leading refractive surgeons.
Dr. Durrie notes that while mechanical microkeratome and femtosecond laser eyes seem to be performing well from a safety standpoint, surgeons need to look to the future and consider laser flaps as possibly providing higher quality of vision as well.
1. von Kulajta P, Stark WJ, O'Brien TP. Management of flap striae. Int. Ophthalmol Clin 2000; 40:87-92.
2,3. Biser SA, Bloom AH, Donnenfeld ED, Perry HD, Solomon R, Doshi S. Flap Folds after Femtosecond Laser. Eye & Contact Lens 2003;Vol. 29(4):252-254.
4. Pallikaris IG, Katsanevaki VJ, Kalyvianaki MI, Naoumidi II. Advances in subepithelial excimer refractive surgery techniques: Epi-LASIK Curr Opin Ophthalmol; 2003 Aug 14,(4):207-12.
5. Pallikaris IG, Naoumidi II, Kalyvianaki MI, Katsanevaki VJ. Epi-LASIK: comparative histological evaluation of mechanical and alcohol-assisted epithelial separation. J Cataract Refract Surg 2003;29(8):1496-501.