LIKE THE OLYMPIC GAMES, THE TEAR FILM and Ocular Surface Society"s International Conference on the Lacrimal Gland, Tear Film, Ocular Surface and Dry Eye Syndromes is held just once every four years. It showcases the talent of the best and brightest in ocular surface and tear-film research. The most recent meeting was held last November in Fajardo, Puerto Rico. During the conference, more than 300 researchers from 24 countries contributed greatly to the current state of knowledge and understanding of the tear film and ocular surface. Here are some of the meeting"s highlights.
(Please note: All citations in the text are page numbers from The Ocular Surface, Supplement Conference Program & Abstract Book 2005;3:1)
Epidemiology: Who is at risk?
Large epidemiological studies on dry eye use symptoms to gain insight on the condition"s scale and risk factors. Schepens Eye Institute researcher Debra Schaumberg, ScD, presented data estimating that the prevalence of dry eye in people aged 50 or older in the United States is 7.8 percent for women and 4.8 percent for men. These large epidemiological studies suggest an increasing prevalence of the condition with age.
Data from the Women"s Health Study suggests a nearly 70-percent increased risk of dry eye associated with post-menopausal estrogen therapy and 30-percent higher risk for women taking estrogen plus progesterone therapy. Diabetes, use of sex steroid hormones and some other medication classes, and dietary intake of essential fatty acids currently appear to be some of the more well-known influences on the risk of dry eye. (Schaumberg D, S111)
Dry-eye epidemiology research has also been conducted overseas. Research from Japan indicated that the incidence of dry eye is 70 percent among that country"s elderly, a statistic that is higher than data presented for other areas of the world. (Tsubota K, S123) This result was corroborated by additional research that used a combination of tear-film breakup time, Schirmer"s test I, fluorescein staining and dry-eye symptomatology to assess the prevalence of dry eye in elderly Japanese. In this study, using the Japanese Dry Eye Diagnostic Criteria, 73.5 percent of the eyes had definite dry eyes. Meibomian gland disease was identified as a major risk factor for exacerbating dry-eye disease. (Dogru M, S58)
Researchers also performed epidemiological studies with a population of Ashkenazi Jewish participants. There is a relatively high prevalence (1:32) of altered function of the autonomic nervous system secondary to familial dysautonomia in this population. This study noted that many meibomian gland alterations were present and consistent across age and gender. Researchers hypothesized that this may be due to an altered autonomic nervous system in this particular population. Further research is necessary to identify whether evaporative dry eye is also a contributor. (Casavant J, S52)
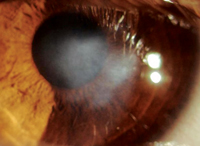
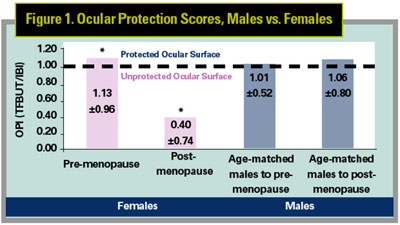
Another study analyzed the effect of menopause on the Ocular Protection Index (OPI) in a population of women with dry eye. The OPI quantifies the interaction of the time between blinks (inter-blink interval) and tear-film breakup time (TFBUT) in maintaining the integrity of the ocular surface. The ocular surface is tear-protected when the OPI score, the ratio of TFBUT/IBI, is greater than or equal to 1. In contrast, the ocular surface is unprotected when the OPI score is less than 1.
In this study, researchers evaluated the OPI in pre- and post-menopausal dry-eye patients and age-matched males with dry eye. In this population, post-menopausal women had a deficient OPI score (0.40 ±0.7) compared with pre-menopausal dry-eye patients (1.13 ±0.96) and age-matched male dry-eye patients (1.06 ±0.80) (See Figure 1). In addition, post-menopausal dry-eye sufferers exhibited an increased inter-blink interval (8.28 ±13.51 seconds) compared with pre-menopausal dry-eye patients (4.93 ±3.53 seconds) and age-matched males with dry eye (4.52 ±3.37 seconds). Researchers found that blink rate is decreased in post-menopausal patients, lengthening the IBI. These results suggest that, as has been established in the research of others, menopause has an effect on tear-film stability. (Wilcox K, S126)
 |
Research: Lipids, Mucins and More
The evaluation of gender-related differences in ocular disease and age-related differences in blink rate inspired researchers to focus on the effect of age and gender on the lipid layer of the tear film, incorporating both epidemiological and basic research to yield further information about dry-eye disorders.
One study used high-performance liquid chromatography to analyze the composition of the lipid layer of the tear film in adults with dry-eye symptoms and in normal infants, allowing for gender and age comparisons.
Researchers found 11 categories of lipids overall, and observed significant differences in certain types of these lipids. Notable variations included significantly lower phosphatidylcholine and significantly higher phosphatidylethanolamine in infants than in adults. Women had significantly higher free fatty acids and monoglycerides than female infants. Women were also significantly higher in triglycerides and significantly lower in cerebrosides and monoglycerides than men. The results of this research indicate that significant lipid differences are evident with relation to age and gender, and that they should be considered in further investigations of tear-film abnormalities. (McCulley J, S91)
- The impact of hormones.
The mucins tethered to the ocular surface cells perform a vital function by forming the foundation of the glycocalyx that anchors the tear film and facilitates uniform distribution of tears across the ocular surface. Three of these mucins, MUC1, -4 and -16 have been examined in order to determine their specific location on the ocular surface. Using sodium dodecyl (lauryl) sulfate-polyacrylamide gel electrophoresis, researchers found that MUC16 is concentrated primarily on the corneal epithelium, localized to the microplicae of the ocular surface cells, while MUC4 is mainly present on the conjunctival epithelium.
Though MUC16 is considered a membrane-bound mucin, it has also been identified floating free in the tear film. Research has documented "shedding" of the extracellular domain of these membrane-bound mucins. Further research will be necessary to determine when and why this occurs, particularly with regard to diseases such as Sjögren"s syndrome, in which changes seem to occur with membrane-bound MUC16. The researchers made it a point to recognize that, though a wealth of information is available, much about mucin functions and control of shedding and glycosylation remains to be discovered. (Gipson I, S66)
The types of mucin in the eye have been well-identified: MUC5AC and the shed domains of MUC4 in the tear film, and, as mentioned above, MUC1, -4, and -16 bound to the ocular surface. The plot thickens, however, when we consider that, even within one type of mucin, the structure, and thus the function, can be heterogeneous. Mucins contain highly glycosylated regions and long sequences of repeating amino acids, both of which are types of structures that can be highly changeable. Such variability in structure can translate to differences in function as well.
For example, researchers point out that, systemically, a specific "short" version of MUC1 is more commonly associated with gastritis, and such parallels may be evident with the mucins found in the eye--with certain populations having different environmental selective pressures resulting in greater expression of certain mucin alleles.
There is much more complexity in the picture when you consider that mucin genes are located near each other physically in the genome, so preferences towards one type of mucin may have a domino effect and initiate changes in the expression of other mucins. The concept certainly warrants further investigation, with the goal being individualized treatment for each patient"s specific case. (Swallow D, S118)
Drugs & Devices
Several presentations at the conference detailed cutting-edge research on dry-eye therapies in development.
- Artificial tears/cyclosporine.
In this study, the supportive therapies of Refresh Tears and Systane were both compatible with Restasis, and the Restasis/Systane group showed a statistical reduction in corneal staining compared to the Restasis/Refresh Tears group. Also, statistical differences were observed in favor of the Restasis/Systane group in patient-reported symptoms (ocular burning, stinging, grittiness, and dryness). These results indicate that the choice of artificial tears used as supportive therapy can yield differences in signs and symptoms of dry eye, and suggest that therapy with artificial tears should be further studied as a first-line therapy in the treatment of dry eye. (Christensen M, S54)
Research presented on cyclosporine 2% used alone indicated it was effective in phlyctenular keratoconjunctivitis and partially effective in vernal keratoconjunctivitis. (Doan, S57) Cyclosporine 0.4% also was effective in patients unresponsive to artificial tears, with severe immunologic-based dry eye, though significantly less effect was evident in those patients not having an immune basis to their condition. (Nepp S94)
Researchers tested the reproducibility and variability of measurements of tear-film osmolarity taken with this new device by testing tear samples taken from 28 individuals at three time points during an hour. Each reading was performed with at least 200 nL of tears measured with the OcuSense system by placing the sample onto a microelectrode tray.
The data indicated that significant differences between dry-eye patients and normals were discernable using this system, and it was 94-percent sensitive and 84-percent specific. This advancement in measurement of osmolarity to indicate dry eye is a great step forward in filling out the array of diagnostic tools available to the clinician and clinical researcher alike. (Sullivan B, S117)
As we look ahead, something to watch for is the final report from the Dry Eye Workshop (DEWS), a follow-up to the National Eye Institute/Industry Workshop on Clinical Trials in Dry Eye that was held immediately prior to the 2004 TFOS meeting. The group was composed of experts gathered to discuss the tear film, the ocular surface and symptoms in relation to dry eye. The final report from the DEWS meeting, based on much of the research presented at TFOS and other conferences, will present an improved definition and classification of dry eye, new diagnostic tools, and suggestions for future clinical trials. (Tsubota K, Lemp M, S123)
Clearly, the 2004 TFOS meeting yielded many fascinating insights and results that the dry-eye research community will use as a foundation to build upon, eventually amazing us with a new compilation of work after another four years. RO
Dr. Abelson, an associate clinical professor of ophthalmology at Harvard Medical School and senior clinical scientist at Schepens Eye Research Institute, consults in ophthalmic pharmaceuticals.
The ORA Dry Eye Department is directed by George W. Ousler III and managed by Katrina Wilcox Hagberg and Jason Casavant. Other members of the department who contributed to this article were Michael Schindelar and Andrew Workman.