Given our patient’s clinical history and exam, a differential diagnosis was constructed and included conditions that were associated with choroidal effusions such as ocular inflammation, posterior scleritis, orbital tumors and orbital arteriovenous fistula. More puzzling was the presence of blood in Schlemm’s canal. Etiologies for blood in Schlemm’s canal can be separated into pathologies that cause elevated episcleral pressure (carotid-cavernous sinus fistula, orbital arteriovenous fistula, mediastinal tumors, superior vena cava obstruction, ocular inflammation and orbital congestion), and pathologies that cause a lower relative intraocular pressure (hypotony, iatrogenic pressure from gonioscopy). Although there was no evidence of intraocular inflammation on clinical exam, the aforementioned findings in the context of proptosis, pain and significant injection of the eye made a scleral and anterior orbital inflammatory process the most likely etiology. The presence of a cavernous sinus thrombosis was also on the differential, especially given the findings of ptosis and limited motility of the left eye. Other considerations included orbital cellulitis, metastatic disease and lymphoproliferative disease, as these conditions can mimic a non-infectious inflammatory process.
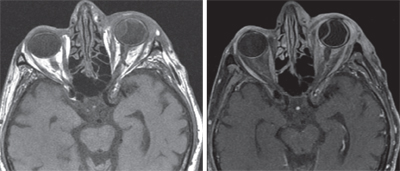
MRI of the orbit was subsequently performed and showed extensive inflammatory changes involving the preseptal soft tissues, intraconal fat and extraconal fat. Additionally, the left lateral rectus was significantly enlarged. The cavernous sinuses were clear bilaterally. No discrete masses were detected.
|
Following his negative workup for a specific systemic inflammatory disease or infection, the patient was diagnosed with idiopathic orbital inflammatory syndrome with posterior scleritis. He was subsequently treated with oral prednisone 80 mg daily, topical prednisolone acetate four times daily and topical atropine twice daily. The patient followed up in the Oculoplastics Department three days after his presentation to the Wills ER with improvement in pain. His physical exam showed decreased edema, erythema and proptosis. He regained full motility in his left eye. His visual acuity was 20/400 at his follow-up visit in the Retina Department, one week after initial presentation. His choroidal effusions were still present at that time. Unfortunately, no further information is known about this patient’s recovery as his medical management was continued in his hometown of Boston. Attempts to connect with the patient to inquire after his visual outcome were unsuccessful.
Discussion
Idiopathic orbital inflammatory syndrome (IOIS) is defined as a benign, non-infective clinical syndrome characterized by features of nonspecific inflammatory conditions of the orbit without an identifiable local or systemic cause. It is a diagnosis of exclusion that is made when all other causes of orbital inflammation have been ruled out.1 After Graves’ ophthalmopathy and lymphoproliferative diseases, IOIS is the third most common disease to affect the orbit.2 It is most commonly diagnosed in middle-aged adults and associated with a 2:1 female predilection, but can also present at the extremes of age.3
There have been many theories that suggest the pathogenesis of idiopathic orbital inflammation. A post-viral etiology has been suggested.4 An association with systemic autoimmune diseases such as Crohn’s disease, lupus and myasthenia gravis has also been reported.5,6,7 More recently, it has been suggested that IOIS is an autoimmune reaction secondary to a molecular mimicry process.8
Idiopathic orbital inflammatory syndrome can be considered a continuum of disease with a varying presentation, ranging from rare bilateral diffuse orbital inflammation to the more common unilateral isolated myositis or dacryoadenitis. This spectrum of presentation can also include posterior scleritis. Presenting symptoms usually include edema, pain, injection, proptosis, diplopia and chemosis. If posterior scleritis is present, the patient may also complain of an acute decrease in vision. The progression of symptoms is typically acute, developing within hours to days.9,10
Systemic steroids remain the mainstay of therapy, with improvement in up to 76 percent of cases. Patients who are non-responsive, unable to tolerate or dependent on steroids may undergo radiotherapy, but this has been associated with poor response.5 Individual response to treatment with chemotherapeutics and immunomodulatory drugs has been reported in recalcitrant cases.11,12 Clinical outcomes of patients who suffer from IOIS are good, and most patients have complete resolution with relapse rates related to the severity and extent of the initial disease. However, patients who present with posterior scleritis as a component of their disease are at serious risk for permanent vision loss. In one study of 99 patients, 30 percent of subjects experienced permanent visual impairment.10 Myositis has been shown to be frequently associated with scleritis, as demonstrated in this patient. Yet, the presence of concomitant myositis does not worsen the visual prognosis of the scleritis.13
In conclusion, IOIS is a diagnosis of exclusion that should only be made after other pathology has been ruled out. Its clinical picture is variable, but typically presents acutely with unilateral pain, periorbital edema and injection. Less commonly, it can present as scleritis that can be more difficult to differentiate from other diseases that cause posterior ocular and anterior orbital inflammation. The etiology of IOIS remains elusive. An autoimmune-mediated process is most likely given the response to steroids and immunomodulatory drugs. Systemic corticosteroids remain the mainstay of treatment. While most patients experience a full recovery, patients with posterior scleritis should be considered at risk for serious vision loss and monitored closely. REVIEW
The author would like to thank Michael P. Rabinowitz, MD, and Robert Penne, MD, of the Wills Eye Hospital Oculoplastic and Orbital Surgery Service.
1. Yuen S, Rubin P. Idiopathic orbital inflammation: Ocular mechanisms and clinicopathology. Ophthalmol Clin North Am 2002;15:121-126.
2. Weber A, Romo L, Sabates N. Pseudotumor of the orbit: Clinical, pathologic, and radiologic evaluation. Radiol Clin North America 1999;37:151-168.
3. Scott I, Siatkowski R. Idiopathic orbital myositis. Curr Opin Rheumatol 1997; 9:504-512.
4. Purcell J, Taulbee W. Orbital myositis after upper respiratory tract infection. Arch Ophthalmol 1981;99:437-438.
5. Young R, et al. Orbital pseudotumor and Crohn disease. J of Pediatr 1981;99:250-252.
6. Serop S., et al. Orbital myositis secondary to systemic lupus erythematosus. Acta Ophthalmol 1994;72: 520-523.
7. Van de Mosselaer G, et al. Pseudotumor orbitae and myasthenia gravis: A case report. Arch Ophthalmol 1980;98:1621-1622.
8. Harris G. Idiopathic orbital inflammation: A pathogenetic construct and treatment strategy: The 2005 ASOPRS Foundation Lecture. Ophthal Plastic Reconstr Surg 2006;22:79-86.
9. Yuen S, Rubin P. Idiopathic orbital inflammation: Distribution, clinical features, and treatment outcome. Arch Ophthalmol 2003;121:491-499.
10. McCluskey P, Watson PG, Lightman S, Haybittle J, Restori M, Branley M. Posterior scleritis: Clinical features, systemic associations, and outcome in a large series of patients. Ophthalmology 1999;106:2380-6
11. Paris G, Waltuch G, Egbert P. Treatment of refractory orbital pseudotumors with pulsed chemotherapy. Ophthal Plastic Reconstr Surg 1990 6:96-101.
12. Shah S, et al. Low-dose methotrexate therapy for ocular inflammatory disease. Ophthalmology 1992;99:1419-1423.
13. Boonman, Z. F. H. M., et al. Orbital myositis in scleritis. Br J Ophthalmol 2003;87:38-42.