"I have found wavefront laser vision correction to be a more powerful tool than I had anticipated," says David Shapiro, MD, who has a laser vision correction specialty practice in Ventura, Calif. "The performance of wavefront correction in complex cases has exceeded my expectations."
According to Dr. Shapiro, who performs LASIK or surface ablation with the Visx S4 IR, "When used with meticulous attention to detail, wavefront technology has become probably the single most important development in refractive surgery since the advent of the excimer laser."
More than LASIK
"Every new patient who walks through the door gets a wavefront analysis," says Perry S. Binder, MD, in practice in San Diego. He uses the Visx platform or the Wavelight Allegretto system depending on the patient.
  |
| Following an auto accident, this patient's right eye produced a normal wavefront (left) while the left eye was abnormal. David R. Hardten, MD |
Dr. Binder notes that wavefront technology also is indirectly a good detector of cataracts for a patient whose vision is not correctable to 20/20 and who has high-order aberrations.
He also finds the wavefront useful for dry-eye patients. Patients who are relatively dry with no previous surgery usually present with a high-order RMS that is two or three standard deviations greater than normal, he explains. After wavefront analysis, he determines the best treatment, such as punctal plugs, Restasis or lubricants. After treatment, he repeats the wavefront. "You can judge the improvement in the wavefront with the improvement in the tear film," Dr. Binder says.
Arturo Chayet, MD, in practice in Chula Vista, Calif., and Tijuana, Mexico, also performs a wavefront analysis routinely on new patients. He uses the Nidek Advanced Vision Excimer Laser System (NAVEX Quest).
"We do the Nidek OPD-Scan preoperatively on all of our patients," he explains. "Since we have acquired the wavefront-guided system, I have found we have a gained a better understanding of the human optical system, and as such, this technology allows for better surgical planning."
David R. Hardten, MD, in practice in Minneapolis, also finds wavefront technology more useful than he first anticipated. "In our practice we are mostly using wavefront technology for initial LVC treatments. The results are definitely better with wavefront than standard LVC, so we don't offer patients a choice of treatments. We use it for all patients for LVC where it makes sense," he explains. "We also use wavefront for treatment of patients with laser vision after IOL implantation, in analysis of patients with cataract (looking for high spherical aberration not present on topography), and for patients with unexplained vision complaints," explains Dr. Hardten, who uses the Visx platform.
He notes that wavefront technology aided in the treatment of a recent case with a 42-year-old patient involved in a motor vehicle accident. The patient had no direct eye trauma and no prior vision problems. However, the patient noted a decrease in vision in the left eye a few months after the motor vehicle accident, and a drop in BCVA to 20/25-2 (compared to 20/15 in the other eye, and 20/15 in this eye in the past).
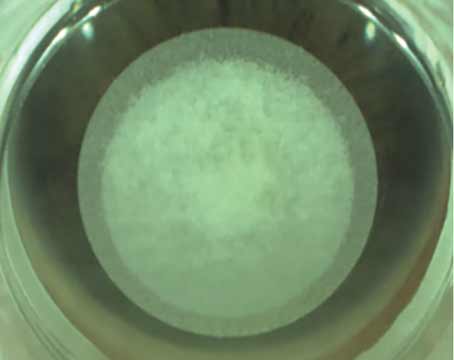
"The patient saw several doctors, including a neuro-ophthalmologist, and was sent to me for a wavefront to evaluate him for other issues," Dr. Hardten says. "There was an increased negativeness to the wavefront in the left eye. On careful exam, we observed that an oil droplet cataract was present (See Figures 1 and 2). The patient did well with cataract surgery."
This patient had complaints of dimness, imbalance, and wavy vision prior to surgery. "Many tests, including a visual field test, MRI, CT, Amsler and fluorescein, were all done before I saw him and were all negative. The wavefront really helped confirm the issue," he says.
Brian Boxer-Wachler, MD, in practice in Beverly Hills, Calif., uses the Alcon Custom Cornea wavefront system for his primary LASIK procedures. "This is definitely what we prefer over conventional LASIK," he explains. The system is so accurate at capturing wavefront aberrations. What we find is that even in corneas that have fairly significant aberrations, the system is able to stand up and capture them."
Dr. Boxer-Wachler also uses the wavefront in a variety of other ways. "We have found that for treating previous surgeries, it works exceedingly well. If someone had a previous LASIK, RK or PRK and had induced aberrations, it is great at helping to reduce those and make patients happy who were otherwise not very happy about their results," he says. "It also is a great diagnostic tool when we are seeing patients for second opinions because it can help explain what is going on behind the patient's symptoms, such as induced coma or spherical aberration."
Challenging Cases
The wavefront aids Dr. Shapiro in his treatment of difficult cases. For example, he used wavefront hyperopic LASIK to reduce higher order aberrations in an eye that had previously undergone RK and hyperopic shift (See Figure 3). "Typical of such cases, this post-RK cornea was a very complex, multifocal cornea with central flattening and a mid-peripheral knee. Wavefront technology, both from a diagnostic and therapeutic standpoint, was robust enough to handle this challenging surgical environment," he explains.
Fourier-based hyperopic wavefront LASIK (using Visx CustomVue) was able to correct the vision and also reduce higher-order aberrations. The reduced higher-order aberrations can be seen by comparing the pre- and post-LASIK Wavescans. The pre- and post-LASIK topographies confirm this improvement by showing reductions in the SRI value (a measurement of corneal irregularity) on the Tomey TMS System.
Dr. Shapiro notes that he has also had great success in other types of difficult, irregular corneas, such as cases with decentered laser ablations with loss of best corrected vision; previous small optical zone laser treatments with poor night vision; and even a cornea that had an irregular surface after undergoing removal of an epithelial neoplasm.
 |
 |
 |
 |
 |
 |
 |
 |
| Figure 3. Both eyes had previously undergone radial keratotomy and then developed consecutive hyperopia (hyperopic shift) over many years. The reduction in higher-order aberrations can be seen by comparing the pre- and post-LASIK Wavescans. A and B, and E and F represent OD and OS, preop, while B and C, G and H represent postop. The pre- and post-LASIK topographies confirm this improvement. David Shapiro, MD |
Other WF Applications
Karl G. Stonecipher, MD, in practice in Greensboro and Raleigh, N.C., uses the Visx S4 IR or the Wavelight Allegretto system. "For the therapeutic side, wavefront technology has been exceptionally helpful with the unhappy refractive patients, such as those patients with smaller optical zones from refractive surgery in 1990s and unhappy patients from the 1990s to early 2000s who received smaller astigmatic treatments," he explains.
These patients report that they are not seeing as well as they would like to, even though they may be 20/25. "Using wavefront, in some of these patients you can pick up higher-order aberrations that are extremely helpful in explaining to the patient the possible problem and the risks of an enhancement. Then, patients can have an enhancement with a custom treatment if they so desire," he says.
Dr. Stonecipher explains that he frequently does this type of treatment from the surface. "Older flaps are easy to lift," he says. "Often these are smaller flap diameters that we used with the anterior corneal shaper. Therefore, an 8- or 9-mm ablation in the periphery can not be done. I have found that removing the epithelium with alcohol is helpful to get a larger treatment zone. I then treat them on the surface and use mitomycin C for 12 seconds."
In addition, for some patients he uses the wavefront to help determine how much of an influence the lens has on the overall wavefront error. "In one map, the Nidek OPD allows me look at how much the cornea contributes and how much the lens contributes," say Dr. Stonecipher. After wavefront analysis, he counsels the patient based on the results, also considering age and other factors. He points out that some patients may be better served by a lensectomy.
|
Holistic Approach
"In our clinic we have changed our overall attitude on exams in the office. Because my main area is surgery, my exams were oriented towards preoperative screening exams or workup exams for surgery," says Daniel S. Durrie, MD, in practice in Overland Park, Kan.
"Now I have changed it to look at the eye to determine what is causing the problem as well as what is the general nutritional health of the eye," he explains. He then documents all information in the patient's electronic medical record. These records include information on the patient's retina, the lens, the topography, the wavefront, the tear film and the eyelids. "All of this affects my surgical outcomes," he adds.
Dr. Durrie also encourages post-surgical patients to return for a total exam of their eyes every couple of years. "Even if they go to their primary-care doctor, I still want to see them because refractive surgery is becoming a continuum," he says. For instance, congenital defects in patients' eyes are corrected when they are young, presbyopia is treated in their 40s, and eventually they have lens treatment. As new treatments are developed, these same patients may be eligible for upgrades within a category, he says.
Category upgrades include cases in which a surgeon may have corrected a patient's congenital defect in the 1990s and now can provide a wavefront-guided correction to upgrade his vision; or a patient who may have received conductive keratoplasty for presbyopia several years ago but who may now need a lens procedure because of advancing age.
This more holistic approach serves patients better, he believes. "It is a continuum of care so we, as surgeons, need to get the diagnostic equipment and the analysis into a continuum and record everything into our systems," he says. "Wavefront is a key to this. Then when patients return in a couple of years to check for the status of their visual systems, we can compare them to the last time they were in."