Although the United States Food and Drug Administration has so far only approved limited uses for topography-guided LASIK—a technology that makes it possible to minimize or eliminate aberrations on the corneal surface—U.S. surgeons do have access to the technology. Available platforms include Alcon’s Contoura Vision, which uses the Wavelight Topolyzer VARIO diagnostic device, proprietary treatment-planning software and either the Allegretto Wave Eye-Q or WaveLight EX500 Excimer Laser systems; NIDEK’s EC-5000 Advanced Vision Excimer laser system (NAVEX), comprising the Quest M2/EC-5000CX, OPD-Scan III and Final Fit custom ablation software; and Johnson & Johnson Vision’s iDESIGN Refractive Studio, which measures wavefront analysis and corneal topography and then combines them to generate a custom LASIK procedure for each patient.
The potential advantages of eliminating corneal aberrations are easy to understand, but the technology itself can be complex. Furthermore, today’s non-topography-guided laser-ablation technology has become very sophisticated, leading many surgeons to wonder whether offering topography-guided ablation is worth the learning curve required to master it—not to mention the time and effort required to use it on each patient. Here, surgeons with extensive experience using this approach share their opinions regarding its pros and cons.
Topo-guided LASIK: The Upside
Surgeons who’ve used topography-guided technology agree that it can produce remarkable outcomes. However, they disagree about how many patients stand to benefit from this, as well as the value of this technology when its use is limited by the FDA.
A. John Kanellopoulos, MD, clinical professor of ophthalmology at NYU Medical School and medical director of the Laservision.gr Institute in Athens, Greece, has had extensive experience with topography-guided LASIK. “We’ve routinely used this technology in our clinical practice for more than 10 years now, to treat both myopia and hyperopia,” he says. “We’ve also published extensively on this topic, discussing our work with what we call topography-modified refraction, or TMR. We use this approach nearly 100 percent of the time, as long as the topographies we obtain are consistent and accurate.
“Our results using this approach are the best we’ve ever seen,” he continues. “Almost 75 percent of these patients are achieving 20/16 visual acuities, and 20 percent of them achieve 20/10. These are numbers we’ve never seen with any laser refractive procedure in the past, and many other clinicians have now reproduced these data. I think that most people who become familiar with this platform will see the tremendous potential that it offers, even in virgin eyes. And of course it’s an effective alternative for treating eyes that have had previous laser vision correction, or even radial keratotomy, although these uses are still off-label in the United States.”
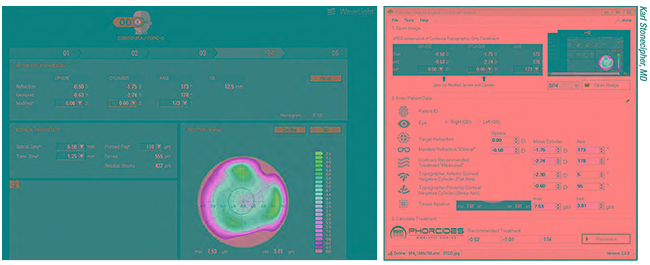  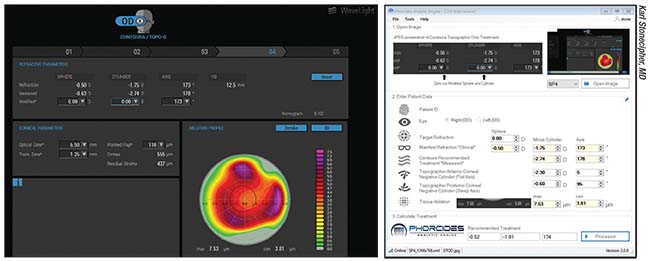 |
| One challenge surgeons using topography-guided ablation often face is conflicting astigmatism measurements—amount and/or axis—from topography and the manifest refraction. Above left: A patient whose amount of astigmatism on topography differs substantially from the manifest refraction. Above right: Phorcides software uses vector analysis and mathematics to suggest treatments in these challenging cases. Beta surgeons are currently using this software in a controlled fashion to determine the best option for these patients. |
Karl Stonecipher, MD, medical director for TLC Laser Eye Centers in Greensboro, North Carolina, and clinical associate professor of ophthalmology at the University of North Carolina, says his practice tries to use topography-guided LASIK on as many patients as possible. “This technology has increased our word-of-mouth referrals,” he says. “These patients see exceptionally well, and they notice the difference. In a recent study we published, we found a significant increase in 20/15-or-better vision favoring topography-guided LASIK over wavefront optimized.1 This technology gives us the best opportunity to make patients see better than they did previously with glasses or contact lenses.
“However,” he adds, “we’re limited by the current range of approval, so when treating patients who don’t fall within the topography-guided approved specs we do wavefront-optimized LASIK. We may also elect to do wavefront-optimized treatment in patients with thinner corneas, because that allows us to spare tissue and preserve corneal integrity.”
Dr. Kanellopoulos points out that how often you choose to use topography-guided LASIK on your patients depends partly on how high your bar is set for visual outcomes. “Most laser platforms today offer wavefront-optimized LASIK,” he says. “That technology produces excellent results, and most patients achieve 20/20. If your aim is simply to get your patients to 20/20, topography-guided LASIK may not impress you, as it requires more preoperative work and planning. This technology becomes pivotal, in my opinion, if you’re trying to pursue the best possible correction of the patient with the fewest possible future re-treatments. As a side effect, you also gain a better understanding of the patient’s optical and visual function.”
Dr. Kanellopoulos says that his experience supports the idea that any patient with repeatable topography readings can benefit from topography-guided LASIK. “If the patient has consistent topographies—meaning the epithelium is relatively untouched and the corneal topography maps are consistent—he stands to benefit considerably from this approach,” Dr. Kanellopoulos says. “The reason for this is that most patients actually have more astigmatism than you measure in the refraction. The slightest amount of angle kappa, i.e., more that 100 µm on the x and/or y axis, means that the eye is not seeing through the center of the astigmatic ‘bow tie,’ but slightly off-center. This causes refractive coma, so the correction the patient chooses is compensating for both the refractive error and the functional corneal coma. Topography-guided treatment can minimize or eliminate this coma.
“I think every potential patient who seeks laser vision correction is a good candidate for topography-guided LASIK or topography-guided PRK,” he concludes. “I believe trying this on a few patients will let any clinician see the superiority of this approach. In our experience, the only patients that don’t benefit from a topography-guided approach are patients who don’t have consistent topographies, meaning they don’t have four or five topographies that are very similar. In that situation, any data you choose to base the treatment upon may not be valid.”
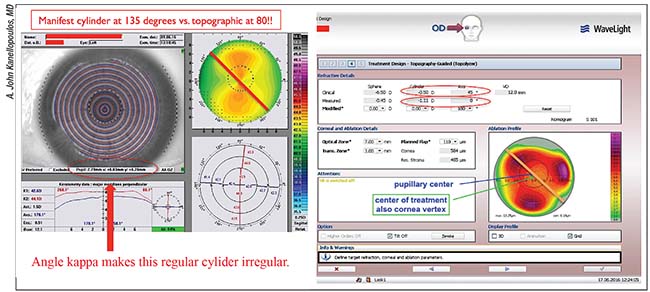 |
| Angle kappa can cause a discrepancy between the cylinder measured by topography and clinical refraction. In the case above, there is significant angle kappa in the y-axis. The topography software measures -1.11 D of cylinder (measured line) at 180 degrees. In contrast, the clinical refraction finds -0.5 D of cylinder at 45 degrees. Adjusting the topography-guided ablation software to zero refractive correction shows that the software is attempting to normalize the cornea in regard to the cornea apex, in a trefoil pattern reminiscent of vertical coma. A possible explanation for the discrepancy in cylinder is that the patient himself “refracts” this corneal coma as cylinder, thus reducing and shifting the axis of the topographic cylinder found in the clinical refraction. The topography-modified refraction here will change the cylinder from -0.5 to -1 D and the axis from 45 to 0 degrees. The sphere will then be reduced from -6.5 D to -6.25 D to maintain the same spherical equivalent. |
A More Conservative Approach
William I. Bond, MD, FACS, medical director at Bond Eye Associates in Peoria, Illinois, and an assistant clinical professor at the University of Illinois Medical School, was a principal investigator in the original trial that resulted in LASIK being approved in the United States, as well as an investigator in the original topography-guided LASIK trials. He says that, given the current approval status, he doesn’t use topography-guided LASIK too often. “I’d hoped it would be available for treating irregular corneas,” he says. “Since wavefront-optimized technology is so robust for most corneas, and it’s a little time-consuming to evaluate the topography, I don’t use it very often. Using this technology requires having a technician who is very well-versed in getting the topographic data. There are some techniques and tricks for accomplishing this, and the manufacturers can help you with that. But most patients have very regular corneas that are easily treated without it. We probably only use it for 3 to 5 percent of our cases.
“However, if you can get good topographic images, you can do a very good job for people,” he says. “Although I don’t have the data to prove it, it’s been my clinical experience that we get a much higher rate of 20/15 and 20/10 outcomes when we do use the technology. And of course, it will be wonderful for treating patients with irregular corneas. Those are patients we’ve been waiting for years to help. This technology can make a person very happy who would otherwise be borderline-happy.”
Dan Z. Reinstein, MD, adjunct professor of ophthalmology at Columbia University Medical Center in New York City and medical director at the London Vision Clinic in the United Kingdom, says he uses topography-guided treatments primarily only for therapeutic refractive surgery—i.e., to correct topographic irregular astigmatism (currently off-label in the United States). He says he wholeheartedly believes that every surgeon should have access to a topography-guided system, as well as a phototherapeutic keratectomy option, to use for therapeutic re-treatments.
“In an editorial in the Journal of Refractive Surgery,2 I argued that laser manufactures should be mandated to include—and the FDA should facilitate the inclusion of—topography-guided software as a standard option, rather than as an expensive add-on,” he says. “This would allow the few patients who suffer from visual disturbances to be treated. Topography-guided treatment, together with trans-epithelial PTK, provides the surgeon with the toolbox to improve overall patient outcomes, but most importantly, it enables the surgeon to help the rare but real patients who sustain visual complications.”
| Topography and Spherical Refraction |
| “A common mistake that surgeons new to this technology make is thinking that topography-guided treatment will give them the perfect outcome when combined with the clinical refraction,” notes A. John Kanellopoulos, MD, clinical professor of ophthalmology at NYU Medical School and medical director of the Laservision.gr Institute in Athens, Greece. “If there’s a significant amount of topographic correction, the refractive outcome will change. It won’t be what you’d expect if you had treated using wavefront-optimized technology. This is certainly true when correcting astigmatism; when we change the amount of astigmatism, an appropriate adjustment needs to be made to the spherical equivalent. If we decrease the astigmatism by a diopter, we’ll need to adjust the spherical correction to take this into account.” Dr. Kanellopoulos points out that the clinician can see the amount of change that will be created by the topography-guided treatment by looking at the ablation plan with the amount of sphere and cylinder set to zero. “This will clearly show what the laser is going to do for that specific cornea in order to normalize it,” he says. “This will allow the clinician to adjust the spherical correction accordingly. If a clinician finds this type of adjustment daunting, it’s probably best to treat using a more familiar technology such as a wavefront-optimized procedure. If that patient has a problem in the future, you can refer the patient to an expert in topography-guided treatments to address it.” —CK |
However, Dr. Reinstein says he doesn’t believe that topography-guided software should be marketed as being essential for the treatment of virgin eyes. “In my experience, about 95 percent of virgin eyes will derive little or no benefit from this technology because there’s very little irregularity in a normal cornea,” he says. “It could have a measurable benefit in some cases, but in other cases it could be detrimental. Most patients that do have ocular aberrations have neurally adapted to them, so they don’t experience loss of contrast or night-vision problems as a result of the nascent corneal aberrations. In addition, a major study done in 2001 showed that in virgin, unoperated eyes, the first surface of the cornea and internal optics partially compensate for each other’s aberrations to produce an improved retinal image.3 Treating corneal coma, for example, could actually unmask lenticular coma. It’s not always beneficial to remove corneal aberrations.”
Obtaining Good-Quality Data
As with any refractive surgery, basing your treatment plan on accurate measurements—and astute analysis of the data—is crucial. These strategies will help when you’re gearing up for topography-guided surgery:
• Don’t start doing treatments until you’ve done your homework. “The best advice I can give to a surgeon who’s new to topography-guided treatments is that you absolutely must do a comprehensive corneal evaluation of the patient before planning your treatment, including epithelial thickness mapping,” says Dr. Reinstein. “Furthermore, be sure to consult with experienced colleagues and your laser-applications team on as many cases as it takes to be comfortable planning the treatment yourself.
“Optimizing the refractive outcome can be challenging, for several reasons,” he continues. “For one thing, a manifest refraction only uses lower-order aberrations—i.e., sphere and cylinder—so higher-order aberrations such as coma and secondary astigmatism can be mistakenly interpreted as increased refractive cylinder. Much work is currently being done to understand how to optimally combine the manifest refraction and the corneal astigmatism/aberrations. Another source of refractive inaccuracy is the asymmetric epithelial remodeling that occurs following a custom ablation as the epithelium remodels to fit the new stromal surface. Taking the time to learn from surgeons who have experience with this technology, and then doing a thorough, comprehensive exam, can prevent refractive surprises.”
• Give patients a full suite of testing before using topography-guided LASIK. “To determine who would benefit from a topography-guided procedure you should perform topography, tomography, wavefront (corneal and whole-eye), and epithelial thickness mapping,” recommends Dr. Reinstein. “Because of the possible interaction of corneal and lenticular aberrations, it’s important to evaluate all of the aberrations of the eye’s optical system. In addition, the epithelial thickness map is crucial for understanding the stromal surface; that’s the only way to identify patients for whom a topography-guided treatment would be less effective.”
Dr. Stonecipher says that his technicians do all of the standard testing for laser vision correction when evaluating patients for topography-guided LASIK. “That includes screening for ocular surface disease,” he notes. “In addition, we do VARIO analysis using the WaveLight Topolyzer system, and we incorporate the Phorcides integration software created by Mark Lobanoff, MD. Phorcides is our current preferred software for choosing a treatment in these patients. It uses mathematical algorithms to fine-tune our treatment plan, and it appears to eliminate a lot of the ‘art’ of using this technology.”
Dr. Kanellopoulos says that when collecting the data, a careful refraction—and a careful analysis of that refraction—is a good start. “We use subjective measurements before and after cycloplegia, and a wavefront analyzer that takes additional refractive measurements,” he explains. “We also take axial length measurements with interferometry in order to correlate the length of the eye and corneal curvature with the manifest refraction. Careful topographic measurement of the eyes with an instrument such as Alcon’s WaveLight platform using the VARIO placido disc Topolyzer, will reveal the exact amount of corneal astigmatism and let the clinician know how consistent and reproducible the topographies are.”
• Make sure you’ve obtained a high-quality topography scan. “The topography scan is the most important part of the treatment, as this data defines the ablation made to the cornea,” notes Dr. Reinstein. To ensure that the data is good:
— Be sure the cornea is healthy before obtaining topographic data. “Contact lens warpage and ocular surface disease must be eliminated prior to analyzing the patients with the VARIO device,” says Dr. Stonecipher. “Fortunately, diagnosis and treatment of ocular surface disease is becoming more mainstream. Just make sure that the patient understands the reasons for eliminating their contact lens use prior to surgery.”
— Check that the scans were properly focused and well centered, i.e., that the patient was looking at the target. “Centration is crucial,” Dr. Reinstein notes.
— Confirm that the mires are smooth and regular. “It they’re irregular, use lubricating drops and repeat the exam,” says Dr. Reinstein.
— Perform multiple scans to satisfy yourself that any irregularity you’re treating is repeatable. “The ablation algorithm cannot differentiate between a true irregularity and an artifact in the data,” Dr. Reinstein points out.
— Select the scan that has the largest area of continuous data. “Pay particular attention to the superior region,” says Dr. Reinstein. “Data acquisition in that area is often limited by the eyelid.”
Adjusting the Ablation Profile
Dr. Reinstein notes that once the topography scan you’ve chosen has been imported into the laser and an ablation profile has been generated, you may need to make adjustments to different aspects of the profile. In that situation:
• Confirm that the ablation profile makes sense with respect to the diagnostic scans. “In other words, be sure that the ablation is being done where it should be,” says Dr. Reinstein. “For example, pay careful attention to steep areas on placido topography. These are generally assumed to represent an elevation, but they can sometimes actually be a depression. It’s possible for the algorithm to misinterpret these, so this data must be cross-checked with elevation-based tomography.”
| “Be sure the ablation is being done where it should be .... Steep areas on placido topography are generally assumed to represent an elevation, but they can sometimes actually be a depression.” — Dan Reinstein, MD |
• Check the centration. “This is the most important part of the ablation profile calculation,” says Dr. Reinstein. “The placido topography scan, and most tomography scans, are centered on the corneal vertex, and the ablation profile has been generated centered on the corneal vertex. So, the ablation should be performed on the corneal vertex. Some systems have the corneal vertex location integrated into the ablation profile, but if not, the surgeon should manually center the ablation on the coaxially sighted corneal light reflex. It should not be centered on the entrance pupil unless the topography and tomography data are also centered on the entrance pupil.”
• Optimize the optical zone. “Because one of the goals of a topography-guided treatment is to optimize the optical zone, you’ll usually want to treat a large optical zone,” Dr. Reinstein says. “However, if you’re treating a patient [off-label] who’s had previous refractive surgery, a smaller optical zone may need to be used due to tissue constraints. In that situation, the best way to determine 3-D flap anatomy and residual stromal tissue reserves is with very high frequency (VHF) digital ultrasound scanning. As a second alternative, taking point measurements here and there is possible with most corneal-designed OCT devices.”
• If necessary, adjust the refraction. “The manifest refraction can be entered to simultaneously treat an expected residual prescription, although sometimes this is limited by tissue constraints,” explains Dr. Reinstein. “Most systems include an algorithm to take into account the refractive effect of the planned change in topography. Nevertheless, you may still experience refractive surprises. This is largely due to fact that the epithelial thickness profile is not currently taken into account.”
• Consider the depth of the ablation. “Outside of the United States, many therapeutic patients have had multiple procedures,” notes Dr. Reinstein. “As a result, there may be limited tissue available. Some systems allow the ablation profile to be shifted down, so that the total ablation depth is smaller, but some irregularities in the profile may still remain.”
• Consider an off-label PTK. “Some systems allow a PTK ablation to be performed as part of the same procedure [off-label], so that these can be done as a single ablation,” says Dr. Reinstein. “For example, a trans-epithelial PTK ablation can be performed to target irregularities masked by the epithelium, while the topography-guided ablation targets those detectable on topography.”
Dr. Kanellopoulos adds one other consideration: It’s important to compare the topographic and refraction-based astigmatic data. “The corneal and refractive astigmatic data may not be identical,” he explains. “In that situation, if you’re using topography-guided LASIK, you can decide whether to blend the corneal and clinical refraction data, modifying the treatment amount and axis of astigmatism based on the topographic data. (See example, p. 26.) On rare occasions you may find that you also need to account for posterior corneal astigmatism, but this is seldom an issue.”
A Caveat …
Dr. Reinstein notes one other point that he’s learned over the years, relating to the currently off-label use of this technology to treat abnormal and post-refractive-surgery eyes (something many American surgeons are eager to try). “Don’t use this technology to try to correct irregularly irregular astigmatism, such as localized, focal irregularity on the stromal surface,” he says. “If you’re using topography-guided treatments to address an eye with astigmatism, it works best for regularly irregular astigmatism. That would include enlarging a small optical zone or recentering a decentered optical zone. These patients experience a significant improvement in visual quality from a topography-guided retreatment.4,5
“The reason for this distinction is that the epithelium acts to compensate for irregularities on the stromal surface,” he explains. “This is driven by the curvature gradient of the stromal surface, so when the irregularities are localized, the amount of masking is greater.6-8 In these cases the majority of the stromal irregularity is hidden from front-surface topography. As a result, performing a topography-guided treatment will be minimally effective, and may actually make the patient worse.9 For this reason, getting an epithelial thickness map is crucial for understanding the stromal surface. It’s the only way of identifying patients in whom a topography-guided treatment would be less effective.”
A Challenge Worth Accepting
Dr. Kanellopoulos points out that there are plenty of opportunities to get help mastering topography-guided ablation. “Maximizing vision with this technology can be complicated,” he says. “I’ve had the honor of chairing and working alongside several other world-recognized topography-guided surgery ‘aficionados’ to offer courses on this subject just prior to all of the major meetings in the past three years. In these courses we spend a full eight hours going through sample cases step-by-step, helping clinicians become familiar with all of the parameters involved in using this technology and allowing them to design treatments on their own. In addition to those courses, I would invite anybody who is interested in this to visit the pertinent website topo-guided.com.”
Dr. Bond says he hopes surgeons won’t be afraid to use this technology. “It’s a little more time-consuming to do the evaluations, but once that’s done it’s pretty rewarding,” he says. “You’ll get some word-of-mouth and you’ll be known as the guy who can do this type of treatment. Patients always expect to be happy and do well, and that’s not a problem when treating the easy patients. However, getting good vision for some patients is a different world. That’s where this technology can really help.” REVIEW
Dr. Kanellopoulos is a consultant for WaveLight, Alcon, iOptics and Avedro. Dr. Bond is a consultant to Alcon Laboratories and WaveLight. Dr. Stonecipher is a consultant for Alcon. Dr. Reinstein is a consultant to Carl Zeiss Meditec and has a financial interest in ArcScan, producer of the Insight 100, a VHF digital ultrasound scanner.
1. Stonecipher K, Parrish J, Stonecipher M. Comparing wavefront-optimized, wavefront-guided and topography-guided laser vision correction: clinical outcomes using an objective decision tree. Curr Opin Ophthalmol 2018;29:4:277–285.
2. Reinstein DZ. Therapeutic refractive surgery: State of technology and a call to action. J Refract Surg. 2018;34:294-295.
3. Artal P, Guirao A, Berrio E, Williams DR. Compensation of corneal aberrations by the internal optics in the human eye. J Vis. 2001;1:1-8.
4. Reinstein DZ, Archer TJ, Carp GI, Stuart AJ, Rowe EL, Nesbit A, Moore T. Incidence and outcomes of optical zone enlargement and recentration after previous myopic LASIK by topography-guided custom ablation. J Refract Surg. 2018;34:121-130.
5. Reinstein DZ, Archer TJ, Gobbe M. Combined corneal topography and corneal wavefront data in the treatment of corneal irregularity and refractive error in LASIK or PRK using the Carl Zeiss Meditec MEL80 and CRS Master. J Refract Surg. 2009;25:503-515.
6. Reinstein DZ, Archer TJ, Dickeson ZI, Gobbe M. Trans-epithelial phototherapeutic keratectomy protocol for treating irregular astigmatism based on population epithelial thickness measurements by Artemis very high-frequency digital ultrasound. J Refract Surg. 2014;30:380-387.
7. Reinstein DZ, Archer TJ, Gobbe M. Rate of change of curvature of the corneal stromal surface drives epithelial compensatory changes and remodeling. J Refract Surg. 2014;30:800-802.
8. Vinciguerra P, Azzolini C, Vinciguerra R. Corneal curvature gradient determines corneal healing process and epithelial behavior. J Refract Surg. 2015;31:281-282.
9. Reinstein DZ, Archer TJ, Gobbe M. Improved effectiveness of trans-epithelial phototherapeutic keratectomy versus topography-guided ablation degraded by epithelial compensation on irregular stromal surfaces [plus video]. J Refract Surg. 2013;29:526-533.



