Mapping the Microbiome
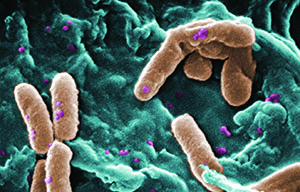
The microbial communities that inhabit our bodies are far more extensive than previously appreciated, outnumbering our own cells by an estimated factor of at least 10 to one.4,5 Although it has long been recognized that many of these microbes are critical participants in a variety of human diseases, their possible role in maintaining human health as commensal or symbiotic species has been unclear.6
In 2008, the National Institutes of Health launched the Human Microbiome Project with the goal of mapping the diversity of microbial species that cohabit the human body, and in doing so laid the groundwork for understanding the importance of these communities in human health.6 A key goal of this project was the identification of a “core” microbiome in healthy individuals to establish a benchmark from which variants could be identified and correlated with specific diseases.4 Samples were collected from 300 healthy subjects from five main body areas: dermal; urogenital; gastrointestinal; oral; and nasal.7 Subsequent studies revealed that healthy individuals differed remarkably in the microbes that colonize the different parts of their bodies.7 However, strong niche specializations were identified, giving rise to the concept of unique site-specific microbiomes.5,7 Much of this diversity remains unexplained, though diet, environment, host genetics and early microbial exposure have all been implicated.7
Studies from the Human Microbiome Project demonstrate a great deal of variation between individuals for each of the body areas examined. In addition, the microbial footprint within a given body habitat, or the diversity and abundance of different types of organisms, appears to have some predictive value when viewed in relation to various diseases.7 For instance, low diversity in the gut is associated with obesity and inflammatory bowel disease.7 Local biomes also serve functions that are indispensable for the well-being of the host, such as educating the immune system in tolerance towards commensal organisms.8 Dysregulation of this process has been shown to be associated with gastrointestinal diseases such as C. difficile colitis and irritable bowel syndrome.5 Remarkably, therapies utilizing fecal transplants are now providing successful treatment of C. difficile, demonstrating a compelling example of therapeutic manipulation of existing microbiomes for the alleviation of disease.1,5
What About the Eye?
Studies from the Human Microbiome Project gave rise to the question of whether mucosal membranes such as those at the ocular surface also possess a resident microbiota and, if so, do these too play a role in disease physiology?5,9 The conjunctival epithelium forms a barrier to ocular infection and represents an interface between diverse and abundant skin microbiota and the ocular surface.10 Communication between commensal microbial flora and the conjunctival epithelium may be critical to ocular surface homeostasis and the induction of immune tolerance.10 Therefore, it’s conceivable, as is the case in the intestine, that dysregulation of an ocular surface microbial community could contribute to ocular disorders. Furthermore, as in the case with fecal transplants, it may be possible to intervene in ocular surface diseases by introducing an appropriate commensal microbial flora.5
The first study documenting the presence of microbes on the ocular surface dates back to 1930, when researchers utilized conventional culture techniques to identify microorganisms.11 These methods have been invaluable from a historical perspective, but they’re limited by the specific growth requirements of individual microorganisms, resulting in a bias towards faster-growing or less-temperamental species that can be easily cultivated on standard media.9,12 It’s likely that many microbes remained undetected utilizing these methods.9 Today, gene sequencing has become the gold standard for phylogenetic studies of microbial communities and for assigning taxonomies to bacteria.6 Sequencing methods focus on minor, species-specific differences in the sequences of bacterial ribosomal RNA using the same powerful, high-fidelity technologies developed for the Human Genome Project. By this criterion we can measure which bacteria are resident, not simply which residents can grow on an agar plate.12 Although sequencing-based techniques provide improved sensitivity, it’s important to keep in mind that they lack the clinical relevance that cultures provide: In cases of microbial infection, you can’t test for antibiotic sensitivity with polymerase chain-reaction products.12,13 In addition, identification of species-specific rRNAs cannot, by itself, confirm that the species are viable residents of the ocular surface.5
|
Despite these challenges, recent studies have set out to identify an ocular surface microbiota that represents a persistent and stable consortium of viable organisms on the ocular surface, and to assess how this population varies in health and disease. One of the first examples of these efforts dates to a 2002 study showing that both the number of CFUs and diversity of bacterial species are increased in individuals who wear contacts.14 In 2007, researchers investigated the normal ocular surface bacterial flora, comparing healthy patients to those with dry eye.12 These investigators reported that 97 percent of patients with dry eye had positive bacterial cultures, while only 75 percent were positive among healthy subjects. However, both culture and DNA-sequencing techniques revealed common genera between dry-eye and healthy subjects, making identification of a disease-specific ocular microbiome inconclusive.
In 2009, scientists at the Bascom Palmer Eye Institute initiated the Ocular Microbiome Project, and in 2010, they published initial results classifying species from four healthy subjects to the phylum level by utilizing 16s rRNA gene-based sequencing.9 This study identified 59 distinct bacterial genera; 42 of these had not yet been previously reported in healthy eyes, demonstrating the power of rRNA sequencing to reveal a more diverse ocular microbiome than what had been previously reported. While the results showed significant variability among the analyzed subjects, they identified a putative core ocular surface microbiome, with 12 of the 59 genera identified found to be ubiquitous among all examined subjects. This analysis was limited by a small sample size, so further studies will be needed to confirm the core designation.
Leveraging the Microbiome
Based upon the lessons from other microbiomes, a key feature seems to be the population diversity that’s associated with disease states. Patients with chronic rhinosinusitis, for example, show the same types of nasal bacteria as unaffected patients, but their populations are altered such that diversity of species is reduced.15 Such reductions in microbiome diversity are observed in a number of diseases.10 Alteration in bacterial diversity and /or bacterial numbers may induce detrimental effects on host function through quorum-sensing mechanisms, or bacterial cell-to-cell signaling systems through which gene expression is regulated.12,16 Quorum-sensing is used by a number of bacterial species to coordinate the expression of genes involved in virulence, biofilm formation and pathogenicity.17 Studies are currently under way exploring the potential relationship between quorum-sensing mechanisms of bacterial populations and ocular disorders, such as dry eye.12
An alternative example of the potential importance of the ocular biome comes from a 2002 study of the role of commensal bacteria in mucin metabolism.14 This study showed that healthy individuals had higher levels of bacterial-derived mucinolytic enzymes, which presumably function to cleave bound mucins from the epithelial surface, releasing them into the tear film. These soluble mucins, in turn, reduce the growth of ocular bacteria, creating a regulatory feedback loop that acts to control the tear bacterial load. It’s easy to imagine how a shift away from such commensal species could disrupt this cycle and potentially allow for pathogenic bacterial growth.
How might identification of an ocular biome affect future therapies? One recent study explored the possibility of microbiome-based therapies for the treatment of ocular disorders through the use of probiotic eye drops.18 A four-week treatment with a Lactobacillus probiotic in eye drops was associated with a modest reduction in signs and symptoms of patients with mild to moderate vernal keratoconjunctivitis.18 The treatment caused no side effects and was well-tolerated. This novel use of topical probiotics suggests a potential role for ocular surface bacteria in regulating immune responses in the eye, and confirms the need for further exploration of probiotic therapy for ocular inflammation in humans.
Until a core ocular flora is defined with greater precision, it will be difficult to identify bacteria as symbiotics, commensals, pathogens or some combination of these.12 Perhaps more important is the realization that it’s not likely to be that simple. Thus, we have a long way to go before understanding the microbiomes that cohabit our bodies. Despite this, it is becoming increasingly apparent that rather than freeloaders or silent passengers, the microbes we carry are part of a continuous communication, a give-and-take that may be as much a part of our physiology as the autonomic impulses telling us to breathe and blink. It’s possible that many of the disorders that we now don’t fully understand will be explicable in the context of a symbiosis between the ocular biome and the ocular surface. REVIEW
Dr. Abelson is a clinical professor of ophthalmology at Harvard Medical School. Mr. Lane is director of Research and Development at Ora Inc. Dr. Slocum is a medical writer at Ora Inc.
1. Rupnik M. Toward a True Bacteriotherapy for Clostridium difficile Infection. N Engl J Med 2015;372:1566-1568.
2. Morgan XC, Segata N, and Huttenhower C. Biodiversity and functional genomics in the human microbiome. Trends Genetics 2013;29:51-58.
3. Alcock J, Maley CC, Aktipis CA. Is eating behavior manipulated by the gastrointestinal microbiota? Evolutionary pressures and potential mechanisms. Bioessays 2014;36:940–949.
4. Turnbaugh PJ, Ley RE, Hamady M, Fraser-Liggett C, Knight R, Gordon JI. The human microbiome project: Exploring the microbial part of ourselves in a changing world. Nature 2007;449:7164:804-810.
5. Zegans ME, Van Gelder RN. Considerations in understanding the ocular surface microbiome. Am J Ophthalmol 2014;158:3:420-2.
6. Huse SM, Ye Y, Zhou Y, Fodor AA. A core human microbiome as viewed through 16s rRNA sequence clusters. PLoS One. 2012;7:6:e34242.
7. The human microbiome project consortium. Structure, function, and diversity of the healthy human microbiome. Nature 2012;486:7402:207-214.
8. Zaura E, Keijser BJ, Huse SM, Crielaard W. Defining the healthy “core microbiome” of oral microbial communities. BMC Microbiology 2009;9:259.
9. Dong Q, Brulc JM, lovieno A, et al. Diversity of bacteria at healthy human conjunctiva. Invest Ophthalmol Vis Sci 2011;52:8:5408-5413.
10. Miller D, Lovieno A. The role of microbial flora on the ocular surface. Curr Opin Allergy Clin Immunol 2009;9:5:466-70.
11. Keilty RA. The bacterial flora of the normal conjunctiva with comparative nasal culture study. Am J Ophthalmol 1930;13:10:876-879.
12. Graham JE, Moore JE, Jiru X, et al. Ocular pathogen or commensal: A PCR-based study of surface bacterial flora in normal and dry eyes. Invest Ophthalmol Vis Sci 2007;48:12:5616.
13. Hanage, W. Microbiome science needs a healthy dose of skepticism. Nature 2014;512:247-8.
14. Berry M, Harris A, Lumb R, Powell K. Commensal ocular bacteria degrade mucins. Br J Ophthalmol 2002;86:1412–1416.
15. Biswas K, Hoggard M, Jain R, Taylor MW, Douglas RG. The nasal microbiota in health and disease: variation within and between subjects. Front Microbiol 2015;9:134.
16. Reading N, Sperandio V. Quorum sensing: The many languages of bacteria. FEMS 2006;254:1-11.
17. Brackman G, Coenye T. Inhibition of Quorum Sensing in Staphylococcus spp. Curr Pharm Des 2015;21:16:2101-8.
18. Lovieno A, Lambiase A, Sacchetti M, et al. Preliminary evidence of the efficacy of probiotic eye-drop treatment in patients with vernal keratoconjunctivitis. Graefes Arch Clin Exp Ophthalmol 2008;246:3:435-41.