What happens when patients who’ve demonstrated the willingness to pursue spectacle independence through laser refractive surgery develop cataracts? Can they realistically expect excellent visual outcomes with IOLs? According to surgeons, the answer is a qualified “yes.” Here, they share their pointers for yielding the best possible results with these tricky eyes.
Two things happen with laser refractive surgery, says Daniel H. Chang, MD, of Empire Eye and Laser Center in Bakersfield, California. “Number one, the ratio of the anterior and posterior corneal curvature changes, so assumptions used by keratometers to measure K’s break down. Number two, the a
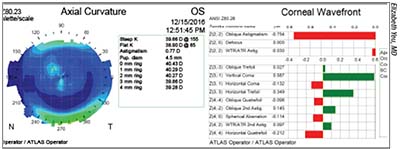 |
| Corneal topography of a post myopic LASIK eye shows irregular astigmatism within the central cornea and a high degree of coma. Such an eye is a poor candidate for an EDOF lens, and may be better suited to a monofocal IOL. |
ssumptions used by IOL calculation formulas to calculate effective lens position break down, because the determined keratometry no longer reflects the shape of the anterior chamber.”
“In these eyes, we are making assumptions about the relationship between the curvature of the anterior and posterior corneal surface—a relationship that is different once you alter the anterior surface of the cornea,” concurs Elizabeth Yeu, MD, partner at Virginia Eye Consultants and an assistant professor at Eastern Virginia Medical School in Norfolk. “The bigger picture is that if you don’t adjust your preop planning, you’ll end up with hyperopic outcomes in your post-myopic LASIK patients and myopic outcomes in your post-hyperopic LASIK patients,” she says.
Another thing that makes these eyes challenging when it’s time for cataract surgery is the fact that laser ablative techniques and their effects have changed over time. “Not all post-refractive eyes are the same,” says Michael Lawless, MBBS, FRANZCO, of Vision Eye Institute, Chatswood, New South Wales, and a clinical associate professor at Sydney Medical School in Australia. “Some patients come in having had PRK or LASIK for high myopia in the 1990s, for example. These eyes have a large amount of induced spherical aberration and are often very long in terms of axial length. They also commonly have some induced irregular corneal astigmatism, a reflection of the laser technology, lack of tracking, etc., from that period,” he says.
Measure for Success
Although there’s not a single, perfect way to work up a post-refractive eye for cataract surgery, thoroughness on each step of the process is important. “You should do your best preop. Each step increases your chance of getting it right,” says Dr. Chang.
Dr. Yeu, whose practice has surgical counselors on staff, always starts with the nondominant eye in post-refractive patients. “The reason for that is that if you have similar axial lengths and similar flat Ks in a post-myopic patient, for example, the response to the first-eye surgery, in terms of residual refractive error, can truly help guide what you need to do with the second eye. This is even more important than in a naïve cornea. These patients in particular have average Ks of around 38.5 and axial lengths of about 26 mm in both eyes,” she says. “The postoperative refractive results can lend insight to the second-eye planning.
“Accurate keratometry is one of the core pieces to really refine your outcomes to be within a half- or quarter-diopter spherical equivalent of your prediction error,” Dr. Yeu continues. She uses an Atlas topographer (Carl Zeiss Meditec; Jena, Germany) as her primary topographer in post-refractive eyes. “With the Atlas specifically, you can enter the central 4 mm zone into the ASCRS post-refractive calculator,” she says. “We also get extra diagnostic information for post-refractive eyes.” In addition to collecting more data with the Cassini corneal shape analyzer (Cassini Technologies; The Hague, The Netherlands) and the Lenstar (Haag-Streit; Keoniz, Switzerland) for these patients, she also uses anterior segment OCT.
Dr. Chang starts by trying to assess how important spectacle independence is to patients, plus their satisfaction with the prior refractive surgery. “I like to ask them how happy they had been with their vision after the initial refractive surgery. Sometimes, mostly with RK, but often with commercial LASIK and PRK as well, they’ll say, ‘You know, it was never quite right.’ These patients should be approached with caution, since some factor such as irregularity, decentration or the like may continue to affect their quality of vision after cataract surgery as well. However, if they say, ‘It was great, but then it recently got worse,’ then you can assume the cataract made vision worse, so cataract surgery will help them,” he says. He adds that this line of questioning also helps alert him to hard-to-please personality types. “If they were big complainers after their first surgery, then there’s a good chance they’ll be complaining after this surgery as well.
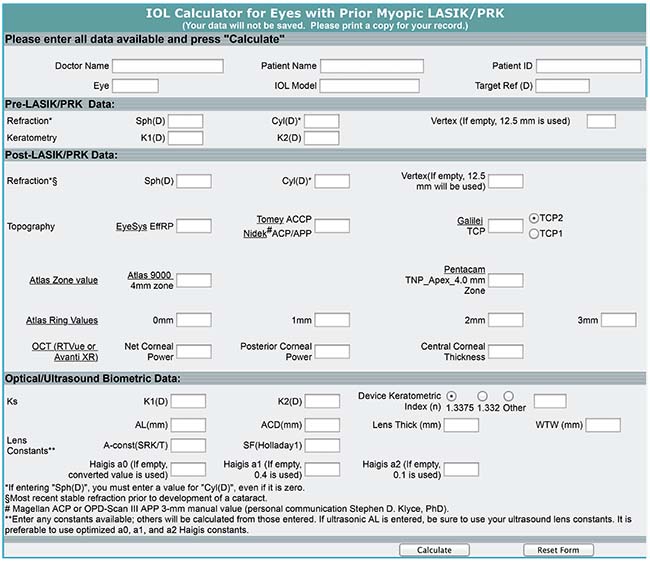 |
| Even though the ASCRS calculator has fields for historical data regarding prior refractive surgery, many surgeons enter current measurements from placido disc and Scheimpflug topography systems to get suggested IOL powers for their post-refractive patients. |
“On exam, I look at the quality and condition of the cornea, assessing the quality of the optical zone and any possible incisions (e.g., LASIK flap or RK incisions) that are present,” continues Dr. Chang, who gets placido disk topography with an Atlas. “The topography tells me two things: number one is whether they’ve had a myopic or hyperopic refractive procedure. Number two is the size, centration, and degree of the previous treatment zone.”
Like Dr. Yeu, Dr. Lawless includes intraoperative aberrometery in his measurements. “These eyes are hard to get right, and benefit from intraoperative aberrometry,” he says. “They may also benefit from IOLs that can be manipulated postop to refine a residual refractive error.”
Selecting IOLs
Patients with prior refractive surgery can choose from a variety of IOL types. The Light-Adjustable Lens (RxSight; Aliso Viejo, California), approved by the FDA in late 2017, is a new option that may help mitigate some of the variability in visual outcomes that can plague these eyes after cataract surgery. “There are two ways of approaching the problem of post-refractive eyes,” says Dr. Chang. “Number one is to make better calculations and measurements. Number two is to make better implants. You could use lenses with some refractive forgiveness, or the Light-Adjustable Lens, where you don’t have to hit the target, but can instead lock them in later. In my experience, it’s always better to hit the target, however.”
Although Dr. Lawless also says that light-adjustable lenses may merit consideration in surgical planning for post-refractive eyes, he notes that he can get excellent results without them. “By paying attention to everything and optimizing the ocular surface, I expect to be within +/- 0.5 D for both sphere and cylinder 90 percent of the time. So it’s hard to justify using an IOL that can be manipulated postop in fewer than 10 percent of eyes, especially when any errors can readily be treated with a small amount of PRK,” he says.
Dr. Chang finds that extended depth-of-focus lenses are suitable for some of his post corneal refractive surgery patients, and may offer better visual range than monofocals. “With EDOFs, theoretically, you can get better-quality vision through a range of refractive change, but I don’t promise that to patients, because as a practical matter it’s difficult to achieve.”
Dr. Yeu says that EDOFs can work well for patients who are interested in crisp distance vision and willing to consider fine-tuning their refractive outcomes postop. While EDOF IOLs can be successfully implanted in post-refractive eyes, corneal topography is vital to this determination. “If patients are looking for distance vision with EDOF lenses, they should have a well-centered ablation zone with no evidence of irregular astigmatism. If they go with a refractive package like this in our practice, then postop enhancements—for which these eyes are at higher risk—are performed after postoperative month two or three at no additional charge,” she says.
She adds that improved lens offerings, together with thorough preoperative workups, have helped make presbyopia-correcting lenses a real option for post-refractive eyes. “I never used to actually consider a diffractive multifocal or diffractive-optic IOL for post-refractive patients seeking spectacle independence and a range of vision. But now, patients who have nice, well-centered ablations and who do not have astigmatism do very nicely using the EDOF lenses, in my experience. The pseudoaccommodating platform, such as the Crystalens or Trulign (both Bausch + Lomb; Rochester, New York), is also an option in all post-refractive eyes with good vision potential, although I have much more experience with the EDOF IOL platform,” she says.
Another viable option for these patients appears to be low-add diffractive multifocal IOLs. In a small retrospective chart-review study1 partially funded by Alcon, post-LASIK eyes implanted with the Acrysof IQ ReSTOR +2.5 (Alcon Laboratories) achieved distance visual acuity and refractive results equivalent to post-LASIK eyes implanted with Alcon’s Acrysof SN60WF monofocal IOL, while also achieving very good intermediate and good near vision. Only 4/44 eyes studied from both groups had a spherical equivalent refractive error >0.5 D from the intended refractive target; all of these had a history of hyperopic LASIK.
Dr. Chang notes that gaining some refractive forgiveness with an EDOF is not as simple as aiming for plano and implanting the lens, however. “With the Symfony, you actually have to target a little bit hyperopic to gain the EDOF advantage,” he says. “This EDOF lens has a better depth of focus only on the myopic side of the defocus curve. Therefore, to maintain good visual quality at optical infinity, you actually have to aim a little positive to gain that advantage. Consequently, the sacrifice involved is to the reading, or near vision, but in return I have the ability to give patients with corneal aberrations a higher potential of getting great distance vision without correction. In these patients, I’ll take a Symfony and aim for +0.5 D. The main goal is uncorrected distance vision, and as long as you tell patients this in advance, they’ll be happy. If they do get some good near vision, that’s great: But if not, they’re already primed in terms of their expectations,” he explains.
For post-refractive patients who aren’t good candidates for premium IOLs, Dr. Yeu selects the sphericity of monofocals with care. “In general if there’s any question at all, I’m using zero-sphericity monofocal IOLs. This helps to at least avoid adding any further aberrations. When you look at the higher-order aberrations profile, while there is a significant range, on average, flattened corneas have a greater amount of positive spherical aberration. So you could go with either a zero-sphericity lens, or with a negative-spherical-aberration lens. For a more prolate hyperopic-LASIK eye, which has greater amounts of negative spherical aberration in the cornea, zero-sphericity IOLs are great: You wouldn’t want to use a negative-spherical-aberration lens, like a lot of the today’s aspheric monofocals. You actually want to use a zero-sphericity IOL, or an older, positive-spherical-aberration lens for these patients to neutralize what’s going on with the cornea,” she says. Dr. Yeu and colleagues conducted a prospective study that showed a positive correlation between higher-order aberrations and depth of focus in eyes with prior myopic or hyperopic PRK and LASIK. That study also influenced her practice patterns when choosing the sphericity of IOLs for post-refractive eyes.2
Calculating Lens Power
When it’s time to calculate suggested lens powers, the ASCRS IOL Calculator (iolcalc.ascrs.org) and the Barrett True K formula are valued resources for post-refractive eyes. “I’m really grateful for the contributions of Doug Koch and Li Wang and Graham Barrett,” Dr. Yeu says. “It’s been further refined over time, especially with greater input utilizing Galilei information and anterior segment OCT. In my experience, my results validate what we see in the literature: The information that you get with the calculator for the suggested lens powers is even more accurate than just having the historical method, where you begin with the original surgical data. So we use the ASCRS Calculator, plus the Barrett True K formula, on everybody. Inputting the concentric mires of the first 4 mm of placido disk rings from the Atlas into the ASCRS post-refractive calculator really helps to zero in on the lens calculations.”
Dr. Chang also uses the ASCRS calculator for these eyes. “I put my topography data into the ASCRS calculator,” he says. “It prints out one page with all the potential formulas applicable to my biometry, topography and imaging data, and provides suggested IOL powers. It’s a really nice resource. You can click myopic or hyperopic laser vision correction, punch in your name, your patient name, some basic information, plug in all the biometric measurements you have, and it spits out the IOL numbers. The way I see it, the more formulas you compare, the better, and the calculator makes that easy.”
One recent update in the ASCRS calculator involves the addition of the Barrett True K formula for myopic and hyperopic LASIK and PRK, as well as eyes with a history of RK. Dr. Lawless, who with colleagues conducted a review of refractive results of known IOL formulas for
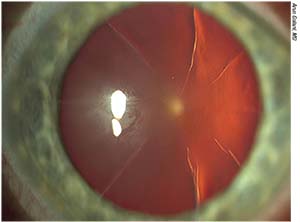 |
| Patients with prior RK should be counseled to expect a hyperopic outcome in the early postoperative days due to the RK’s flattening effect on the cornea. Refractive stability should settle in at close to plano at around six weeks post cataract surgery, surgeons say. |
post-refractive eyes,3 says that the Barrett True K most consistently produces refractive outcomes close to emmetropia in post-refractive eyes. “We have internal data on a large number of eyes to satisfy us that this is the best formula,” he says. The Asia Pacific Association of Cataract and Refractive Surgeons (www.apacrs.org) advances the Barrett True K for IOL power calculations in post-refractive eyes.
“Between the Barrett True K and the ASCRS post-refractive calculator, enhancements are, fortunately, few and far between,” says Dr. Yeu, who offers this pearl when entering data from post-refractive eyes into the ASCRS calculator: “For post-refractive eyes, when you’re putting data into the ASCRS post-refractive calculator, don’t use the ‘optimize axial length’ adjustment. You want to put the patient’s original axial length into the calculator,” she says, because optimizing would produce myopic results. “Two weeks postoperatively, if the patient still ends up being a little bit more myopic than you expected, you can sometimes use that information to guide you with regard to what IOL option you’re going to use in the second eye, if that patient’s preop ocular keratometry and axial lengths were similar.”
Dr. Yeu’s second pearl is that post-refractive eye data entered into the calculator should yield suggested IOL powers within a specific range—and if not, it should alert you that something is probably off. “Generally speaking, you’ll be getting IOL numbers that are going to be average because they’re post-refractive,” she says. “So the IOL-power numbers should be somewhere in the range of about 19 to 24. If they’re not, then I always go back and look at the information to see why they may not be in that average-power range. Sometimes it’s because they’ve regressed over time; or they may have evidence of ectasia or something else going on. But in general, these eyes should have average IOL powers popping up in the calculator as recommendations.”
Making History Optional
Dr. Yeu and Dr. Chang both say that current preoperative measurement and IOL power calculation techniques for post-refractive eyes yield excellent results without data from prior refractive procedures. “Five-plus years ago, I really harped on trying to find the historical data if I could,” Dr. Yeu recalls. “But as it turns out, we often aren’t able to get that historical data, and in my clinical experience, using the calculator and having good K-value input from multiple devices actually gives more accurate power calculations without it.”
Dr. Chang agrees that K values collected during the preop workup for cataract surgery are a more reliable basis for lens calculation than those from some prior refractive surgery would be. “Previous refractive surgery data is not any better than any of the current measurement and IOL calculation formulas,” he says. “The general thinking is moving away from using historical data, which is nice. I think one big factor is that pre-LASIK Ks were probably just sim Ks measured to guide the laser ablation and were never meant to be used for IOL calculations. Therefore, there’s no real benefit to having prior surgical data. I like to keep things simple. If you do more work getting prior data, it doesn’t hurt to look at it. But we don’t track prior data, and we haven’t tracked it for years. Most people don’t have it and it’s hard to get.”
Educating Your Patients
For all the advancements in IOL selection, measurement and power calculation for post-refractive eyes, visual outcomes are still more subject to variability than in virgin corneas.2 “The most important thing is not to over-promise,” says Dr. Chang. “I tell post-refractive patients that whatever I do, there’s going to be a higher chance of being off, and a higher chance of needing an enhancement. You should essentially be prepping your patient for that because of the increased variability in outcome with these eyes. I think that’s important.”
Dr. Yeu says that her practice’s clinical counselors initiate that important conversation with post-refractive patients. “They discuss the fact that our outcomes, while they’re very good, are not as accurate as those calculated for a naïve cornea in an average eye, because of the changes to the cornea induced by the prior surgery. So these patients are advised that they’re at a slightly higher risk of requiring a touch-up to get them to the uncorrected vision that they’re looking for, or that they’re at higher risk of needing glasses for all ranges of vision,” she says.
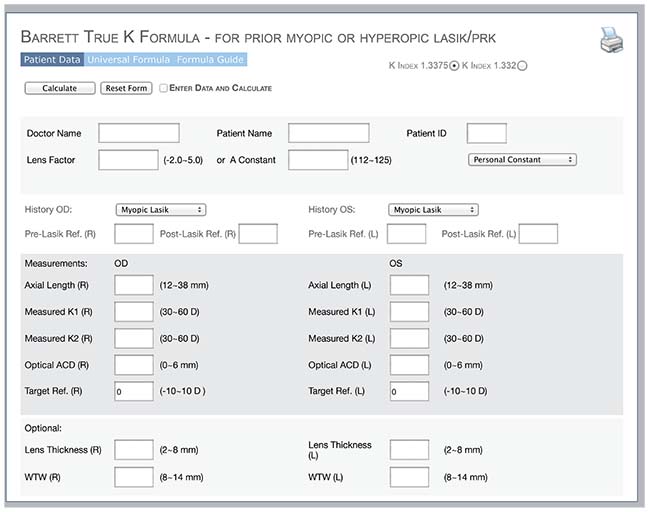 |
| The Barrett True K formula for eyes with a prior history of LASIK or PRK has found favor with ophthalmologists tasked with planning cataract surgery. The Asia Pacific Association of Cataract and Refractive Surgeons provides a calculator at www.apacrs.org. |
Dr. Yeu adds that one subcategory of post-refractive eyes calls for extra patient education, since the early postop refractive outcome is off as a matter of course. “In post-RK eyes, they’ll have a hyperopic outcome for about the first three to six weeks,” she says. “It’s just the effect of the RK wounds. So they start off a little hyperopic and you expect that. In a post-RK eye, on day one, that conversation needs to be had. I usually tend to wait about six weeks in between eyes for those patients because it takes a little bit longer for their final refractive outcome to settle in. I always caution them, ‘Your vision will be blurred at first.’ If they end up at around +2 to start with, that’s exactly where I want them to be, because at week six, they’ll end up being close to plano. On the other hand, if they end up plano and 20/25 on day one, and they’ve got an eight-cut RK or more, then by week six they’re going to end up being myopic. It’s just because of the hyperopic flattening effect of the RK wounds, even when you don’t see any clinically evident corneal edema. They can have a pristine-looking cornea on day one; it’s just a side effect of having the RK wounds. These are the trickiest post-refractive eyes to deal with,” she says.
Post-refractive patients are a self-selected group of people who’ve already demonstrated a desire for spectacle independence and good vision. “Someone who’s had previous refractive surgery has obviously demonstrated a desire for spectacle independence at some point in his or her life. You have to consider that,” says Dr. Chang of cataract surgery planning for post-refractive eyes. By enhancing your already-careful preop workup by collecting some extra measurements, and carefully weighing your patients’ suitability for premium IOLs, you can get the odds of good outcomes for these eyes firmly on your side. REVIEW
Dr. Lawless is a consultant for Alcon. Dr. Yeu reports that she has consulted for Bausch + Lomb, Alcon and Johnson & Johnson Vision. Dr. Chang has consulted with Carl Zeiss Meditec on the IOLMaster and IOLMaster 700, and with Johnson & Johnson Vision for products related to cataract, including the Symfony IOL and multifocal IOLs.
1. Fisher B, Potvin R. Clinical outcomes with distance-dominant multifocal and monofocal intraocular lenses in post-LASIK cataract surgery planned using an intraoperative aberrometer. Clin Exp Ophthalmol. 2018 Jan 23. doi: 10.1111/ceo.13153. [Epub ahead of print]. Accessed 2 April 2018.
2. Yeu E, Wang L, Koch DD. The effect of corneal wavefront aberrations on corneal pseudoaccommodation. Amer J Ophthalmol 2012;153:972-81.
3. Hodge C, McAlinden C, Lawless M, Chan C, Sutton G, Martin A. Intraocular lens power calculation following laser refractive surgery. Eye and Vision 2015;2;7:
https://doi.org/10.1186/s40662-015-0017-3. Accessed February 3, 2018.