In the past, if you were a vitreoretinal surgeon looking for the best method for repairing a retinal detachment, the search for definitive data was frustrating, since most surgeons seemed to have a method that worked great for them but might not be reproducible by everyone else. Recently, however, the landmark Primary Retinal Detachment Outcomes (PRO) Study cut through a lot of the anecdotal noise and provided truly useful insights on such topics as the true value of scleral buckles in a surgical area dominated by vitrectomies (it turns out buckles are still very useful) and the results of detachment repair in phakic vs. pseudophakic eyes (the study found that one surgical method in particular is best for one of these groups).
To learn about all of the valuable data we’ve gleaned from this study that you can put to use in your practice, read on.
Differing Approaches
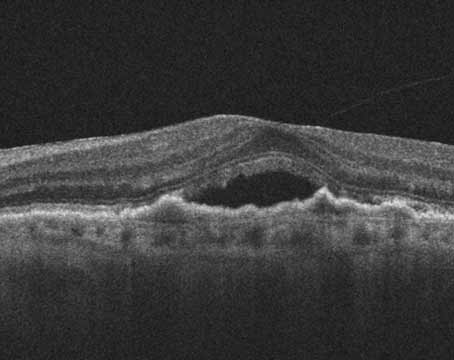
During the past 50 years, the preferred surgical method for repair of primary rhegmatogenous retinal detachment has shifted from scleral buckles to pars plana vitrectomy, or combination PPV/SB. In 1980, PPV accounted for only 1 percent of all RRD surgeries, but by 2014 this percentage reached 83 percent.1,2
The surgical approach for RRD differs amongst retina specialists; many will choose either SB, PPV or PPV/SB for the same anatomic presentation of RRD based upon their experience, preoperative factors and evidence in the literature. Specifically, many preoperative factors like the location and extent of retinal detachment, the patient’s lens status, the location and number of breaks, and personal experience lead to the surgical plan, but there is still a lack of consensus among surgeons regarding the best approach.3 This discord is due to the difficulty in accounting for the many variables in surgical studies, such as draining of subretinal fluid, shaving of the vitreous base, preferred tamponade agent and the best amount of endolaser, among others.
 |
Studies Lend Help
Though numerous studies have attempted to analyze surgical outcomes for RRD repair, the Scleral Buckling versus Primary Vitrectomy in Rhegmatogenous Retinal Detachment (SPR) study was perhaps the first and most important report on outcomes of various surgical approaches to RRDs. The SPR was a randomized, prospective clinical trial published in 2007 that showed the superiority of SB to PPV in visual acuity outcomes in phakic patients. The study also concluded that PPV was superior to SB in terms of anatomic outcomes for pseudophakic patients.4,5 This study, though, was carried out in the early 2000s before the widespread use of small-gauge vitrectomy and enhanced visualization systems, so more up-to-date studies are warranted. Also, it wasn’t designed to compare PPV to PPV/SB.
This leads us to the Primary Retinal Detachment Outcomes study, in which we compiled a large, comprehensive, observational dataset from all patients at six centers who underwent primary RRD repair in 2015. Sixty-one vitreoretinal surgeons participated in the study, and the study centers spanned the United States, and consisted of:
• VitreoRetinal Surgery in Minneapolis;
• The Retina Center in Minneapolis;
• The Retina Institute in St. Louis;
• Mid Atlantic Retina/Wills Eye Hospital in Philadelphia;
• Associated Retinal Consultants in Royal Oak, Michigan, and;
• Massachusetts Eye and Ear Infirmary in Boston.
The PRO study group investigated the outcomes of RRD surgeries as no other series had done before. The study analyzed more than 250 pre-, intra- and postoperative metrics, attempting to identify any difference in surgical outcomes based on these metrics. The surgeons analyzed only primary rhegmatogenous retinal detachments that had not undergone previous attempts at surgical repair and excluded complicated retinal detachments such as those in the setting of penetrating injury, proliferative diabetic retinopathy, sickle cell disease, retinopathy of prematurity, familial exudative vitreoretinopathy or ischemic vein occlusion, acute retinal necrosis and prior endophthalmitis. All in all, nearly 3,000 eyes recorded in the database had primary RRD repair with either SB, PPV, PPV/SB, laser retinopexy, cryopexy or pneumatic retinopexy.
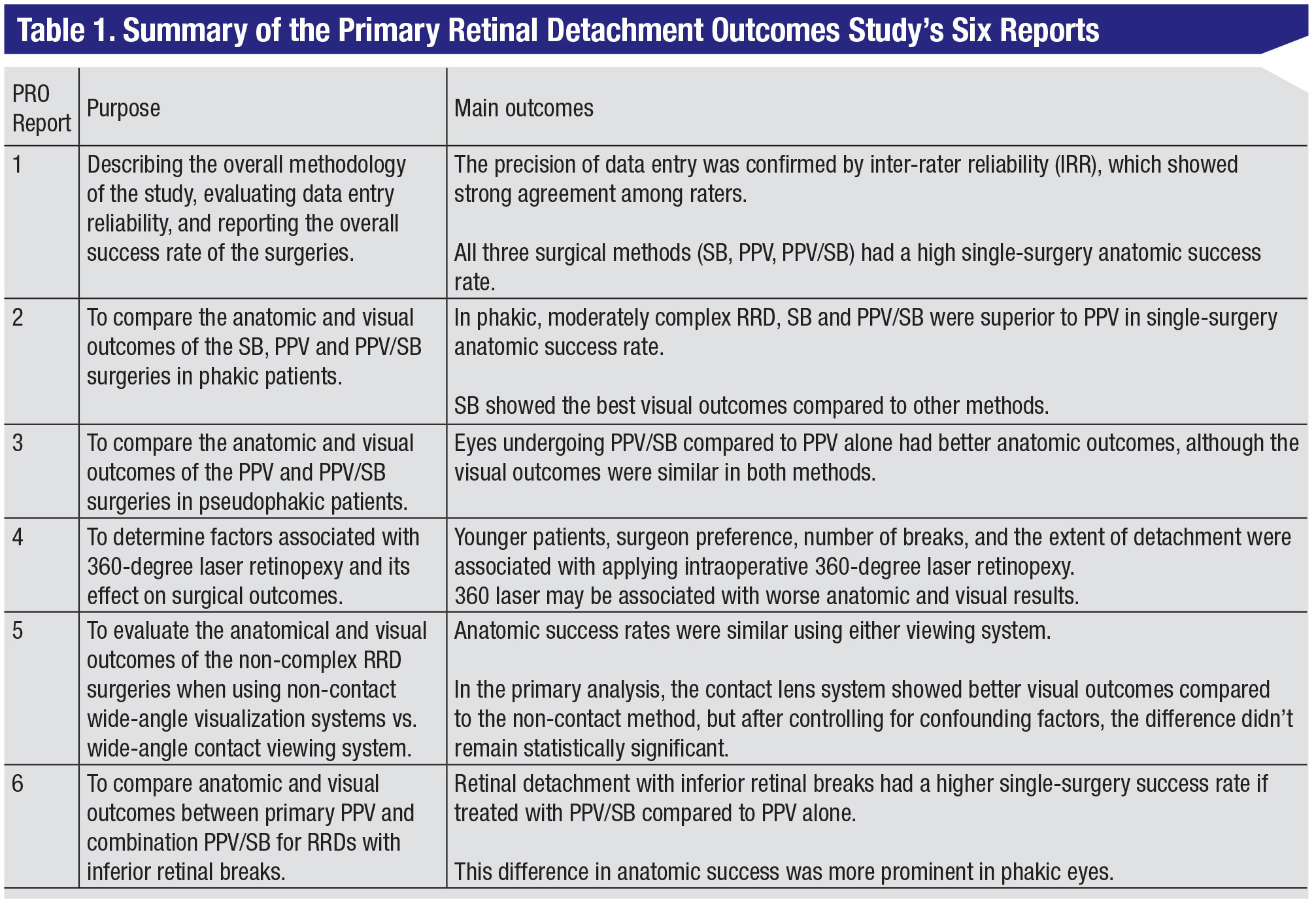
To date, six publications have stemmed from the PRO database, with numerous other manuscripts either in-press or submitted to well-known ophthalmology journals.6,7(p2),8–11 The results of all six published papers are summarized in Table 1. Here’s a look at each PRO study report and the unique insights it brought to vitreoretinal surgeons.
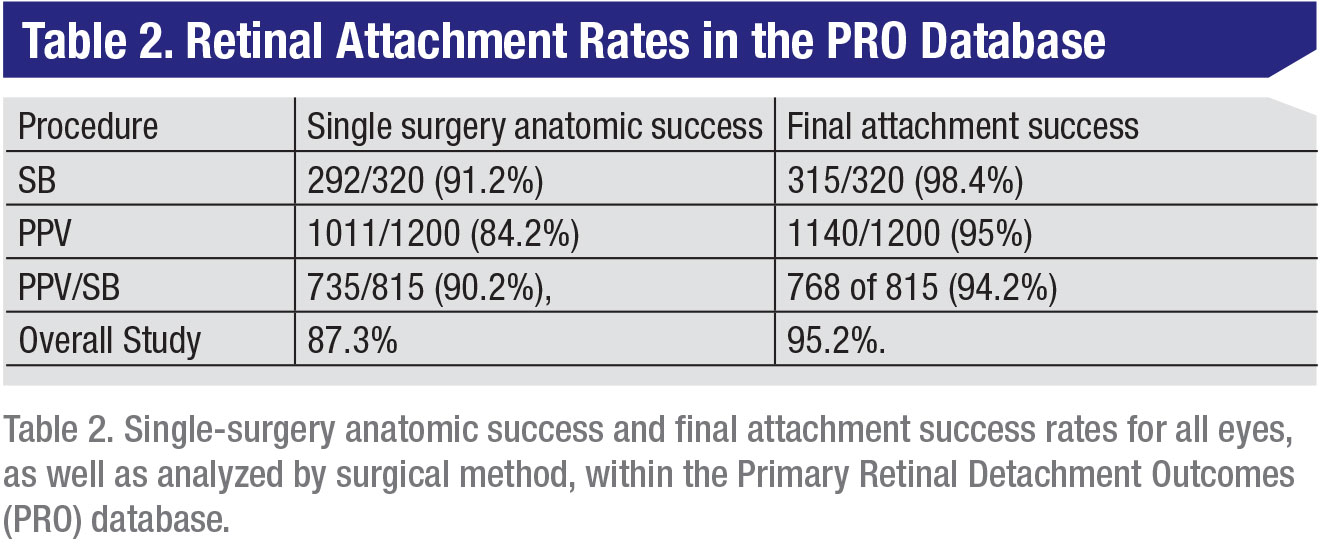
• Report #1—Methodology. This was first a methodology paper, but also highlighted overall non-comparative outcomes.6(p1) First, regardless of the surgical approach, the overall success rate was high for primary RRD repair. Second, more than half of the patients in this study were managed with primary PPV; primary SB was used in 13.5 percent of the cases, and 40.2 percent of the cases were managed with combination PPV/SB. These data underscore the importance of scleral buckling in the management of phakic retinal detachment. Lastly, this study analyzed data reliability using an inter-rater reliability (IRR) calculation factoring in 15 key variables to determine the consistency of data entry. The paper concluded there was a high degree of agreement in reliability of observations, giving reassurance that the data are trustworthy.
• Report #2—Phakic outcomes. The second PRO report focused on the visual and anatomic outcomes of phakic patients who underwent primary repair of RRD with PPV, SB or PPV/SB.7(p2) For these patients, SB was superior to PPV in both anatomic and visual outcomes, and PPV/SB was superior to PPV in anatomic outcomes. These results again highlight the importance of scleral buckling and the need to continue to educate future trainees on the intricacies of proper buckling techniques. Certainly, as a fellow I can appreciate the buckle training I’m receiving here at Wills Eye and know how important these buckles are to achieving anatomic and visual success. Even in the modern era of small-gauge PPV and enhanced wide-angle viewing systems, the results of the PRO study validate the continued use of scleral buckles in the management of RRDs.
• Report #3—Pseudophakic outcomes. The third PRO report focused solely on pseudophakic eyes undergoing either PPV or PPV/SB.8(p3) SB wasn’t analyzed separately, as only five pseudophakic eyes in the dataset underwent SB. This subset was composed of nearly 1,000 eyes, with 77 percent of the RRDs treated with PPV, and the remainder with PPV/SB. Patients undergoing combination PPV/SB were more likely to have inferior RRDs. This study again showed superior anatomic outcomes for PPV/SB versus primary PPV, but with no statistical differences in final visual outcomes between the cohorts.
• Report #4—Surgical metrics. Perhaps the greatest strength of the PRO database is the robust number of individual metrics collected for each surgery, which speaks to the effort of the hard-working researchers involved in the data-collection process. The first PRO paper to focus on the subset of metrics was PRO report number 4.9(p4) The aim of this study was to assess outcomes in eyes that underwent intraoperative 360-degree laser retinopexy during repair of primary RRD with primary PPV or combination PPV/SB. Ultimately, 516 of 2,248 (23 percent) eyes underwent 360-degree laser retinopexy. Younger age, more retinal breaks, more extensive RRD and surgeon preference were significantly associated with the use of this procedure. However, when controlling for case complexity, intraoperative 360-degree laser retinopexy was significantly associated with lower final anatomic success and worse final visual acuity. Certainly these results are interesting and perhaps highlight the superior outcomes of a more targeted laser retinopexy during surgery. Within our practices, the choice of approach seems to be surgeon-dependent and is a question that will continue to be debated.
• Report #5—Contact vs. non-contact lens viewing systems. The fifth PRO report again used the vast metrics within the dataset to focus on outcomes of vitrectomies done with a contact versus a non-contact wide-angle lens during primary RRD repair.10
In this cohort, 363 eyes were treated using the contact lens system and 1,893 eyes treated with the non-contact viewing system. The initial analysis showed better final visual outcomes for the contact lens cohort, but after controlling for confounding factors, the difference didn’t remain statistically significant. An analysis of anatomic outcomes showed no differences in single-surgery success or final anatomic success between the two viewing systems.
• Report #6—Inferior retinal pathology and scleral buckles. The sixth published manuscript answered the question of whether it’s necessary to add a scleral buckle when repairing RRDs with inferior retinal pathology.11 Compared to previous papers on this topic that were more lenient in their grading of inferior pathology, the PRO manuscript only included eyes with retinal breaks found between the 5- and 7-o’clock meridians. The study included 238 eyes with inferior pathology and excluded primary scleral buckles. Ninety-five eyes (40 percent) underwent primary PPV and 163 (60 percent) that underwent combined PPV/SB. Combination PPV/SB had superior anatomic outcomes compared to primary vitrectomy, which remained significant when accounting for other preoperative metrics that may affect success, such as macula status, number of breaks, lens status, extent of detachment and surgeon factor. Subgroup analysis also showed that phakic eyes undergoing PPV/SB had superior single-surgery success rates.
 |
Looking Ahead
The Primary Retinal Detachment Outcomes Study is a landmark database in vitreoretinal surgery. The use of a multicenter, multiple-surgeon, longitudinal analysis of outcomes of the repair of primary rhegmatogenous retinal detachments over a single calendar year gives the vitreoretinal community incredibly valuable insights. In particular, in the era of increasing use of small-gauge PPV for RRD repair, the PRO database reveals the continued usefulness of both primary and adjunctive sceral buckling for improved anatomic and visual success, and underscores the added value of scleral buckles for the repair of primary rhegmatogenous retinal detachments. It’s imperative that the next generation of vitreoretinal surgeons understands the nuances of proper scleral buckling technique given the outcomes identified in the PRO database, especially in phakic patients.
Moving forward, there are several other key projects coming from the PRO database that are analyzing various metrics within the rich dataset. Many reports are in press, specifically manuscripts focusing on the use of prophylactic ILM peeling during primary RRD repair, and repair of primary RRDs with concomitant, non-causal macular holes, as well as outcomes in younger and older patients with primary RRDs. These papers and others that delve into the different surgical approaches that lead to improved outcomes are on the horizon.
In the final analysis, the PRO database has been an excellent resource for retrospective cohort studies comparing multiple surgeons’ approaches to the repair of many different types of primary RRDs with a variety of anatomic nuances. There will always be debate on how to best approach a particular surgical problem, and many surgeons can achieve the same outcome using vastly different approaches. The database highlights these different approaches, and in the era of increasing use of vitrectomy for the repair of primary RRD the study’s outcomes remind us all of the continued importance of scleral buckles.
The database also allows critical examination of the various approaches the study’s surgeons used to repair RRDs, and makes the results generalizable to the greater vitreoretinal surgery community. Even so, it remains difficult to design the perfect study of RRD treatment, given the inherent limitations of any research analyzing heterodox surgical techniques and methods; each patient and surgical encounter is unique and requires a precise surgical plan. The PRO reports remain very useful for physicians, however, and we hope that this review of these and future PRO manuscripts will help guide vitreoretinal surgeons moving forward. REVIEW
Dr. Starr is a surgical retina fellow in the retina service at Wills Eye Hospital/Mid Atlantic Retina in Philadelphia. Dr. Salabati is a research fellow in the retina service at Wills Eye Hospital/Mid Atlantic Retina in Philadelphia. Dr. Ryan is an associate clinical professor of ophthalmology in the University of Minnesota Department of Ophthalmology.
1. Minihan M, Tanner V, Williamson TH. Primary rhegmatogenous retinal detachment: 20 years of change. Br J Ophthalmol 2001;85:5:546-548.
2. McLaughlin MD, Hwang JC. Trends in vitreoretinal procedures for Medicare beneficiaries, 2000 to 2014. Ophthalmology 2017;124:5:667-673.
3. Schwartz SG, Flynn HW. Primary retinal detachment: Scleral buckle or pars plana vitrectomy? Curr Opin Ophthalmol 2006;17:3:245-250.
4. Feltgen N, Heimann H, Hoerauf H, et al. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment study (SPR study): Risk assessment of anatomical outcome. SPR study report no. 7. Acta Ophthalmol (Copenh) 2013;91:3:282-287.
5. Heussen N, Hilgers R-D, Heimann H, Collins L, Grisanti S, SPR study group. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment study (SPR study): Multiple-event analysis of risk factors for reoperations. SPR Study report
no. 4. Acta Ophthalmol (Copenh) 2011;89:7:622-628.
6. Ryan EH, Joseph DP, Ryan CM, et al. Primary Retinal Detachment Outcomes Study (PRO Study): Methodology and overall outcomes—PRO study report #1. Ophthalmol Retina. Published online March 4, 2020. doi:10.1016/j.oret.2020.02.014
7. Ryan EH, Ryan CM, Forbes NJ, et al. Primary Retinal Detachment Outcomes Study (PRO Study): Phakic retinal detachment outcomes—PRO study report #2. Ophthalmology 2020;127:8:1077-1085.
8. Joseph DP, Ryan EH, Ryan CM, et al. Primary Retinal Detachment Outcomes Study: Pseudophakic retinal detachment outcomes: PRO study report #3. Ophthalmology. Published online May 8, 2020. doi:10.1016/j.ophtha.2020.05.005
9. Wang JC, Ryan EH, Ryan C, et al. Factors associated with the use of 360-degree laser retinopexy during primary vitrectomy with or without scleral buckle for rhegmatogenous retinal detachment and impact on surgical outcomes (PRO study report number 4). Retina. Published online December 23, 2019. doi:10.1097/IAE.0000000000002728
10. Tieger MG, Rodriguez M, Wang JC, et al. Impact of contact versus non-contact wide-angle viewing systems on outcomes of primary retinal detachment repair (PRO study report number 5). Br J Ophthalmol. Published online May 14, 2020. doi:10.1136/bjophthalmol-2020-315948
11. Starr MR, Obeid A, Ryan EH, et al. Retinal detachment with inferior retinal breaks: Primary vitrectomy versus vitrectomy with scleral buckle (PRO Study Report No. 6). Retina. Published online July 13, 2020. doi: 10.1097/IAE.0000000000002917