Nearly all patients (95 percent) treated with Lucentis maintained their vision in the Phase III clinical trials. Vision improved by at least three lines (or 15 letters) on the study eye chart in up to 40 percent of these patients at one year.
"Lucentis provides new hope for patients with wet AMD because it is the first therapy to provide a benefit in vision for a significant number of patients," said Arthur D. Levinson, PhD, Genentech's chairman and chief executive officer.
The approval is based on data from two large Phase III clinical trials (MARINA and ANCHOR). In these studies:
• Nearly all patients (approximately 95 percent) treated with Lucentis (0.5 mg) maintained (defined as the loss of less than 15 letters in visual acuity) and up to 40 percent improved (defined as the gain of 15 letters or more in visual acuity) vision at one year, as measured on the ETDRS chart.
• On average, patients treated with Lucentis in the MARINA study experienced an improvement from baseline of 6.6 letters at two years compared to a loss of 14.9 letters in the sham group. In the ANCHOR study, patients treated with Lucentis, on average, experienced an 11.3 letter gain from baseline at one year compared to a loss of 9.5 letters in the Visudyne photodynamic therapy control group.
• Up to 40 percent of patients treated with Lucentis achieved vision of 20/40 or better.
In addition to data from the two pivotal studies, data from the Phase I/II FOCUS and Phase IIIb PIER studies were included in the FDA review.
Lucentis 0.5 mg is recommended for intravitreal injection once a month. If monthly injections are not feasible, treatments can be reduced to one injection every three months after the first four monthly injections. Compared to continued monthly dosing, dosing every three months will lead to an approximate five-letter (one-line) loss of visual acuity benefit, on average, over the following nine months. Patients should be evaluated regularly.
In clinical trials, the most common adverse reactions among patients treated with Lucentis (reported in at least 6 percent more patients than in the control groups in at least one study) included conjunctival hemorrhage, eye pain, vitreous floaters, increased intraocular pressure and intraocular inflammation. Although there was a low rate (less than 4 percent) of arterial thromboembolic events (ATEs) observed in the Lucentis clinical trials that was not statistically different between the Lucentis and control groups, there is a theoretical risk of ATEs following intravitreal use of inhibitors of VEGF. Serious adverse events related to the injection procedure occurred in less than 0.1 percent of intravitreal injections, including endophthalmitis, retinal detachments and traumatic cataracts. Other serious ocular adverse events observed among Lucentis-treated patients (that occurred in less than 2 percent of patients) included intraocular inflammation and increased intraocular pressure. Lucentis is contraindicated in patients with hypersensitivity and ocular or periocular infections.
"In my opinion, the Lucentis approval stands out as one of the most important medical developments in ophthalmology during my 25 years in the field because it has the potential to reverse vision loss associated with wet AMD," said Eugene de Juan, MD, president of the American Society of Retina Specialists. "We are pleased that Lucentis has been approved by the FDA and look forward to working with Genentech to provide retina specialists in the United States with access to Lucentis for patients as quickly and smoothly as possible."
Lucentis was specifically developed for intraocular use in the eye to treat the underlying cause of wet AMD by targeting the molecular pathway that controls the formation of new blood vessels. Lucentis is designed to bind and inhibit VEGF-A, a protein that is believed to play a critical role in angiogenesis.
FDA Rejects IMT, Seeks More data
On July 14, the FDA's Ophthalmic Devices Advisory Panel, meeting for the first time in more than two years, recommended against approval of Vision Care Ophthalmic Technologies' Implantable Miniature Telescope.
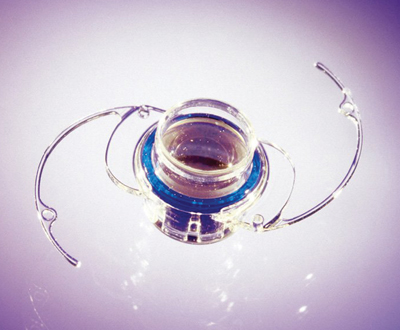
The IMT is intended for implantation in adults with stable, bilateral moderate to profound central vision impairment (20/80 to 20/800) due to age-related macular degeneration. The device, which contains two wide-angle microlenses that magnify the retinal image, is implanted in one eye of a patient to restore central vision, while the fellow, unimplanted eye provides peripheral vision. It is implanted in the capsular bag of the anterior chamber much like an intraocular lens, but its size requires a large, 12-mm incision.
Jeffrey Heier, MD, retina medical monitor for the trial, says the implant has several key advantages over external low-vision telescope devices, including a significantly wider field of vision, normal appearance and the ability to use natural eye movements. Two IMT patients testified during the FDA public hearing that the device had changed their lives, allowing them to see their grandchildren and resume activities that poor vision had forced them to give up previously, such as bike riding and painting.
Dr. Heier, R. Doyle Stulting, MD, and Stephen S. Lane, MD, who served as anterior segment medical monitor, presented data from a two-year clinical trial in which 206 patients received the IMT implant. The average age of patients was 75.4, with mean preoperative best-corrected distance acuity of 20/312.
The primary efficacy endpoint was an improvement in distance or near visual acuity of two lines or more in 50 percent of patients. Almost 90 percent of the patients met this goal, with more than 80 percent achieving a three-line or greater gain. Moreover, nearly 70 percent of patients gained two or more lines of both distance and near acuity. Investigators also reported gains on the NEI VFQ-25 test of 6 to 14 points, particularly among patients who gained lines of visual acuity. Patients with profound visual limitations preoperatively "achieved substantial and clinically relevant improvement in their vision and quality of life," Dr. Heier said.
Less than 2.5 percent of patients lost more than one line of BCDVA. However, a key safety target, endothelial cell loss of no more than 17 percent, was not met. Endothelial cell density (ECD) loss in the group as a whole was 28.2 percent at two years. ECD loss was greatest in patients with shallower anterior chambers.
Eight of the telescopes were explanted during the trial, due to device failure (two), patient dissatisfaction (four) or corneal decompensation (two).
Panelist and retinal specialist Neil M. Bressler, MD, made the motion for a vote of "not approvable," which passed by a 10-3 vote. Dr. Bressler said it was almost impossible for him to determine the efficacy of the device without a control group.
 |
| Makers of the Implantable Miniature Telescope will focus on gathering additional data for approval. |
Most of his colleagues on the panel, however, were primarily concerned about the rate of ECD loss. FDA reviewers extrapolated the chronic cell loss of 5.4 percent per year that occurred during months three to 24 out an additional two years. They predicted that more than one-fifth of the eyes would have mean ECD <1,000 cells/mm2 at year four, putting them at risk for corneal edema and decompensation. The predicted risk was higher for those who started off with relatively low ECD or shallower anterior chambers.
Following the vote, many panel members expressed regret that they could not find sufficient scientific evidence to support the IMT device at this time and urged the company to work with the FDA to provide additional data toward approval in the future. "We really do want this to work … we feel it has great potential," panel chair William D. Mathers, MD, said.
VisionCare Chairman and CEO Allen W. Hill said the company isn't giving up. "We look forward to working with the FDA to resolve any concerns they may have about the safety and efficacy of the IMT so that end-stage AMD patients with otherwise very limited options can gain access to this technology," he said.
Faster Allegretto Approved
In July, the FDA also approved WaveLight's 400-Hz Allegretto Wave Eye-Q laser for use in refractive surgery. This is not the same Eye-Q platform sold internationally as the Custom Q, which is only available outside the United States.
The Eye-Q was approved to use Allegretto's wavefront-optimized ablations to treat myopia of up to -12 D with up to -6 D of astigmatism and hyperopia up to +6 D with as much as 5 D of cylinder. The company says its wavefront-optimized profiles deliver ablations based on the eye's corneal asphericity in an effort to preserve the eye's natural shape. WaveLight says this helps enhance outcomes, especially in dim light.
In practice, the 400-Hz Eye-Q delivers 1 D of correction every two seconds at the 6.5-mm optical zone, which the company hopes makes for a more comfortable patient experience. WaveLight thinks the shorter procedure times possible with the faster laser will be particularly useful for time-intensive procedures such as high myopia and high astigmatism, and will enable practices to deal with large volumes of patients quicker than before.
Federal Legislation Seeks to Provide Kids with Vision Care
New legislation introduced last month aims to help eradicate untreated vision disorders among children. The American Academy of Ophthalmology says the "Vision Care for Kids Act," introduced by Sen. Christopher Bond, R-Mo., is both fiscally responsible and effective in providing critical vision care funding where it is needed most when children require follow-up care after a vision screening identifies a possible eye problem.
The AAO, American Association for Pediatric Ophthalmology and Strabismus (AAPOS) and other eye-care organizations helped create and strongly support the act, saying it complements individual state programs that identify vision problems in preschoolers. The act helps close the gap for kids who fail a vision screening who are not getting the follow-up diagnosis and treatment they need. It would provide state grants for eye examinations and additional treatment for uninsured children or those whose health plans do not cover vision service.
Two to 5 percent of children who fail a vision screening have significant eye problems, beyond those that can be fixed immediately with glasses. Many of these eye problems, if not treated early in life, can lead to permanent and irreversible visual loss. Yet, nearly 25 percent of parents whose children failed a vision screening did not schedule a follow-up comprehensive vision exam for their children because of a lack of financial resources.
This legislation also complements the Children's Healthy Vision Campaign, which promotes routine vision screenings by physicians and professionally trained screeners to identify children who need more comprehensive eye exams.



