Despite the visual importance of the macula, ophthalmologists seldom focus on this region when looking for signs of early glaucoma. However, the work done by our group has demonstrated that early glaucomatous damage can and does occur in this area, and the most commonly used visual field test—the 24-2 test—misses most of this damage.
|
That area represents less than 2 percent of your retina, but it contains more than 30 percent of your ganglion cells. That’s where the action is, and that’s the area you want to preserve. (It’s worth noting that the thinness in the center is the result of all non-receptor cells being pushed to the side; the center area is packed with receptors, providing the detailed vision we experience at the fovea.) The points that are tested in the 24-2 test—not counting the one point that’s right in the center—miss this region of high ganglion cell density. Furthermore, even within the central ±8 degrees the 24-2 only tests four points.
Our research is now showing that considerable damage due to glaucoma can occur within the area bounded by those four points. This can be seen in Figure 1B, which shows the retinal ganglion cell damage (thinning) in this eye due to glaucoma. The fact that early damage can occur in this area means that in some patients the results of a 24-2 visual field test may appear normal or only reveal a couple of trouble spots—but if you did a finer test like the 10-2 visual field, you’d find clear abnormalities.
Why the Macula Is at Risk
Currently, the damage caused by glaucoma is generally presumed to begin at the optic disc, creating arcuate visual defects because of the way the ganglion cell fibers travel to the disc. Up until now, early glaucomatous damage in the macula has not been seen as an issue by many ophthalmologists. That’s partly because not everyone believes that early damage is likely to occur there; but equally important, the parts of the optic disc thought of as most vulnerable to glaucoma, where glaucomatous damage is generally believed to originate, are its superior and inferior quadrants. The fibers in those vulnerable quadrants were typically assumed to be associated with the classic arcuate defects seen clearly on the 24-2 test. (In fact, the 24-2 test was designed to pick up that kind of damage.)
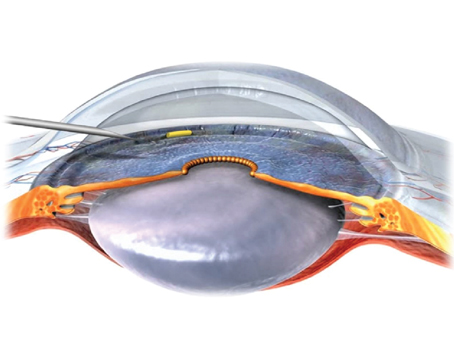
What our work has demonstrated is that large sections of the inferior macula—within the ±8 degree region—are, in fact, associated with fibers entering the optic disc in the vulnerable inferior quadrant, not in the relatively damage-immune temporal quad-rant that you would expect to be associated with the macula. This explains why macular damage from glaucoma should not be a surprise, and why it often appears as what my colleague Robert Ritch, MD, who first alerted me to this damage, refers to as a comma. They are just very tight arcuates close to fixation. (Also, the fact that the fibers in question originate in the inferior macula explains why these small macular defects tend to appear in the superior visual field, which of course is flipped relative to the physical location on the retina.)
In other words, the lower half of the macula is just as vulnerable to damage occurring in the inferior disc as we have traditionally assumed the inferior retina outside the macula to be. That means we need to be looking there for damage.
Some ophthalmologists perform the 10-2 if they notice a suspicious point on the 24-2, or if the patient has a vague complaint about having trouble seeing, or notes that his contrast is not as good as it used to be. But for many ophthalmologists, the 10-2 test is reserved for following advanced glaucoma cases, where the damage is so extensive that the 24-2 is largely useless and they’re trying to determine what vision is left. In fact, the 10-2 test is helpful when it’s used early in the disease. It can indeed reveal damage that would not be evident from a 24-2 test.
Adding OCT to the Mix
I’m a firm believer in scanning glaucoma suspects with OCT and com-paring the results to the patient’s visual fields. In my lab we routinely perform OCT and visual field tests on all patients suspected of having glaucoma or neuro-ophthalmological problems. Then, we com-pare the results.
The beauty of looking at them together is that they’re different kinds of tests that produce complementary data, with differ-ent kinds of variability and problems. One is a structural, anatomical test; the other is a behavioral/func-tional test. Also, if one test doesn’t produce useable data, the other probably will. Some patients, for example, have a hard time doing visual fields and produce variable results, but we can usually get a good OCT scans from those individuals.
|
For example, consider Figure 2. Here, the defect visible on the 10-2 printout (2A) is confirmed by the retinal ganglion cell thickness map from the OCT (2B, left panel), and the OCT retinal ganglion cell probability map (2C, left panel) confirms that this area is statistically abnormal. The same kind of comparison can also be done using the OCT measurements of the retinal nerve fiber layer (2B and 2C, right panels). This damage might have been missed, and certainly would have been underestimated, if the patient only took the 24-2 visual field test.
In some cases, having the two tests to compare elevates something that looks insignificant to something of concern. In a case like this, the visual field may only have a few marginally abnormal points and many doctors would not be concerned. The same might be true of the OCT by itself. But when both show damage in the same location, it suggests that there may indeed be a problem.
It wouldn’t be unreasonable to ask: Why not just scan these patients with the OCT? We’re currently doing a prospective study asking that question: If you just did the OCT, how often would you have to do a visual field to make the best diagnosis? There’s no question that in many cases you can make your diagnosis just using OCT. However, that strategy will not work 100 percent of the time. Furthermore, if you want to follow the patient, the functional measure—the visual field—is typically going to be closer to the patient’s complaint. For screening purposes you might be able to just use the OCT and save some time by not doing the visual field. But there is a point to doing both in the clinic, and many ophthalmologists are doing exactly that.
Despite the advantages of OCT, there are some serious concerns surrounding interpretation of the results. Most ophthalmologists are very busy; they just want to know: Is the result normal or abnormal? This is understandable, and the manufacturers are trying to respond to this need by developing reports that can make interpretation easier, highlighting more of the subtle information the scans contain. In the meantime, we can make sure that young ophthalmologists receive more training in how to read the scans. Also, most ophthalmologists should have someone they can rely on, as needed, to help interpret OCT scans. The reality is that OCT scans are just as complicated as MRI scans, and ophthalmologists would benefit from having the equivalent of a radiologist to help interpret them.
Points to Remember
With this information in mind, here are some strategies that will help enhance your ability to detect early glaucomatous damage:
• If your patient has any complaints of hazy vision or difficulty reading, or if you do a 24-2 visual field and find even one suspicious spot in the middle, perform a 10-2 visual field. The macula is often damaged in early glaucoma, and signs of this can easily be missed if you don’t run the 10-2 test. (In general, it would be even better to perform a visual field test that combines the best of the 24-2 and 10-2 test patterns.)
• Be aware that the macula can have diffuse damage. We now have clear OCT evidence for something that’s been in the literature for some time. In addition to the macula often having early local defects, the macula can also have very subtle but significant diffuse damage through-out. This damage is easy to miss. It’s visible on the 10-2 visual field, but clinicians often dismiss that evidence because it could be due to a small pupil or cataracts. For that reason, the best way to confirm it is with macular OCT.
• If you’re going to look at a circumpapillary retinal nerve fiber report, know which areas are most important. Scrutinize the region of the temporal portion of the inferior quadrant of the disc for local thinning. This is where you will find damage associated with small arcuate defects in the upper visual field of the macula. We call this relative small, about 35-degree region the macular vulnerability zone. Damage in that area will affect the macula and have a major impact on vision.
• With OCT, look at more than just the retinal nerve fiber layer profiles or the summary in-formation. Ophthalmologists often just look at the circumpapillary plot or some simple summary of the plot on the routine reports.
|
I wouldn't suggest replacing the 24-2 test with the 10-2 ... In fact, damage may first appear at either location. Sometimes a patient will produce a normal 24-2 and an abnormal 10-2; sometimes it will be the other way around. So you really need both types of information.
|
• When checking the circumpapillary plot, also check the underlying scan. Every manufacturer includes the scan on which the circumpapillary plot is based, although in some reports it’s too small to be of much use. The reason for looking at this scan is that it will tell you whether the circumpapillary information can be trusted. In particular, make sure that the machine’s software is accurately marking the edges of the retinal nerve fiber layer. If not, the circumpapillary information is flawed and you’ll need to redo the scan or hand-correct the lines placed by the algorithm.
• Realize that getting maximum information from OCT scans requires expertise. You can’t just look at the summary circles on these reports with their red or green regions and expect to find all the signs of damage that the scans might reveal to an experienced eye. To really take advantage of this technology, you should either devote some time and energy to learning to interpret the scans or find someone who has experience reading them that you can turn to for help when faced with a challenging case.
• When checking the circumpapillary plot, ask yourself whether it agrees with what you’re seeing on the visual field. There should be some agreement between them, especially if the damage is clear. If there’s any doubt, then go to the retinal ganglion cell thickness scan and superimpose it on the visual field to see whether there’s agreement.
Clinical Realities
Although ophthalmologists are increasingly adding OCT to their glaucoma work-ups, the idea of doing a second visual field test (the 10-2) is not always well-received. That’s not surprising, given the heavy patient load most ophthalmologists manage today; performing an extra visual field test takes extra time. I wouldn’t suggest replacing the 24-2 test with the 10-2; after all, damage can and does appear farther from the fovea. In fact, damage may first appear at either location. Sometimes a patient will produce a normal 24-2 and an abnormal 10-2; sometimes it will be the other way around. So, you really need both types of information.
The ideal solution would be to modify the 24-2 test pattern so that it has extra points in the center. At least one manufacturer has already done this; the Octopus machine from Haag-Streit has a test that includes those extra points. But most of the machines in clinical use are Zeiss machines. It isn’t that hard to modify the test, and I suspect Zeiss is working on making an alternative test pattern available.
In the meantime, you should at least be doing a 10-2 test if you have any concern whatsoever. And, if possible, use your OCT to enhance and confirm the information you gain from the visual fields. REVIEW
Dr. Hood is a professor of visual sciences in ophthalmology and James F. Bender Professor of Psychology at Columbia University in New York City.