 |
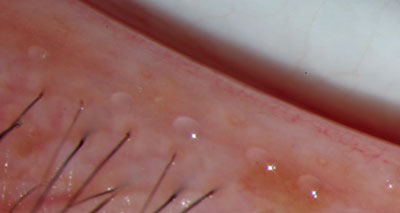
| Meibomian gland lipid content (sebum) spills out of the acini at the mucocutaneous lid junction to coat the ocular surface. The lipid then becomes the smooth film meibum on the surface. Ophthalmic Research Associates |
Meibomian glands are a type of sebaceous gland located in the tarsal plate of the upper and lower eyelids. They are distinguished by grape-like clusters of acini on the mucocutaneous lid junction, and empty their lipid content (sebum) at this junction in order to coat the ocular surface via holocrine breakdown. Meibomian glands are anchored by cells that produce both polar and nonpolar lipids, which are then stored in lysosomes that merge into larger storage granules.1 As these cells continue to enlarge with lipid, they eventually rupture into the meibomian gland opening and spill the sebum over the ocular surface. These lipids are liquid at room temperature with a normal melting point of between 66 and 89 F, and are distributed over the ocular surface in a thin, smooth film called meibum. This meibum functions to prevent evaporation of the aqueous layer.
It's important to understand the mechanism of secretion for this layer of tear film, as the inadequate release of meibum often leads to disorders such as dry eye, blepharitis, sties and chalazia.
Symptoms of meibomian gland dysfunction are similar to severe dry eye in that patients often report that their eyelids feel as though they're stuck together in the morning, feel a foreign body sensation and have blurred vision after performing near tasks. Patients may also report excessive tearing and intolerance to contact lenses.2
In a normal patient, meibomian gland orifices are open and visible as small gray rings on the posterior lid margin. In patients with meibomian gland dysfunction, however, the gland orifices are often compromised due to stenosis or closure. This may be attributed to an increase not only in the lipid melting point, but also in the tear-film osmolarity due to an increase in aqueous evaporation or an increase in viscosity of the sebum, which compromises delivery to the marginal reservoirs.
The marginal reservoirs provide a barrier to tear overspill and contamination by skin lipids, which may destabilize the tear film. Without a continuous flow into these reservoirs, the distribution of the meibomian secretion that spreads with each blink is compromised and can lead to the clinical presentation of evaporative dry eye and blepharitis. For this reason, it's important for clinicians to determine the functionality of the orifices and the quality of secretions onto the ocular surface.
An easy test of the functionality of the orifices and the quality of secretions is to express meibum either by applying gentle pressure with a fingertip or by using a cotton-tipped applicator. Normal eyes will produce a clear, thin oil, while eyes with orifice stenosis will produce a thicker oil that may appear cloudy. In advanced meibomian gland dysfunction, the orifice can be completely obstructed, preventing secretion of any oil at all. In such cases, closure of the orifice may be due to chronic inflammatory conditions of the lids, such as blepharitis.
Blepharitis
About half of all patients with blepharitis tend to see their ophthalmologists for dry-eye symptoms such as burning, stinging or other ocular discomfort.
Posterior blepharitis has been associated with meibomian gland dysfunction, which is classified by high lipid viscosity and low lipid volume, often creating an operculum over the gland. Clinicians may notice debris or scales along the lash line, a greasy coating on the lashes themselves, hyperemia or even missing or broken lashes.
Further indications of blepharitis include inflammation and irregular lid margins.3 Inflammation disrupts the wiper blade function of the eyelids, often leaving dry areas on the ocular surface, which can cause damage to epithelial cells. Some studies have indicated that most, if not all patients presenting with signs and symptoms of blepharitis have underlying meibomian gland dysfunction.4
If your patient has blepharitis, it's important to analyze the quality and quantity of his meibomian secretions. Poor secretions should be treated by lid hygiene and massaged with a moist cotton tip in order to remove debris from the eye and increase blood flow so as to open up occluded meibomian glands.5 Warm compresses will also unblock the glands, as a higher compress temperature will liquefy viscous meibum.
Blepharitis often occurs alongside acne rosacea. Rosacea is another chronic inflammatory disorder that affects the midline facial skin and causes the development of fine telangiectasias, which suggests chronic lid margin inflammation and recurrent inflammatory papules and pustules.1
Approximately 58 percent of people with acne rosacea experience ocular symptoms of the disease, such as chronic blepharitis, chronic low-grade conjunctivitis and tear-film instability.
Just as with blepharitis, the first line of treatment and prevention for the ocular symptoms of rosacea is proper lid hygiene using lid scrubs, hypoallergenic bar soap or baby shampoo. One eyelid cleanser, OCuSOFT (Austin Medical Technologies), is available in the form of solution, foam pump and pre-moistened pads. Advanced Vision Research recently introduced a new option in lid scrubs in the form of a premixed, pre-diluted foam cleanser called SteriLid. This is an antibacterial lid foam designed specifically to treat the conditions blepharitis and dry eye.
Glandular Infection
While posterior blepharitis is directly linked to obstructed meibomian glands, anterior blepharitis has been thought to be the result of bacterial infection, which leads to lid margin inflammation. Other ocular conditions associated with bacterial infection include hordeolum, or sty. A sty is caused by an infected meibomian gland, most often due to blockage caused by the bacteria Staphylococcus aureus, resulting in acute inflammation of the eyelid. The hordeolum will generally drain spontaneously within five to seven days, though the pus can be expelled manually by nicking the occluded orifice and then applying pressure to the area.
Chalazia are also related to meibomian gland infection, and may actually develop from a hordeolum. By definition, a chalazion is a mass of infected tissue that develops around a blocked meibomian gland. Inflammation associated with this disorder may cause lid edema, which may poke through the skin anteriorly or into the subconjunctival-tarsal space where it may spontaneously drain or exist as a chronically inflamed granuloma.1 Treatment for chronic chalazia may rarely require surgical drainage.
Glandular Control
Meibum secretion over the ocular surface is hypothesized to be neuronally and hormonally controlled. Neuronal control is thought to be attributed to vasoactive intestinal polypeptide (VIP), a neurotransmitter that is present in meibomian gland nerves that are in direct contact with the acinar cells, as well as in the main lacrimal gland.6-8
A type of sebaceous gland, meibomian glands are characterized by androgen receptors, so it's hypothesized that these glands are under hormonal control. This point is particularly noteworthy because there is a significantly increased prevalence of meibomian gland dysfunction in post-menopausal women. Androgens act on the acinar epithelial cells, which contain receptor messenger RNA and/or androgen receptor protein.9 These cells respond to androgens by binding the androgen to a specific lipid-producing area on the cell, which then transcribes specified genes to increase the lipid layer distribution over the ocular surface.9 On the contrary, an orchiectomy or a topical anti-androgen treatment causes a significant decrease in the ocular lipid profile. The administration of sex hormones, such as the androgen precursor dehydroepiandrosterone, to the surface of the eye has been found to stimulate meibomian gland lipid production and release and prolong the eye's tear-film breakup time.10
Future Treatment
Perhaps the future of treating meibomian gland dysfunction lies in targeting the hormone receptors on the meibomian glands rather than treating disorders when they become symptomatic, particularly those that result from underlying dysfunction, such as chalazia, sties and blepharitis. Until this type of treatment is readily available however, clinicians should be sure to take a close look at the meibomian glands of patients presenting symptoms of evaporative dry eye, lid margin inflammatory disorders and bacterial infection that cause surrounding lid-margin inflammation. For these patients, thorough lid hygiene, massage, warm compresses and possible steroid/antibiotic treatment can't be stressed enough, as these measures may prevent ocular surface disorders associated with meibomian gland dysfunction.
Dr. Abelson, an associate clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at Schepens Eye Research Institute, consults in ophthalmic pharmaceuticals.
Ms. Oberoi is a research associate at ORA Clinical Research & Development in North Andover.
1 Bajart AM. Lid inflammations. In: Albert DM, Jakobiec FA, eds. Principles and Practice of Ophthalmology. Philadelphia: WB Saunders Company 2000;829-47.
2 Nichols JJ, Ziegler C, Mitchell GL, Nichols KK. Self-reported dry eye disease across refractive modalities. Invest Ophthalmol Vis Sci 2005;46:6:1911-4.
3 Abelson MB, Reynolds O. Are you missing these common eyelid disorders? Skin and Aging 1998;2:6:48-53.
4 Mathers WD, Choi D. Cluster analysis of patients with ocular surface disease, blepharitis, and dry eye. Arch Ophthalmol 2004;122:11:1700-1704.
5 Bowman RW, Dougherty JM, McCulley JP. Chronic blepharitis and dry eyes. Int Ophthalmol Clin 1987;27:27.
6 McCulley JP, Shine WE. Meibomian gland function and the tear lipid layer. Oc Surf 2003;1:3:97-106.
7 McCulley JP, Shine WE. The lipid layer of tears: dependent on meibomian gland function. Exp Eye Res 2004;78:361-5.
8 Dartt DA, Sullivan DA. Wetting of the ocular surface. In: Albert DM, Jakobiec FA, eds. Principles and Practice of Ophthalmology. Philadelphia: WB Saunders Co.;2000:900-81.
9 Sullivan DA, Sullivan BD, Evans JE. Androgen deficiency, meibomian gland dysfunction, and evaporative dry eye. Ann New York Academy Sciences 2002;966:211-222.
10 Zelligs MA, Gordon K. Dehydroepiandosterone therapy for the treatment of dry eye disorders. Int Patent Application WO 94/04155. 1994.



