According to Eric D. Donnenfeld, MD, Ophthalmic Consultants of Long Island, manual LRIs are as vibrant and important to optics and ophthalmology as they have ever been. “The reason for this is that, as patient expectations have increased, the management of residual astigmatism associated with cataract surgery has become of paramount importance,” he says. “The previous generation of LRIs were performed to debulk the patient’s astigmatism. The plan today is to eliminate astigmatism, so that we no longer do manual LRIs for high degrees of astigmatism. We have better technology now than we had in the past. Toric IOLs and excimer laser photoablation are our plan of action for most patients with moderate to severe astigmatism. When I’m performing cataract surgery on a patient who has 1.5 D or more of astigmatism, I feel very comfortable offering him or her a toric IOL, whether it be a monofocal lens, extended-depth-of-focus, or a multifocal or accommodating IOL.”
 |
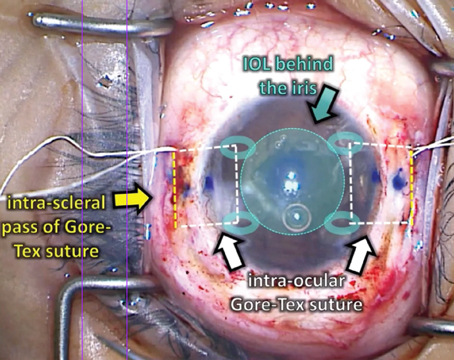
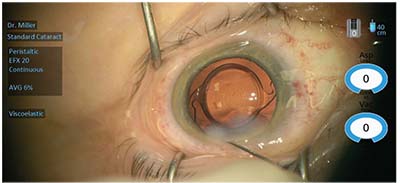
| Figure 1. (A) This patient suffered trauma, resulting in a white intumescent cataract, iris damage and posterior synechiae. A femtosecond laser phaco incision was placed in the steep corneal meridian to deal with astigmatism of less than 1 D. (B) The appearance of the eye after the surgery. |
However, when the cylinder drops down to 1 D or less, Dr. Donnenfeld feels that the advantages of a femtosecond laser are significant. “I like to combine the advantages of femtosecond laser technology with a femtosecond LRI so that the patient can have the perfect capsulotomy and the lens disassembled. However, postoperatively, I routinely continue to perform manual LRIs for patients who have residual astigmatism. The amount that’s tolerated has gone down dramatically as patient expectations have increased. We used to tolerate 1 D of residual astigmatism, but the current conventional wisdom is 0.5 D. However, I’ve seen many patients who will not even tolerate 0.5 D based on their visual expectations and the knowledge that, with a manual LRI, I can reduce the cylinder very commonly to 0.25 D or less,” he adds.
Small Amounts of Astigmatism
According to Kevin M. Miller, MD, from UCLA, “For high amounts of astigmatism, nobody argues the benefits of a toric lens over relaxing incisions,” he says. “But when you get down to smaller amounts, you can still make a compelling case for why you might want to do a relaxing incision instead of implanting a low-power toric lens. A benefit of toric lenses is that the power is going to be uniform from lens to lens, which is not always the case with LRIs. If you make the exact same incision in 100 different corneas, you’re going to get a spread of effect with 100 slightly different outcomes. So, the predictability of relaxing incisions is just not as good as with the torics. However, toric IOLs are not perfect, either.”
If the toric lens sits in the presumed effective lens position, then the toric power calculation is accurate. But if it sits a little anterior or posterior to the ELP, then its calculated power is not its effective power. So, there is variability of toric lens power based on vertex distance, but there is also variability of effect based on axis alignment. “If the lens is sitting exactly on the correct corneal axis, you get the full effect of the lens. However, if it’s 3 degrees, 5 degrees, or 10 degrees off of that, you start losing power, and you rotate the axis of residual astigmatism to some new location, which might be h
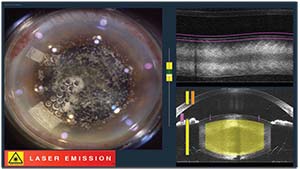 |
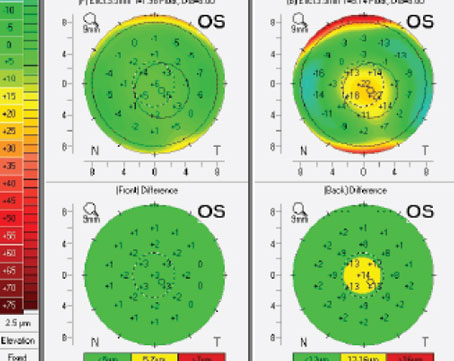
| Figure 2. An Alcon LenSx femtosecond laser in the process of making corneal incisions. The phaco incision was placed on the steep corneal axis in a superotemporal meridian to correct less than 1 D of corneal astigmatism. |
“As time has gone on, and as toric lenses have nibbled a larger portion of the astigmatism market away from incisions, I think we’ve seen a resurgence of incisions to touch up postoperative refractive errors,” he adds. “So, if a patient has mixed astigmatism, such that the spherical power of the eye is dead-on and the spherical power of the lens implant is good, but there is residual mixed astigmatism, either right after surgery, a couple of weeks later, a year later, or five years later, the surgeon can touch up those mixed astigmatisms with relaxing incisions and get a nice result.”
Dr. Donnenfeld says he’s performing increasing numbers of LRIs for smaller and smaller amounts of astigmatism. “The majority of LRIs that I perform today are for 0.5 D to 1 D of residual cylinder, with 0.5 to 0.75 D being my sweet spot,” he says. “I like doing my manual LRIs at the slit lamp because it’s an easier procedure for the patient. One incision is all that’s required, and I use a pre-set diamond knife at 600 µm depth with a curved interface that hits the cornea. This creates a deeper, more regular incision. So, for patients whose expectations have not been met and who have residual astigmatism, rather than bringing them back for an excimer laser ablation or a femtosecond LRI, these small amounts of cylinder are easily treated with manual LRIs. The visual rehabilitation is almost immediate, and for patients who are receiving a premium IOL, specifically multifocal and extended-depth-of-focus, the quality of vision and the added reading vision that’s obtained by reducing this 0.5 D or so of astigmatism can be very dramatic. It can turn a dissatisfied patient into a very grateful postoperative patient.”
Techniques
According to Dr. Miller, many surgeons believe that LRIs must be performed in pairs, one on each side of the cornea. That simply isn’t true, he says. “You can perform a relaxing incision on just one side of the cornea,” he notes. “Eighty percent of my astigmatism management at the time of cataract surgery is simply moving my phaco incision onto the steep axis. If a patient has 1 D or less of corneal cylinder, I will just place the phaco incision on the steep axis, and I can get that down to 0.5 D or so without a matching incision on the other side, and without a toric lens. So, 75 to 80 percent of my astigmatism management is still just a single relaxing incision instead of a pair of incisions. So, in a sense, it’s still the driving force of astigmatism management, at least for my practice, and I suspect that’s probably true for a lot of practices. This is especially true with the rise in popularity of femtosecond laser-assisted cataract surgery.”
However, Dr. Miller notes that many surgeons don’t feel comfortable moving their chair and microscope to operate on the steep axis. For example, some surgeons always like to sit on the temporal side of the cornea. “Then, they’ll use a toric lens and rotate it to whatever axis is necessary to nullify whatever the patient comes in with, plus whatever they’re inducing by making their temporal corneal incision. But, that’s going to cost the patient more money, and it’s going to mean more time calculating before the surgery,” he adds.
“I like relaxing incisions because they’re something that can correct small amounts of astigmatism. Relaxing incisions don’t rotate; when you make them on the right axis, they don’t rotate off that axis. Toric lenses sometimes will rotate off. So, for a lot of reasons, LRIs work, and they will remain one of my most important tools,” Dr. Miller concludes.
A Lost Art
According to Elizabeth Yeu, MD, who is in practice at Virginia Eye Consultants, “all cataract surgeons who are refractively minded should be offering astigmatic keratotomies without forgetting how useful manual LRIs actually are. It’s a skill and an art that, if we haven’t embraced it yet, we should be embracing. And there are several reasons for this. The most obvious one is that, for those patients who have astigmatism in the 1 D or lower range, it is a very nice way to predictably reduce the astig
 |
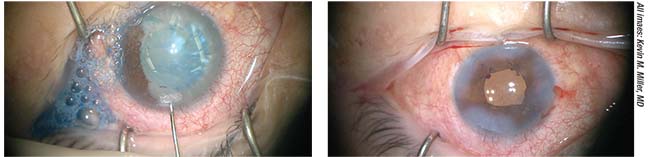
| Figure 3. This eye underwent standard femtosecond laser-assisted cataract surgery with implantation of a multifocal IOL. The phaco incision was placed superonasally in the steep corneal meridian. |
Dr. Yeu explains that the contribution of posterior corneal curvature affects the overall refractive corneal astigmatism. Specifically, she doesn’t offer these patients a toric IOL until she sees at least 1.4 D of anterior with-the-rule astigmatism, but preferentially offers a toric IOL to patients with any more than 0.70 D of anterior against-the-rule astigmatism.
“Lastly, in those cases where something happens intraoperatively that demonstrates that the patient should not be getting a toric IOL, but would instead be best served with an LRI, it’s important for surgeons to understand and be comfortable with manual LRIs,” she explains. “Such scenarios include a complex cataract procedure where the toric IOL could not be implanted, or if intraoperative aberrometry calls for a standard, non-toric monofocal IOL. This can really help to improve the outcome for the surgeon. So, there are many reasons why we should not forego the art form that is the manual LRI,” she explains.
Jeremy Z. Kieval, MD, from Lexington Eye Associates in Massachusetts, agrees. “I think being able to perform a manual LRI is a really important skill to have, no matter what other treatment options exist out there,” he says. “It’s a skill that all surgeons should have, especially for managing a patient’s residual astigmatism. For me, the place that I use manual LRIs the most is in the office. I have been transitioning from a procedure that I exclusively did in the operating room at the time of cataract surgery to a minor procedure that I can do in the office at the slit lamp to adjust the patient’s residual astigmatism that they may have after implantation of a toric lens or after a femtosecond limbal relaxing incision.”
Dr. Kieval believes that femtosecond lasers are probably the best choice for performing LRIs in most cases. “However, what if your laser goes down? It’s a nice skill to have to be able to go on with your day in the event that your laser isn’t working. Surgeons have been saying for the past 15 years that new surgeons aren’t learning how to do extracap surgery. Everybody knows how to do phaco, but extracapsular cataract extraction is a skill that comes in handy every once in a while. The same is true for being able to perform manual LRIs,” he says.
The Future
Dr. Donnenfeld believes that there will still be a role for manual LRIs for the foreseeable future. “The light-adjustable lens, which just got approved by the FDA, may reduce the need for manual LRIs in a subset of patients. For those patients who want to have a better result, and specifically for patients who don’t want to or can’t afford to pay a premium for cataract surgery, I routinely bundle manual LRIs into my procedure at no cost to the patient if I feel it’s in their best interest and if they aren’t in the position to pay out-of-pocket for a costly astigmatic procedure,” he says. REVIEW