Researchers in England and Australia compared formula-specific and patient-specific methods of second-eye refinement in cataract surgery in two heterogenous datasets in order to produce more precise adjustment coefficients for improved refractive precision. Second-eye refinement is an attempt to account for inaccuracies in effective lens positioning prediction and other sources of error.
The retrospective study included 139 patients in Australia who underwent delayed sequential bilateral cataract surgery. The researchers derived adjustment coefficients for the Barrett Universal II, Hoffer Q, Holladay I and SRK/T formulas and applied them to the second eye’s IOL calculation. Patient-specific optimized IOL constants were also derived from the first-eye prediction error and applied to the second-eye calculations. To test the validity of the results, the same adjustments were applied to a 605-patient U.K. dataset.
Here are the Australian-derived adjustment coefficients based on prediction error:
• Barrett Universal II: 0.30
• Hoffer Q: 0.56
• Holladay I: 0.53
• SRK/T: 0.48
• Range: 0.30 to 0.56
When applied to the dataset from the United Kingdom, 68 to 72 percent of patients were within 0.5 D of the predicted postoperative refraction (PPOR).
The researchers found that second-eye refinement using either method improves the refractive target in the second eye with a statistically significant positive impact on mean absolute error. They recommend using formula-specific adjustment coefficients only if the first-eye prediction error is greater than 0.5 D and if interocular symmetry is present. They developed the following formula: Adjustment =
PPOR + (formula-specific adjustment coefficient x first-eye PE).
J Cataract Refract Surg 2019;45:1239-1245.
Turnbull A and Barrett G.
Safer Phaco Frequencies?
 |
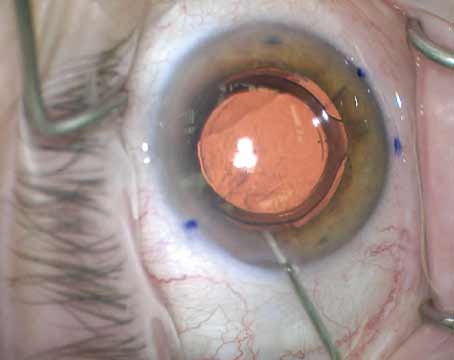
In a randomized, controlled trial in New Delhi, India, researchers grouped 160 eyes of 160 patients with grade 4.0 to 6.9 senile cataract into two groups, one receiving lower-frequency (28 kHz) phacoemulsification (Group A, n=80) and one receiving higher-frequency (42 kHz) phacoemulsification (Group B, n=80). A Megatron S3 phacoemulsification machine was used. Its handpiece functions were between 27 and 55 kHz. Effective phaco time and estimated fluid usage were compared intraoperatively, and endothelial parameters were assessed over one year.
The researchers found that the cataract cases performed in Group B had significant reductions in effective phacoemulsification time and estimated fluid usage compared to Group A. Over one year of follow-up, Group B also had significantly higher endothelial cell density. This difference in cell loss after one year was found to be statistically significant, and the researchers concluded that higher frequency ultrasound is more effective and safer than lower frequency for moderate to hard cataracts.
The researchers suggest that the more localized action of higher frequency phacoemulsification may help spare endothelial cells during cataract surgery. REVIEW
J Cataract Refract Surg 2019;45:1285-1293.
Dewan T, Malik PK, Kumari R.