Despite the best of intentions, clinically important information sometimes takes years to become incorporated into standard practice. For example, Niels Ehlers demonstrated the relationship between central corneal thickness and measured intraocular pressure 25 years ago, yet until recently this information was almost universally ignored.
 |
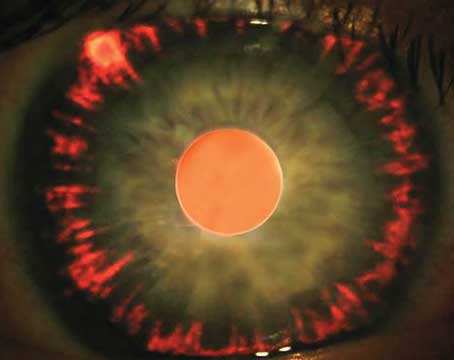
| A large cup in a 1.9-mm disc, like the one above, may be physiological rather than pathological. |
As a result, small glaucomatous discs may be misdiagnosed as normal, and large normal discs may be misdiagnosed as glaucomatous.
Taking Disc Size into Account
In fact, C/D tends to be larger in healthy eyes that have larger discs. Recently published normative data relates C/D to disc size using several thousand eyes from the Blue Mountain Eye Study in Australia.2 Investigators there found the average disc diameter to be 1.5 mm; they classified discs from 1.0 to 1.3 mm as small, from 1.4 to 1.7 mm as medium, and from 1.8 to 2.0 mm as large. Mean C/D was about 0.35, 0.45, and 0.55 for the respective size categories; the 95th percentiles for upper limit of normal C/D were 0.59, 0.66 and 0.74. (These numbers are easier to remember if you round them off to 0.55, 0.65, and 0.75—think highway speed limits.)
These findings have numerous implications for glaucoma diagnosis and monitoring:
• A high ratio may not be pathologic. When first examining a patient, it's important to know that a large cup in a small disc is likely to be pathologic, but a large cup in a large disc may simply be physiologic. For example, a C/D of 0.5 is often pathologic in a small cup, but is usually physiologic in a large cup.
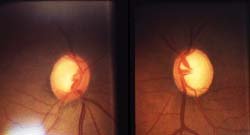 |
| When C/D is large, as in the large discs pictured above (1.8 mm OU), smaller changes in C/D are more significant. Here, C/D is similar (0.8, 0.9), but the right eye is normal; the left eye has moderate superior field loss. (Note changes in the inferior nerve fiber layer.) |
• C/Ds for large discs change by a smaller amount. Less change detected in a large disc with a physiologically large cup may represent just as much progression as a greater amount of C/D change detected in a small disc. For example, a large disc might begin with a C/D of 0.7 and progress to 1.0, while a small disc might change from no cup to a C/D of 1.0.
• C/D changes caused by glaucoma occur more slowly in large discs than in small discs. This is a consequence of the way linear measurements relate to area in geometry. A 50-percent loss of rim area in a disc with no physiologic cup would enlarge the C/D from 0.0 to 0.7. However, a 50-percent rim loss in a disc which originally had a C/D of 0.7 will only increase the C/D to a little more than 0.85.
Because the C/D changes more gradually in large discs (for a given amount of rim loss), glaucoma patients with large discs must be observed with extra care.3 For this reason, it's especially important to have baseline photos of large discs to make it easier to detect change.
• C/D asymmetry isn't always pathological. Usually, glaucoma is likely if the C/D of one eye differs from that of the fellow eye by more than 0.2. However, if the two discs are of significantly different sizes, that could be sufficient to explain the difference in ratios. (See example.)
Easier than It Sounds
Few doctors realize how easily disc size can be measured at the slit lamp. Simply classifying a disc as small, medium or large is clinically helpful, and can be accomplished in 30 seconds.
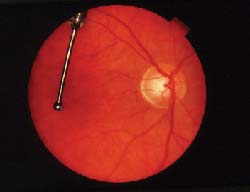 |
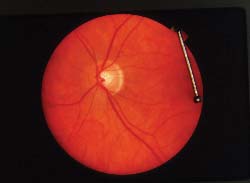 |
| In this healthy patient's eyes, asymmetry is physiological, not pathological. Discs are 1.8 mm and 1.6 mm; C/D ratios are 0.65 and 0.35. | |
• Take photographs. When a disc is large, photographs may be helpful in determining change, which is more difficult to observe in large discs (as noted above). Also, a photograph is a concrete record of the exam, and it gives you the option of remeasuring later if necessary.
The most accurate measurements—generally used only for research purposes—measure the disc size on a photograph and then apply an optics formula. Such formulas correct for magnification induced by the optics of the eye, taking axial length, keratometry and refraction into account. This level of precision actually isn't necessary, however, to classify a disc as small, medium or large, which is sufficient to improve the accuracy of your glaucoma diagnosis. Several much simpler alternatives are available.
• Use an indirect lens. This is quick, easy and provides enough information to classify a disc as small, medium or large. Project the slit lamp light beam onto the disc through a 60-, 78-, or 90-D handheld lens and adjust the beam height to coincide with the vertical disc diameter.
To calibrate the result, consider the minification induced by the lens. Measurements with the 60-D lens require no adjustment. Measurements made using the 78-D lens should be multiplied by 1.1, and those made with the 90-D lens should be multiplied by 1.4. (I avoid using a 90-D lens because the smaller image can cause greater measurement errors.) Even if you don't calibrate your slit beam height and multiply your measurements by the appropriate factor, a little experience will enable you to determine which size category best describes the disc.
A drawback to using an indirect lens is that the distance from the lens to the eye can vary, affecting the magnification. To compensate, use the highest feasible magnification setting of the slit lamp oculars. This minimizes the depth of field and may reduce the likelihood of error.
Also, be aware that patient refractive error can influence the measurement. Myopic eyes can cause disc size to be underestimated; hyperopic eyes can cause disc size to be overestimated. Twelve diopters of ametropia will change the apparent size about 22 percent when using a 60-D lens and 13 percent with a 78-D lens.4
• Measure with the Heidelberg Retina Tomograph (HRT). The HRT is very convenient for this purpose, if one is available in your clinic. The OCT and GDx may be less accurate, since they don't account for the patient's keratometry and refraction.
• Use a contact lens such as the Goldmann lens or Zeiss goniolens. Because these lenses are held against the cornea, the focal length is fixed, which may increase the accuracy of your measurement. However, because of the need to anesthetize the eye, use a gel and disinfect the lens after each use, these methods are inherently more time consuming and inconvenient. The gel also makes the pa-tient's vision blurry afterwards, something most patients don't appreciate. And, like indirect lens measurements, contact lens measurements are somewhat influenced by refractive errors.
It's intuitively obvious that the longer a beam is, the more it will sag under load. Imagine walking over a one-inch-thick plank to cross a creek. If the plank spanned 3 feet, your weight wouldn't stress the plank; but, if it spanned 9 feet, your weight might bow the plank and cause it to crack. 1. Bellezza AJ, Hart RT, Burgoyne CF. The optic nerve head as a biomechanical structure: initial finite element modeling. Invest Ophthalmol Vis Sci. 2000 Sep;41:10:2991-3000.
Are Larger Discs More Susceptible to Deformation?
This principle suggests that smaller discs might be structurally less vulnerable to pressure-induced deformation (cupping). Work by Claude Burgoyne, MD, has predicted that larger discs might be more susceptible to damage for a given intraocular pressure, in part because the longer unsupported lamina cribrosa "beams" in a large disc might bend more readily under increased pressure than the shorter lamina cribrosa in a small disc.1
However, a recent prospective study of 763 eyes with ocular hypertension or chronic open angle glaucoma found no association between progression and disc size.2 Progression did correlate with smaller rim area, larger beta zone of parapapillary atrophy, and greater age.
Further study of disc susceptibility may reveal that beam span is less important than beam strength. In other words, the strength of the lamina cribrosa may depend not only upon its length, but also upon its material properties. Some individuals may have weaker connective tissue; this would be analogous to using a rotted plank to span the creek.
2. Jonas JB, Martus P, Horn FK, Junemann A, Korth M, Budde WM. Predictive factors of the optic nerve head for development or progression of glaucomatous visual field loss. Invest Ophthalmol Vis Sci. 2004 Aug;45:8:2613-8.
Adding In the Missing Factor
With a little experience using the slit lamp and an indirect lens you'll be able to categorize discs as small, medium or large quickly and easily. Just remember that approximately 95 percent of normal small discs have a C/D £0.55; 95 percent of medium discs have a C/D £0.65; and 95 percent of large discs have a C/D £0.75.
Hopefully, the importance of disc size in evaluating C/D will soon become mainstream knowledge. Taking the size of the disc into account when diagnosing and monitoring glaucoma could have a significant impact on the effectiveness of your treatment—and your patient's vision.
Dr. Libre is a glaucoma specialist in Norwalk. He also attends at the glaucoma clinic of the Harkness Eye Institute at New York-Presbyterian Hospital. He can be reached at pel3@columbia.edu.
1. Bengtsson B. The variation and covariation of cup and disc diameters. Acta Ophthalmol 1976; 54:804-818.
2. Crowston JG, Hopley CR, Healey PR, Lee A, Mitchell P. The effect of optic disc diameter on vertical cup to disc ratio percentiles in a population based cohort: the Blue Mountains Eye Study. Br J Ophthalmol 2004;88:766-770.
3. Garway-Heath DF, Ruben ST, Viswanathan A, Hitchings RA. Vertical cup/disc ratio in relation to optic disc size: its value in the assessment of the glaucoma suspect. Br J Ophthalmol 1998; 82:10:1118-24.
4. Ansari-Shahrezaei S, Maar N, Biowski R, Stur M. Biomicroscopic measurement of the optic disc with a high power positive lens. Invest Ophthalmol Vis Sci 2001;42:153-157.