 |
The differential diagnosis in this patient with peripheral corneal
perforation and no history of trauma includes the spectrum of diseases
that cause peripheral ulcerative keratitis (PUK). These diseases
include infectious keratitis whether from bacteria, viruses, fungi,
Chlamydia and parasites, as well as Mooren’s ulceration. In this case,
given the significant history of joint aches and a likely
rheumatological illness, the differential diagnosis included rheumatoid
arthritis, Wegener’s granulomatosis, relapsing polychondritis, systemic
lupus erythematosus and polyarteritis nodosa.1
The patient had an extensive laboratory evaluation, which was notable for a mildly positive ANA 1:40, negative rheumatoid factor, negative ANCA and a CT angiogram of the chest, which showed no evidence of vasculitis. Based on the negative laboratory evaluation and the combination of PUK, saddle-nose deformity and large joint swelling, the patient was diagnosed with relapsing polychondritis.
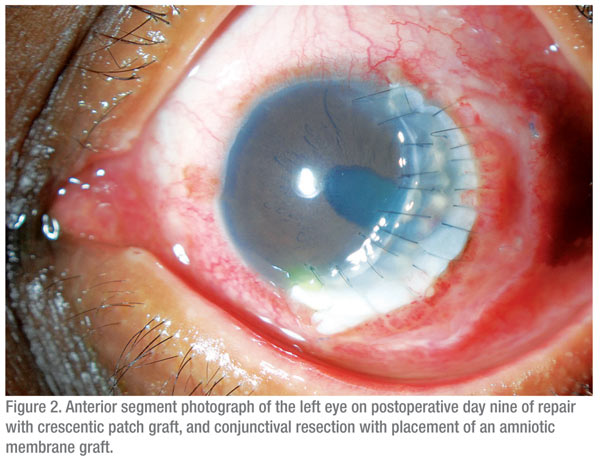
The treatment options for this patient included corneal gluing and bandage contact lens application, conjunctival or amniotic membrane Grafting, central keratoplasty or eccentric keratoplasty. Given the extent of the perforation and the remaining clear central cornea, an eccentric crescentic keratoplasty was chosen in addition to the resection of adjacent conjunctiva with placement of an amniotic membrane graft (See Figure 2). The patient tolerated the procedure well and postoperatively was started on moxifloxacin drops, erythromycin ointment and frequent artificial tears. The biopsied tissue showed evidence of chronic conjunctivitis with an infiltrate of lymphocytes and plasma cells and no evidence of infection. Given the progression of the patient’s disease on prednisone, methotrexate and infliximab, the patient was started on cyclophosphamide by his rheumatologist for additional systemic immunosuppression.
Discussion
PUK is a crescent-shaped, destructive, inflammatory lesion of the perilimbal cornea that is associated with an epithelial defect.1 The condition is usually associated with inflammation of the adjacent conjunctiva, episclera and sclera, which differentiates the lesion from noninflammatory lesions such as Terrien’s marginal degeneration. PUK can often be differentiated From a Mooren’s ulceration by the presence of scleral involvement, associated systemic findings and the lack of the characteristic overhanging corneal edge. PUK in the setting of systemic disease has a high rate of mortality, with one study demonstrating more than 50 percent mortality if left untreated.2 The treating ophthalmologist must work closely With a rheumatologist to determine the appropriate evaluation and treatment plan. Therapy usually begins with systemic corticosteroids with adjunctive immunosuppressive and cytotoxic agents including methotrexate and cyclophosphamide. In addition, the TNF-á antagonist infliximab has been reported to be effective in treating rheumatoid arthritis-associated PUK in a small case series.3
The patient had an extensive laboratory evaluation, which was notable for a mildly positive ANA 1:40, negative rheumatoid factor, negative ANCA and a CT angiogram of the chest, which showed no evidence of vasculitis. Based on the negative laboratory evaluation and the combination of PUK, saddle-nose deformity and large joint swelling, the patient was diagnosed with relapsing polychondritis.
The treatment options for this patient included corneal gluing and bandage contact lens application, conjunctival or amniotic membrane Grafting, central keratoplasty or eccentric keratoplasty. Given the extent of the perforation and the remaining clear central cornea, an eccentric crescentic keratoplasty was chosen in addition to the resection of adjacent conjunctiva with placement of an amniotic membrane graft (See Figure 2). The patient tolerated the procedure well and postoperatively was started on moxifloxacin drops, erythromycin ointment and frequent artificial tears. The biopsied tissue showed evidence of chronic conjunctivitis with an infiltrate of lymphocytes and plasma cells and no evidence of infection. Given the progression of the patient’s disease on prednisone, methotrexate and infliximab, the patient was started on cyclophosphamide by his rheumatologist for additional systemic immunosuppression.
Discussion
PUK is a crescent-shaped, destructive, inflammatory lesion of the perilimbal cornea that is associated with an epithelial defect.1 The condition is usually associated with inflammation of the adjacent conjunctiva, episclera and sclera, which differentiates the lesion from noninflammatory lesions such as Terrien’s marginal degeneration. PUK can often be differentiated From a Mooren’s ulceration by the presence of scleral involvement, associated systemic findings and the lack of the characteristic overhanging corneal edge. PUK in the setting of systemic disease has a high rate of mortality, with one study demonstrating more than 50 percent mortality if left untreated.2 The treating ophthalmologist must work closely With a rheumatologist to determine the appropriate evaluation and treatment plan. Therapy usually begins with systemic corticosteroids with adjunctive immunosuppressive and cytotoxic agents including methotrexate and cyclophosphamide. In addition, the TNF-á antagonist infliximab has been reported to be effective in treating rheumatoid arthritis-associated PUK in a small case series.3
Relapsing polychronditis is a rare autoimmune disorder that is
characterized by recurrent inflammation of the cartilaginous tissues
throughout the body.4 The disease primarily affects the ears, nose, eyes
and joints. The condition equally affects men and women and has an
average age of onset between 32 and 51 years. There are no specific
laboratory tests to establish the diagnosis. Ocular inflammation occurs
in 60 percent of patients, and marginal corneal ulceration or
sclerokeratitis is found in approximately 10 percent. As in this case,
most patients with relapsing polychondritis and severe PUK will require
cyclophosphamide to control their disease and therefore must be
aggressively managed by a rheumatologist.5
The peripheral cornea is predisposed to inflammatory reactions as a result of its distinct morphology and immunologic characteristics.4 The architecture of the limbus allows for the deposition of immune complexes which increase the recruitment of inflammatory cells and the liberation of collagenolytic and proteolytic enzymes. Serum antibodies to corneal epithelial antigens have been found in patients with immune-mediated PUK.
In contrast, cell-mediated toxicity may play a role in pathogenesis in ANCA-positive vasculitides. This complex sequence of immunologic dysregulation is still under investigation, but the final pathway of the immune system is the activation of specific keratolytic enzymes which melt the peripheral cornea.
The treatment of PUK-associated corneal perforation is focused on removing the inflamed tissue and restoring the integrity of the cornea. The crescentic patch graft offers an alternative to central keratoplasty for the repair of these peripheral perforations. The potential advantages include lower risk of graft rejection, lower risk of peripheral anterior synechiae and secondary glaucoma and improved visual acuity, given the preservation of the visual axis.6
The peripheral cornea is predisposed to inflammatory reactions as a result of its distinct morphology and immunologic characteristics.4 The architecture of the limbus allows for the deposition of immune complexes which increase the recruitment of inflammatory cells and the liberation of collagenolytic and proteolytic enzymes. Serum antibodies to corneal epithelial antigens have been found in patients with immune-mediated PUK.
In contrast, cell-mediated toxicity may play a role in pathogenesis in ANCA-positive vasculitides. This complex sequence of immunologic dysregulation is still under investigation, but the final pathway of the immune system is the activation of specific keratolytic enzymes which melt the peripheral cornea.
The treatment of PUK-associated corneal perforation is focused on removing the inflamed tissue and restoring the integrity of the cornea. The crescentic patch graft offers an alternative to central keratoplasty for the repair of these peripheral perforations. The potential advantages include lower risk of graft rejection, lower risk of peripheral anterior synechiae and secondary glaucoma and improved visual acuity, given the preservation of the visual axis.6
The author would like to thank Brad Feldman, MD, Wills Eye Institute Cornea Service.
1. Ladas JG, Mondino BJ. Systemic disorders associated with peripheral corneal ulceration. Curr Opin Ophthalmol 2000;11:468-71.
2. Foster CS, Forstot SL, Wilson LA. Mortality rate in rheumatoid arthritis patients developing necrotizing scleritis or peripheral ulcerative keratitis. Effects of systemic immunosuppression. Ophthalmology 1984;91:1253-63.
3. Thomas JW, Pflugfelder SC. Therapy of progressive rheumatoid arthritis-associated corneal ulceration with infliximab. Cornea 2005;24:742-4.
4. Messmer EM, Foster CS. Vasculitic peripheral ulcerative keratitis. Surv Ophthalmol 1999;43:379-96.
5. Hoang-Xaun T, Foster CS, Rice BA. Scleritis in relapsing polychondritis. Response to therapy. Ophthalmology 1990;97:892-8.
6. Parmar P, Salman A, Jesudasan CA. Visual outcome and corneal topography after eccentric “shaped” corneal grafts. Cornea 2009;28:379-84.



