With the late May Food and Drug Administration approval of Visx's CustomVue technology for refractive surgery, wavefront has once again captured the attention of the media and refractive surgery patients. Researchers and users say that wavefront clearly yields some benefit in visual outcomes, though the approved ranges are still fairly narrow, and bringing wavefront into clinical practice is no small feat.
This article will review recent studies on the benefits of wavefront and some of the lessons that early users have learned about the technology.
Trial Data
With the decision, Visx joins Alcon as the only U.S. manufacturers with approved wavefront systems. The approved indications are for the treatment of myopia up to -6 D, with up to 3.0 D of astigmatism.
The Visx multicenter clinical trials that served as the basis for approval included 351 eyes of 189 patients with mean age of 36 ± 8 years. The mean preop refractive error was sphere -3.6 D ± 1.4, cylinder +0.7 D ± 0.7. All eyes received bilateral LASIK, with an 8-mm ablation zone and were targeted for emmetropia. There was no nomogram adjustment.
 |
| In the Visx system, a PreVue lens is ablated with the patient's expected treatment. |
One of the major benefits of wavefront is the reported decreased level of higher order aberrations that may be induced by conventional LASIK. The Visx trial also looked at improvement in higher order terms at six months and showed the percentage of wavefront patients who experienced a decrease (or an increase on less than 0.1 µm), for coma (71 percent), trefoil (92 percent) and spherical aberration (76 percent).
No study subject lost more than one line of BSCVA at six months; 3 percent lost one line; and 64 percent of eyes experienced a gain in BSCVA from baseline. There were eight adverse events reported: two eyes experienced an epithelial defect; five developed diffuse lamellar keratitis, and all seven of these events resolved without a loss of BSCVA; and one eye experienced a partial LASIK flap.
A Better Mousetrap
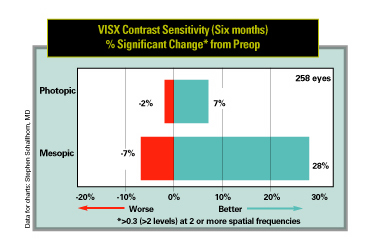
A major potential selling point of wavefront is the decrease in the level of surgically induced higher-order aberrations that contribute to nighttime vision complaints. To assess the actual effect of wavefront-guided treatment, San Diego surgeon Stephen Schallhorn gathered data on wavefront treatments from the FDA submissions of the three U.S. manufacturers and independently analyzed the results and compared them with data on his own conventional LASIK cases. The latter was based on 430 subjects, 856 eyes, on multiple laser platforms.
 |
In low-contrast settings, the results suffer. On a 5-percent contrast, logarithmically based chart, the same patient base shows that 17 percent experience a loss of two or more lines of vision, and 3 percent experience an increase of that magnitude.
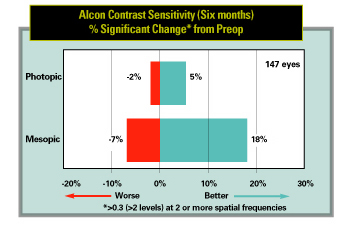 |
Alcon data, using a refined algorithm, was based on 147 eyes of 74 subjects with a -3.0 D ± 1.16 MSE preop, that improved to -0.2 D ± 0.34 at six months with 90 percent seeing 20/20 or better. Once again, more than twice as many patients displayed improved contrast sensitivity results following custom treatment than those with poorer results.
Bausch & Lomb data (340 eyes of 190 patients showing 92 percent at 20/20 after six months) also showed similar improvement, though using a different type of contrast sensitivity chart.
Dr. Schallhorn finds the consistency of the results both "amazing" and very positive for the industry. "This is definitely a step up in technology; it's a better mousetrap," he says. "It's not just one laser company saying, 'we have the secrets, we have a lock.' It's different companies going different routes and winding up almost in the same place as far as improvement. It speaks very powerfully, to me, that wavefront-guided treatment is a better technology. It's good news for everybody."
In Practice
Los Angeles surgeon Andrew Caster, MD, uses Alcon's LADARVision system with the company's CustomCornea wavefront. He has performed wavefront-guided surgery on about 200 eyes of commercial patients. What he's learned, he says, is that wavefront "is not cook book. The machine is not doing everything; there are surgeon decisions and techniques that are very important in achieving the best results. People need to study this and pay attention to the details if they want to get consistently good results." He estimates the learning curve at about 100 patients.
One clinical observation Dr. Caster has made is that wavefront-treated eyes take a bit longer to stabilize. "At the one-week visit, I'm finding that the non-wavefront eyes are seeing better than the wavefront eyes," says Dr. Caster. "But by the one month visit, most of the wavefront eyes are seeing better than the non-wavefront eyes." He suspects that the greater complexity of the wavefront pattern may be the reason.
He also places great emphasis on assessing the tear film before wavefront-guided treatment. "We assess the tear film with fluorescein prior to performing the surgical wavefront treatment," he says. "You have to be careful not to disturb the tear film or the epithelium while you're marking the eye or while you're actually taking the wavefront measurements, which can take some time. A lot of drying or epithelial irregularities will degrade your wavefront measurements and lead to a less than perfect result. The testing can take some minutes and you have to make sure that the patient is blinking consistently throughout that time."
Another important factor is registration. "The alignment is extremely critical," he says. "The dots you make on the eye have to be small, round and dark enough that they're going to last the required amount of time. You need to align the treatment on the LADARVision laser in the exact same way that you align them on the LADARWave machine. Any imprecision in that registration will lead to a less than ideal result. The more aberrated the eye is, the more important that registration is. That's why I personally find it difficult to understand how any system that is not using some type of electronic alignment can possibly achieve comparable results. Even using the electronic alignment, it's difficult."
Houston surgeon Douglas D. Koch, MD, an investigator for the Visx wavefront system, agrees that registration is essential. "All of these patients will benefit by being marked at the slit lamp so that if there is any ocular rotation on the table, that can be recognized and adjusted for in the treatment," says Dr. Koch.
He strongly recommend that surgeons stick to what's been tested. "We did not use nomogram adjustment in the trials, but it is certainly possible that people will require nomogram adjustments," says Dr. Koch. "The clinical trials were conducted under very strict environmental conditions and if people don't match that, then it is possible that they will encounter over- or undercorrections in their particular laser setting. And you really have to be sure to stick with the requirement that the wavefront data not deviate any more than is recommended from the manifest refraction, so that outliers are eliminated before you get started."
Dilate or Don't?
Barrie Soloway, MD, of New York City, has been using the Alcon system since January and has performed about 100 wavefront-guided procedures. He stresses the role of the quality of the input. "What might be problematic on almost any wavefront device is opacities in the media, or severe surface changes, where it's difficult to get a good wavefront. The tear film and the whole optical system need to be very clear. Patients with mild cataracts or even dry eye, people who are not getting a good tear film, can end up giving problems in terms of getting good information. The quality of the information is important."
Dr. Soloway sees clear benefit in performing the wavefront measurement through a dilated pupil. "You're only getting information through the pupil, so the size of the pupil is a key.
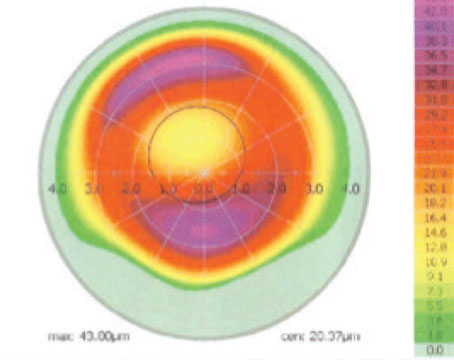
He presented data at ASCRS on a study of 100 eyes looking at their higher order aberrations at different pupil sizes. "We looked at the same patient at 8 mm, 7.5, etc., going in half-millimeter steps down to a 5-mm diameter. We found a significant difference in the amount of higher-order aberrations that we were measuring. If we looked at 8 mm scan diameters as a percent of aberrations so that we could standardize everybody's numbers together, at 7.5 we were measuring 74 percent of the aberrations; at 7 mm, 57 percent; at 6, 33 percent; at 4.5 mm, 9 percent."
Dr. Koch, however, prefers not to induce dilation. "I would be concerned about pharmacologic dilation because of the potential for moving the center of the pupil," he says. "And it's so critical that centration be preserved from measurement to treatment that by capturing patients who are dilated just in a natural state in a dim room, you're more likely to have perfect registration of the centration of the treatment.
He sees the proof in the clinical trial data. "The Visx numbers are so good and patient complaints about difficulty of seeing to drive at night or seeing at night with glare actually diminished in patients treated in the Visx study. And more than half of the patients had pupil sizes that were bigger than 6 mm. So I think that if you get a beautifully positioned 6-mm treatment and then blend that out to the periphery, you're going to do a great job covering these patients."
Avoid the Hype
Surgeons agree that, until much more research is done, one thing that needs to be carefully controlled is patient expectations.
Dr. Schallhorn, who is transitioning to wavefront in his practice, says, "I tell patients that I think the quality of vision—in terms of night vision, glare, halos—is better. How much? A little. I say, 'You may have a 4 percent chance of having significant night halos or glare at night with conventional surgery; with wavefront you may have a 2 percent chance.' In a normal population of virgin eyes, we don't find any predictive value as to who will do better with wavefront based on their higher-order aberrations prior to surgery. Patient A with low higher-order aberrations is just as likely to benefit from wavefront as patient B, with lots of preop higher-order aberrations. The only predictive value is the level of preop myopia. Patients with higher levels of preop myopia, within the approved range, might do better with wavefront because they're the ones with more induced aberrations. The higher the myopia, the more the induced aberrations."
Adds Dr. Koch, "You have to really couch your statements that wavefront correction offers you the possibility of better quality vision, more accurate correction than standard LASIK. If patients come in thinking this is going to be super vision, with the implicit sense that there is some guarantee, that will really create a lot of negative backlash."
| Improving on Zernike |
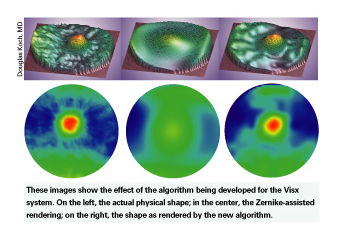 |
| One of the longtime staples of the relatively young wavefront technology has been Zernike polynomials. These mathematical terms, born of research in astronomy and optics, served to describe the shape of the wavefront in an aberrated optical system. One problem with them however has been the tendency to drop data, that not all of the data are used. "When you have a fair amount of optical irregularity," says Douglas Koch, MD, a Visx investigator and professor of ophthalmology at Baylor College of Medicine's Cullen Eye Institute, "Zernike polynomials, by the way they're constructed, create a smoothing effect in the interpretation of those data, so that you lose a lot of the detail in the irregularity or abnormality. You start with 200 or so data points with the WaveScan system and a 6-mm pupil, and then you have to have some way of interpreting the data, the way that the light from those 200 lenslets is refracted to recreate the wavefront. Zernikes appear to do a good reconstruction for normal eyes, but in eyes with more irregular astigmatism, it's becoming evident that Zernikes give a little bit of an incomplete picture." Visx is developing new software that will go beyond Zernike polynomials, intended to reduce the "smoothing" of data that contributes to data loss. "As we try to extend the applications of wavefront to better treatments of patients with irregular astigmatism, such as those with corneal grafts or complications of prior refractive surgery, new algorithms will provide a greater level of fidelity in interpreting the lenslet data," says Dr. Koch. "This will help us create a treatment plan that is much more detailed and truly reflects the actual underlying pathology. It tremendously reduces the smoothing associated with Zernikes." |