| ||
 |
|
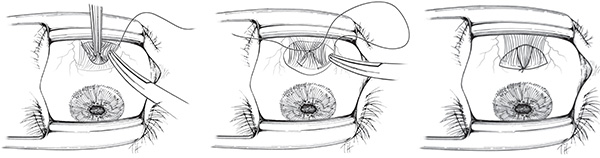
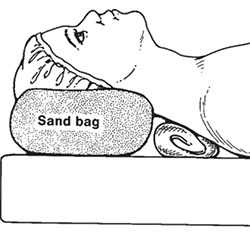
Proper head positioning really helps take the frustration out of strabismus surgery. Have the neck extended so the patient is looking at the surgeon sitting at the head of the surgical table. It is helpful to place a towel roll under the patient’s shoulders to get the chin up as shown in Figure 1.
 |
 |
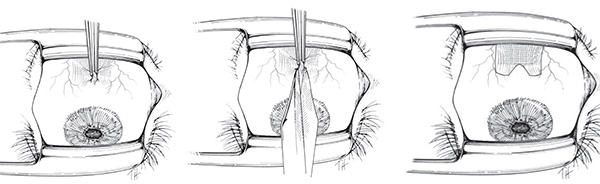
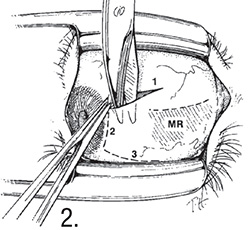
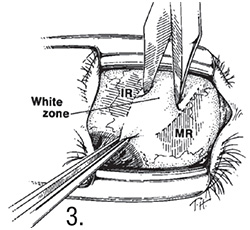
A proper conjunctival incision can make or break your strabismus surgery. The limbal incision is made at the limbus (See Figure 2) while the fornix incision is 7 to 8 mm posterior to the limbus in the inferior fornix (See Figure 3).
Basic rules:
A. Rectus surgery: limbal for older patients (over 40 to 45 years old) as the conjunctiva is friable.
B. Rectus surgery: fornix or limbal for patients under 40 years old.
C. Use fornix for inferior and superior oblique surgery.
A swan incision is the incision over the muscle insertion. This gives good exposure but can leave a conjunctival scar. That is why a fornix incision is preferred. If Swan is used, careful closure is required.
 |  |
 |
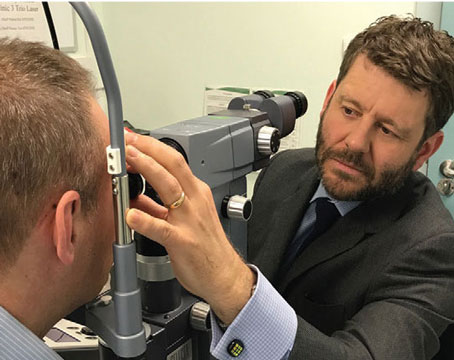
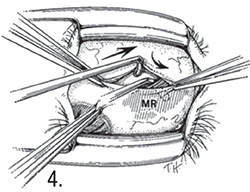
To hook a rectus muscle, place a small hook firmly on the sclera so the hook is straight up and down and perpendicular to the sclera. Then pass the hook under the rectus insertion, keeping the perpendicular orientation as much as possible until the hook is under the muscle (See Figure 4). Starting with hook perpendicular assures that you will not split the rectus muscle, as the muscle tip stays on the sclera. Replace the small hook with a large hook like a Jameson hook.
Be careful if the sclera is thinned. In these cases better to not push down on sclera but lay the hook flat on sclera.
 |
 |
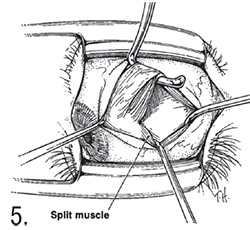
To ensure the entire rectus muscle is hooked, do the pole test. If the tip of the hook comes up and penetrates the muscle you will have a split muscle and residual fibers will be left behind. The pole test is used to ensure the entire muscle is hooked. Figure 5 shows the pole test in the case of a split muscle. Note that a small hook is placed at the tip of the larger Jameson hook holding the muscle. With the tip perpendicular to sclera, the small hook is pulled superoanteriorly. If the muscle is split, residual fibers not incorporated in the large hook will restrict the small hook from moving anterior to the insertion.
 |
 |
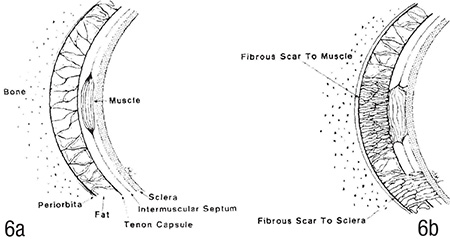
Posterior Tenon’s capsule separates orbital fat from the extraocular muscles and sclera (See Figure 6A). If during periocular surgery such as strabismus or plastic surgery one ruptures posterior Tenon’s capsule, fat will prolapse and scar to muscle and/or sclera. Over two to six weeks a scar attaches to the extraocular muscle and/or the sclera (See Figure 6B). The scar is an adhesion that contracts causing restriction of ocular rotations (i.e. restrictive strabismus). This is called fat adherence, first described by the late Marshall M. Parks, MD, (one of my teachers). There is no good treatment for fat adherence because removal of the scar is temporary, as the scar usually recurs. Figure 6A shows the normal anatomy with the posterior Tenon’s capsule separating orbital fat from the sclera and rectus muscle. Figure 6B shows fat adherence after posterior Tenon’s has been violated. Note the scar to muscle and sclera.
 |
 |
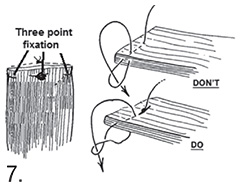
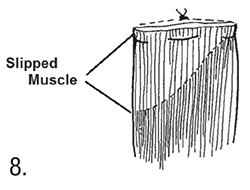
To secure an extraocular muscle, take a full-thickness central bite and then a full-thickness locking bite at each edge of the muscle for three-point fixation (See Figure 7). When suturing through the edge of the muscle, make sure you do a full-thickness pass. If a partial thickness pass is done, the unsecured muscle fibers will retract, resulting in a slipped muscle. Figure 8 shows a partially slipped muscle that occurred because the left muscle edge was not secured with a full-thickness bite.
 |  |
 |
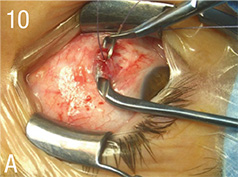
For rectus muscle recessions, replace the standard large hook (e.g., Jameson hook) with the Wright grooved hook, as seen in Figure 9. The Wright grooved hook allows for suturing the muscle insertion over the groove, thus preventing inadvertent scleral perforation. It also makes it easy to get full-thickness locking bites, and keeps suture placement consistent: not too posterior, not too anterior. It is very helpful when suturing tight muscles, as it pulls the muscle to the surgical field and provides a space to suture the muscle (See Figure 10A). It is also useful for suturing the inferior oblique muscle insertion while protecting the sclera in the area of the macula (See Figure 10B). (Dr. Wright holds a U.S. patent on the hook design.)
 |  |  |
 |
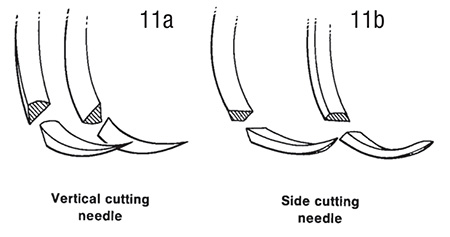
The sclera behind the rectus muscle insertion is extremely thin, only 0.3 mm. Because of the thin sclera, perforation into the globe is a significant risk during the scleral needle pass when suturing the muscle to sclera. The risk of perforation can be reduced by proper needle selection. The two basic types of needles are vertical cutting (See Figure 11A) and side cutting or spatulated (See Figure 11B). The preferred side cutting or spatulated needle has a flat top and bottom, thereby reducing the chance of inadvertent perforation deep into the globe or the roof of the scleral tunnel above. The vertical cutting needle, with the sharp pointed up or down, can either penetrate too deep or cut the roof of the scleral pass above.
 |
 |
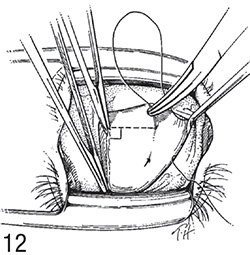
Because the sclera behind the muscle insertion is thin, less than the thickness of your needle, it is critical the scleral needle pass is shallow and controlled. Present the needle to the sclera with the needle tip up. This is analogous to how an airplane lands. The nose is up as the plane touches down to make sure the nose doses not plant into the tarmac. By keeping the needle tip up it prevents inadvertent perforation of the globe if the patient moves. Pass the needle horizontally, not up and down, as this will result in too deep or too thin a pass (See Figure 12). Pass like a barracuda swimming flat and straight, and avoid passing like a dolphin that swims up and down.
 |
 |
Over the past several years I’ve developed several minimally invasive procedures to correct small-angle strabismus. Here are two of those procedures: the Wright central tenotomy and the Wright central plication.
• Wright Central Tenotomy. The Wright central tenotomy causes a slight weakening of a rectus muscle by performing a tenotomy of the central 3 to 4 mm. The central tenotomy can be performed with topical anesthesia with the patient awake. This procedure is most useful to treat small vertical deviations between 2 to 3 prism diopters. A right hypertropia of 4 PD can be treated by performing a central tenotomy of the right superior rectus muscle. If there is a residual right hypertropia you can add a left inferior rectus central tenotomy. Because the procedure is done under topical anesthesia, we can check for a residual deviation and extend the tenotomy or as an additional muscle, if necessary.
|
• Wright Central Plication. I invented the full-tendon rectus plication procedure in the 1980s and first published the rectus plication procedure in 1991 calling it a modified rectus tuck. The modification involved suturing muscle to sclera, in contrast to a tuck, which sutures muscle to muscle. The standard muscle-to-muscle tuck relaxes over time and was therefore generally abandoned. A few years ago I developed a minimally invasive version of the plication called the Wright central plication, designed for small horizontal and vertical deviations. Instead of plicating the entire tendon, the central plication folds forward only the central 4 mm of muscle fibers. The Wright central plication is a tightening procedure that corrects 6 to 8 PD of strabismus.
|
To correct an esotropia of 7 PD in primary that increases in right gaze, perform a left lateral rectus central plication. It can be done with topical anesthesia with the patient awake or sedated. REVIEW
Acknowledgement: Drawings from Color Atlas of Strabismus, Springer Publishing, with permission from Kenneth W. Wright, MD.
Dr. Wright is the director of the Wright Foundation for Pediatric Ophthalmology & Strabismus and a clinical professor of ophthalmology at the Keck School of Medicine of USC. Contact him at 520 S. San Vicente Blvd., Los Angeles, Calif. 90048. Phone (310) 652-6420 or e-mail: wright2020md@aol.com.
1. Wright KW. Color Atlas of Strabismus. New York: Springer: 3rd ed. 2007, and 4th ed. 2015.
2. Wright KW. Wright Grooved Hook for Suturing Extraocular Muscle Insertion. Saudi J Ophthalmol 2010; 24:30-32.
3. Wright KW. Mini-tenotomy procedure to correct diplopia associated with small angle strabismus. Trans Am Ophthalmol Soc 2009;107:97-103.
4. Leenheer RS, Wright KW. Mini-plication to treat small-angle strabismus: A minimally invasive procedure. J AAPOS 2012;16(4):327-330.
5. Wright KW, Lanier AB. Effect of a modified rectus tuck on anterior segment circulation. J Pediatr Ophthalmol Strab 1991;28:77-81.
6. Park C, Min B, Wright KW. Effect of a modified rectus tuck on anterior ciliary artery perfusion. Korean J Ophthalmol 1991;5(1):15-25.