Workup, Diagnosis and Treatment
 |
 |
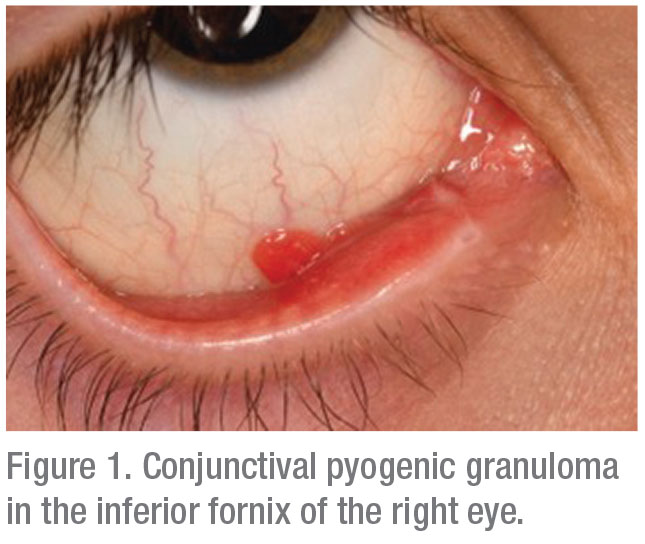
Upon presentation, nearly one year after the initial appearance of this conjunctival lesion, the patient was advised to have surgical excision and exploration for a suspected large, ruptured chalazion with associated pyogenic granuloma. In the operating room, the pyogenic granuloma was excised with wide margins, disclosing a 4-mm, open defect in the tarsoconjunctival tissue. Enlargement of the wound disclosed a wooden foreign body measuring 1.5 cm in length, extending into the orbit (Figure 2 and 3). The wound was rinsed with antibiotics and partially closed to allow for drainage.
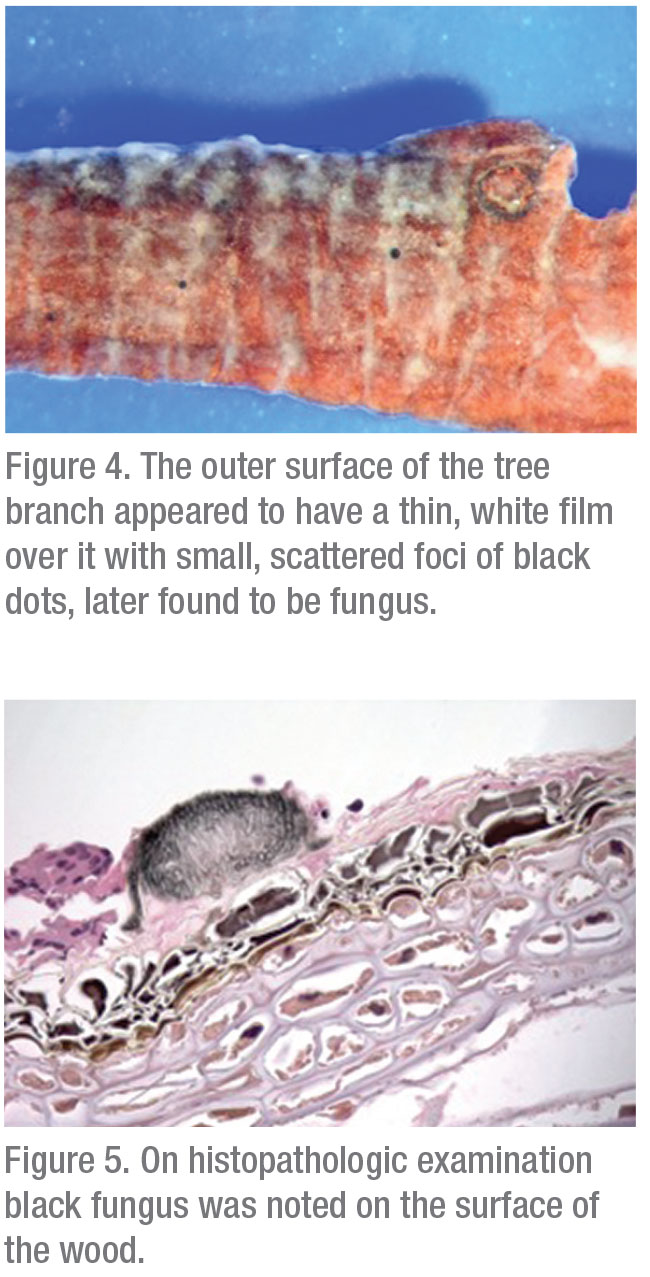
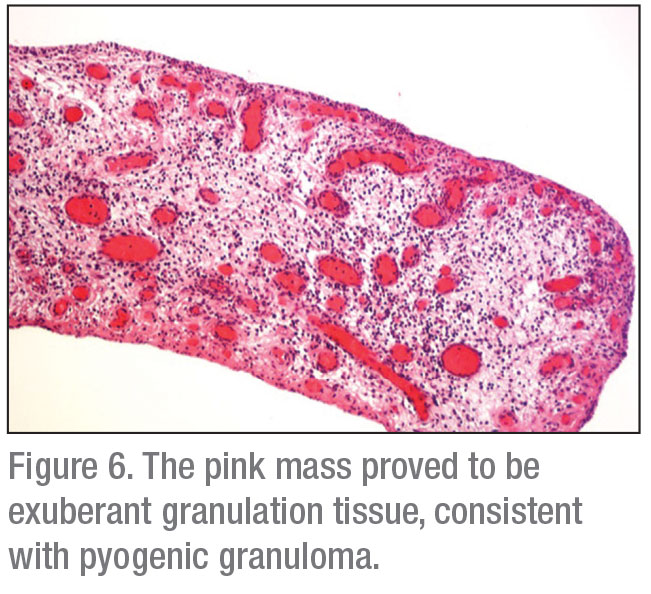
Histopathology demonstrated a mass composed of birefringent PAS-positive material consistent with wood. Foreign body giant cells and polymorphonuclear leukocytes were present. Several small, circular, black foci were noted grossly on the surface of the wood (Figure 4). These proved to be colonies of pigmented fungal hyphae (Figure 5). Examination of the conjunctival lesion revealed a mass of exuberant granulation tissue consistent with a pyogenic granuloma (Figure 6).
Following identification of the wooden foreign body, the patient’s mother recalled an incident one-and-a-half years prior when the patient had run into a bush chasing after a baseball and had suffered a small, cutaneous abrasion on the right lower eyelid with no residual trauma. Three months later, the first pyogenic granuloma appeared in close proximity to the area of prior trauma.
The patient was discharged on a regimen of oral amoxicillin for seven days and topical dexamethasone/neomycin/polymyxin B sulfate for three weeks. On follow-up evaluation one month later, the patient had complete healing of the wound with no recurrence of the conjunctival lesion or evidence of residual infection.
Discussion
Intraorbital wooden foreign body (IOWFB) is a rare complication of penetrating ocular injury that can pose a particularly difficult clinical challenge for ophthalmologists. A component of this challenge stems from the rare nature of wooden foreign body injury to the eye. Management guidelines are based on several case reports1-3 and small case series4,5 described in the literature.
Often, as in this case, a prior history of trauma isn’t volunteered at the time of clinical presentation. This may be because a wooden foreign body injury can occur remote from the time of clinical presentation. Additionally, this injury can occur in the pediatric population, who might not volunteer a history of trauma. Young males under 30 years of age are the prime targets at risk for such injuries, and a high degree of suspicion should be kept when evaluating these patients.4
Presenting symptoms for IOWFB injury are variable. The literature describes a range of clinical complaints. One study described a series of nine patients with IOWFB, revealing common features of motility disturbance (five of the nine patients) as well conjunctival injection (again, five of the nine patients) with or without discharge. Less-common features included chronic drainage from an orbital fistula, decreased visual acuity and eyelid pain.5
 |
 |
The presence of a pyogenic granuloma in association with a deep-seated foreign body is rarely reported in the literature. In the orthopedic literature, there are a few cases detailing an association between recurrent pyogenic granuloma of the hand in association with an occult, retained foreign body.6 In the ophthalmic literature, pyogenic granulomas have been reported in association with irritating or misplaced silicone punctal plugs.7,8 Given the persistent, recurrent pyogenic granuloma presented in this case, the mass likely developed following a foreign body reaction to the wood.
The preferred imaging modality in patients with potential IOWFB injury is debated in the ophthalmic literature. A study by Wills Eye endorses computed tomography as the imaging modality of choice for identifying wood in the orbit. Bone windows are believed to be more effective than soft tissue windows at identifying IOWFB, as soft tissue windows—at their standard intensity of 200 to 350 Hounsfield units and level of 15 to 40 HU—are relatively inadequate to achieve wood resolution. Plain X-ray doesn’t offer ancillary information, as it can’t highlight wood. B-scan ultrasonography may or may not be helpful. The authors believed that magnetic resonance imaging could offer additional information to the CT scan as wood can appear hypointense relative to surrounding soft tissue and sometimes have ring-enhancing features on T-1 weighted imaging.4 Other authors have argued that both CT and MRI should be considered when evaluating a patient with a potential wooden foreign body injury.9-12
By nature of the varied mechanisms of injury that lead to wooden penetration of the orbit, there’s a high risk of intracranial penetration. Orbital bones can be fractured by high-velocity objects. Typically, wood acts as a low-velocity object that enters the orbit through the eyelid and is deflected by the globe, being directed towards the orbital apex. This location allows a port of entry for intracranial extension.1 The risk of intracranial penetration should be kept in mind, and patients should undergo appropriate brain imaging to rule out this potentially fatal complication.
Wood, unlike other inert foreign bodies that are well-tolerated by the body, can result in a significant inflammatory or infectious reaction.2,11 For this reason, management nearly always involves surgical removal, wide exploration and rinsing the site with anti-biotics. Penetrating orbital injuries have been reported to have an infection rate of up to 64 percent; therefore, antibiotic coverage is recommended, in conjunction with surgical removal.3 Some authorities recommend that clinicians use antibiotics with adequate blood-brain penetration, given the risk of intracranial penetration with a case involving an intraorbital wooden foreign body.1
Interestingly, empiric antifungal therapy is typically not recommended for IOWFB injuries, despite the presence of organic matter. This is due to the rarity of associated fungal infection and the relative toxicity of treatment regimens.4 The patient discussed in this case was noted to have several foci of fungi on the wood that was extracted from his inferior fornix. Surprisingly, despite the presence of an undetected piece of wood in the orbit for more than a year, the patient didn’t develop an infection. Given the patient’s well-healed incision and lack of infection at the postoperative follow-up visit, a course of antifungal therapy was deemed unnecessary.
In summary, intraorbitals wooden foreign body injury is a rare and difficult-to-detect trauma that requires a clinician to maintain a high degree of suspicion. A recurrent pyogenic granuloma may be a clue to a deep-seated foreign body, especially in the appropriate population. A combination of imaging, including a CT scan and/or MRI, should be used to exclude intracranial involvement, a potentially serious complication of these injuries. Management of IOWFB injury typically involves surgical extraction of the wood, exploration of the tissue, antibiotic rinsing of the site and postoperative local and systemic antibiotic coverage. REVIEW
1. Dunn IF, Kim DH, Rubin PA, Blinder R, Gates J, Golby AJ. Orbitocranial wooden foreign body. Neurosurgery 2009;65:2.
2. Kim YH, Kim H, Yoon E-S. Unrecognized intraorbital wooden foreign body. Archives of Craniofacial Surgery 2018;19:4:300-303.
3. Kazarian EL, Stokes NA, Flynn JT. The orbital puncture wound: Intracranial complications of a retained foreign body. J Pediatr Ophthalmol Strabismus 1980;17:4:247-50.
4. Shelsta HN, Bilyk JR, Rubin PAD, Penne RB, Carrasco JR. Wooden intraorbital foreign body injuries: Clinical characteristics and outcomes of 23 patients. Ophthalmic Plast Reconstr Surg 2010;26:4:238-244.
5. Liu D. Common denominators in retained orbital wooden foreign body. Ophthalmic Plastic & Reconstructive Surgery 2010;26:6:454-458.
6. Azzopardi EA, Xuereb CB, Iyer S. Pyogenic granuloma as a surrogate indicator of deep seated foreign bodies: A case report. Cases Journal 2009;5:2:7354.
7. Ababneh OH, Msallam MM. Bilateral simultaneous pyogenic granuloma after perforated punctal plug insertion. Ophthalmic Plastic and Reconstructive Surgery 2014;30:5.
8. Kim BM, Osmanovic SS, Edward DP. Pyogenic granulomas after silicone punctal plugs: A clinical and histopathologic study. American Journal of Ophthalmology 2005;139:4:678-684.
9. Gaeta AD, Giurazza F, Capobianco E, et al. Intraorbital wooden foreign body detected by computed tomography and magnetic resonance imaging. The Neuroradiology Journal 2016;30:1:88.
10. Li J, Zhou L-P, Jin J, Yuan H-F. Clinical diagnosis and treatment of intraorbital wooden foreign bodies. Chinese Journal of Traumatology 2016;19:6:322-325.
11. Boncoeur-Martel MP, Adenis JP, Rulfi JY, Robert PY, Dupuy JP, Maubon A. CT appearances of chronically retained wooden intraorbital foreign bodies. Neuroradiology 2001;43:2:165-168.
12. Green BF, Kraft SP, Carter KD, Buncic JR, Nerad JA, Armstrong D. Intraorbital wood. Detection by magnetic resonance imaging. Ophthalmology 1990;97:5:608-11.



