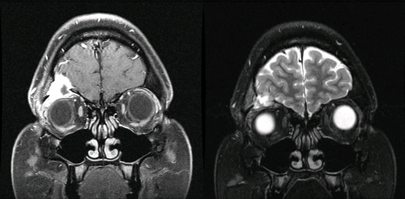
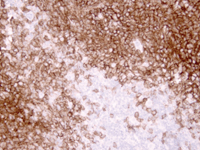
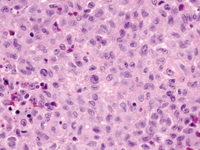
The patient underwent CT imaging of the orbits which revealed a mass in the right orbital roof with bony erosion. Further workup with MRI demonstrated a 2.4-cm aggressive enhancing lesion in the right orbit with extension to the right frontal calvarium and intracranial involvement with dural and epidural extension (See Figure 1). Neurosurgery was consulted and a collaborative neurosurgery-ophthalmology team completely resected the mass. Pathology of the tissue biopsy demonstrated proliferation of macrophages or dendritic cells, and positive staining with CD1a confirmed a diagnosis of Langerhans’ cell histiocytosis (See Figure 2).
Discussion
Langerhans’ cell histiocytosis (LCH), previously known as histiocytosis X, describes a rare spectrum of conditions with abnormal proliferation of histiocytes, occuring in various locations throughout the body. Three diagnoses historically fell under the classification of Langerhans’ cell histiocytosis, differentiated by the extent and the number of organ systems involved: eosinophilic granuloma (unifocal, uni-system disease); Hand-Schuller-Christian disease (multifocal, uni-system disease); and Letterer-Siwe disease (multifocal, multi-system disease), the last being the most severe, with a 50-percent five-year survival rate. Its underlying pathogenesis remains unclear, as it has been characterized as both a neoplastic and reactive inflammatory process. Several triggers have been posited in the literature, including viruses and minor trauma, but these remain controversial.1,2
| |||||||||||||||
Imaging with both CT and MRI allows for enhanced characterization of both the bony changes and soft tissue extension into the orbit and cranial fossae. Biopsy of the lesion is necessary to confirm the diagnosis as other orbital lesions in children, such as neuroblastoma, Ewing sarcoma and Wilms tumor, and other bony tumors may also present similarly on clinical exam and radiographic imaging. Positive immunohistological staining with neuronal markers S100 and CD1a are specific for Langerhans’ cells and help to confirm the diagnosis. Other tissue markers may also be positive, including adenosine triphosphatase, acid phosphatase, peanut lectin, alpha-mannosidase, CD207, fascin, CD4, CD45, CD101, HLA-DR, MHC Class II antigens and receptors for the Fc fragment of immunoglobulins.2 Birbeck granules, rod or racquet-shaped inclusion bodies seen on electron microscopy, are considered pathognomonic. However, the absence of Birbeck granules, which are present in 50 to 70 percent of cases, does not exclude a diagnosis of LCH.
Once the diagnosis is established by tissue biopsy, systemic evaluation is necessary for proper staging of the disease. This includes laboratory testing with complete blood count, comprehensive metabolic panel, coagulation studies, urine osmolality, and imaging with skeletal survey and CT or MRI to search for metastases. Our patient had an extensive workup that did not demonstrate any other concerning lesions or multi-system involvement. The usual treatment strategies for LCH include observation, biopsy with either subtotal or total curettage, intra-lesional steroid injections, systemic steroid therapy or chemotherapy. Excision and intra-lesional steroid injections can spare children from the adverse effects of chemotherapy, with systemic chemotherapy and systemic steroid therapy reserved for recurrent lesions or lesions that fail to respond to initial excision. REVIEW
The author would like to thank Edward Bedrossian, MD, Wills Eye Hospital Oculoplastics and Orbital Surgery Service, Ralph Eagle, MD, Wills Eye Pathology Service, and Brian Doyle, MD, for their time and assistance in preparing this report.
1. Maccheron LJ, McNab AA, Elder J, Selva D, Martin FJ, Clement CI, Sainani A, Sullivan TJ. Ocular adnexal Langerhans cell histiocytosis clinical features and management. Orbit 2006 Sep;25(3):169-77.
2. Harris GJ. Langerhans Cell Histiocytosis of the Orbit: A Need for Interdisciplinary Dialogue. Am J Ophth 2006; 141: 374-78.
3. Herwig MC, Wojno T, Zhang Q, Grossniklaus HE. Langerhans Cell Histiocytosis of the Orbit: Five Clinicopathologic Cases and Review of the Literature. Surv Ophthalmol 2013 Jul-Aug;58(4):330-40.