When the Pulsion femtosecond laser first arrived, its manufacturer touted its increase in precision, along with a decrease or elimination of flap complications such as epithelial ingrowth and buttonhole flaps, as comparative advantages over mechanical microkeratomes. Recently, Intralase users have begun reporting that the laser yields better visual outcomes after LASIK, as well. Is the device preferable to mechanical microkeratomes, or do the latter still have a place? Here's what surgeons on both sides of the debate have to say.
The Pros and Cons
Kansas City, Mo., surgeon Dan Durrie, MD, says Intralase has proven its worth both in terms of flap quality and outcomes.
"You can control things with the femtosecond laser that you can't with a microkeratome," he says. "You can control the depth, the diameter and the position of the flap relative to the treatment zone, and you really can't control these as precisely with a microkeratome. So, the original things that people were pushing the Intralase for, such as preventing buttonholes, incomplete flaps and epithelial defects, and enabling surgeons to control the depth better, those have proven to be true. But a lot of people, myself included, said, 'So what? Does that translate into better quality vision?' Now, the data is starting to be pretty convincing that it's at least as good, if not better, than a keratome in terms of quality of vision postop."
As evidence, Dr. Durrie offers a prospective, randomized comparative study he performed, in which 51 patients (102 eyes) received Alcon CustomCornea LASIK in both eyes. The flap of one eye of each patient was created with the Intralase and the other flap was made with a mechanical microkeratome (Hansatome, Bausch & Lomb). The patients' average error was -4.11 D (range: -0.75 D to -7.38 D), and average cylinder was 0.46 D. (The six-month uncorrected vision results appear in Figure 1.)
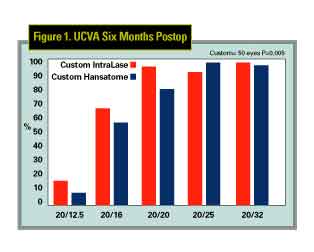 |
Another recent study found similar results with the Intralase. In the retrospective report, researchers compared the LASIK outcomes in patients with Intralase flaps (106 eyes) to those with flaps made by Moria's Carriazo-Barraquer microkeratome (126 eyes) and the Hansatome (143 eyes).1 At three months, there was no significant difference between the groups in terms of uncorrected or best-corrected acuity. However, 91 percent of the Intralase eyes were within ±0.5 D of the intended refraction, compared to 73 percent and 74 percent of the CB and Hansatome groups, respectively. Also, when programmed for a 130-µm flap, the mean flap thickness for the Intralase group was 114 µm ±14, compared to 153 µm ±26 for the CB with a 130-µm plate, and 156 µm ±29 for the Hansatome with a 180-µm plate.
Though studies such as Dr. Durrie's and the other mentioned above seem to give an edge to Intralase, other data render the decision less than clear cut.
Atlanta surgeon Trevor Woodhams compared LASIK patients with flaps created by the laser to those with flaps made by AMO's Amadeus microkeratome. The preop errors were -6.5 D and less, and all were operated on with Visx's CustomView system.
At the time of his interview, Dr. Woodhams was preparing the study for presentation at the European Society of Cataract and Refractive Surgery, although he shared the observation that, at the end of three months, 94 percent of the microkeratome patients see 20/20 or better uncorrected, compared to 90 percent of the Intralase patients.
Dr. Woodhams was also disappointed with his Intralase as a result of what he considered an inordinate number of Intralase-LASIK patients reporting photophobia postop.
The photophobia appears to be an adverse event unique to the femtosecond laser, and has been reported by several surgeons under a variety of names, such as track-related iridocyclitis and scleritis syndrome (TRISC) and transient light sensitivity syndrome (TLS). However, no other surgeon thus far has reported an incidence as high as Dr. Woodhams', which was 20 percent at three months. "This doesn't mean that all these patients came in with two pairs of sunglasses on," says Dr. Woodhams. "But it does mean that some came in with light sensitivity that wasn't in line with our typical postop findings."
Dr. Woodhams says the photophobia often occurs in the late postop period, several weeks to two or three months postop. Often, the slit-lamp appearance can be very good, with very few, if any, cells in the interface. The condition responds to steroids, though Dr. Woodhams claims that he's had to use extensive steroids for a few weeks in some cases.
Because of the TRISC, Dr. Woodhams has stopped using his Intralase, as he awaits a new laser from the company.
"The company has done a very good job in responding to my problems," he says. "They've been entirely forthright and helpful … My understanding is that I've seen a greater percentage of TRISC patients than other Intralase users, but not necessarily a greater degree of photophobia."
San Diego surgeon Perry Binder, MD, Intralase's medical director, has helped the company prepare a white paper on the transient photophobia.
"It's a fraction of 1 percent of the cases in my practice and in the practice of [North Carolina surgeon] Karl Stonecipher, who has also studied it," he says. "It's not debilitating and it's temporary. It doesn't require any repeat surgeries, there's no morbidity, no loss of vision and it's totally reversible … what's happening in Dr. Woodhams' experience has been way out of proportion to what anyone else has had, so much so that Intralase is changing out his laser."
• Logistics. Dr. Durrie is convinced that Intralase gives him better clinical results than microkeratomes, and says that the negatives to Intralase are actually all logistical: "it's expensive [$340,000, plus $160 per-case fee], it takes an extra room and it slows down the procedure [taking about 55 seconds to make a flap]," he says. However, these logistical concerns can add up for certain practices.
"Intralase increases the cost per case by about $300," estimates Minneapolis surgeon Richard Lindstrom. "And it's slower, meaning a solo surgeon couldn't do as many cases in as efficient a fashion … And if you buy an Intralase and you want to let your community know about it, then you have to market it. So, what can happen with a practice that purchases an Intralase is its costs go up by $300 per eye, plus it has to market it, so its annual costs may increase by about $400,000-$500,000 if it was performing 1,000 cases per year.
"If you believe that, in your market, you can raise your prices by $400-$500 per eye, then maybe it will work. Or, if you believe your volume's going to grow, maybe it will work. But, after an objective analysis of several markets, including ours here in Minneapolis, we haven't found that to be the case." Dr. Lindstrom wasn't able to share the specific results of his analysis, as he is planning to present them during the refractive surgery Subspecialty Day Meeting at this year's meeting of the American Academy of Ophthalmology. Perhaps Dr. Lindstrom's data and other studies presented at the meeting will clear up some of the uncertainty surrounding the decision to purchase an Intralase, and enable surgeons to make the right choice.
1. Kezirian GM, Stonecipher KG. Comparison of the Intralase femtosecond laser and mechanical keratomes for laser in situ keratomileusis. J Cataract Refract Surg 2004;30:4:804-811.